What are furcation lesions?
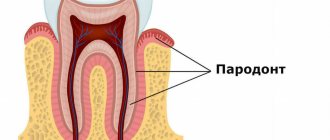
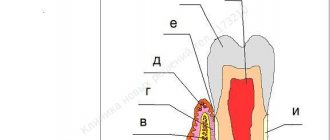
Furcation damage is the process of loss of bone tissue in the area of branching of the roots of the tooth. Typically, bone loss is a consequence of periodontal disease. Periodontium is a complex of tissues that surround and hold the tooth in the bone.
Almost all periodontal diseases are caused by the accumulation of plaque (plaque). Thus, high-quality and regular removal of plaque and stones is a mandatory, integral part of the course of treatment of periodontal diseases. As periodontal disease progresses, plaque and tartar begin to form on the root surface. In this case, the patient will no longer be able to independently remove microbial contamination. When the lesion reaches the furcation, self-cleaning becomes impossible.
Assessing furcation involvement The first step is to determine the presence and extent of furcation involvement. For this purpose, special (periodontal) curved probes are used, which are inserted by the doctor into the furcation area. The second step is to conduct an x-ray examination, which will help to visualize the existing defect.
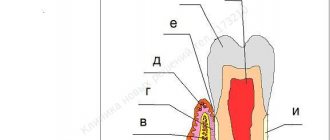
Classification of furcations depending on the severity of the lesion
Normal state of tooth furcation
Class 1 (initial changes) - on an x-ray, the affected area can be visualized as a groove
Class 2 (moderate damage) – the depth of the bone defect is 1-2 mm
Grade 3 - significant bone loss in the furcation area
Treatment Treatment of furcation lesions is a complex and painstaking task for both the doctor and the patient. Cleansing the furcation area is usually carried out using special scalers and currets. Drug therapy consists of taking or topical application of antimicrobial and antibacterial drugs. There are also surgical techniques for the treatment of furcation defects, which have two main goals: to make the furcation area more accessible for cleansing or to regenerate lost bone and soft tissue. The possibility of regeneration largely depends on the severity of the lesion; with significant defects, this procedure may not give positive results.
Prognosis The future of teeth with furcation defects of bone tissue is largely determined by how well the patient maintains oral hygiene and how regularly he visits the hygienist.
based on materials from the site www.deardoctor.com
Furcation defects - diagnostic basics
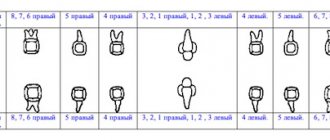
Molars of the upper jaw As a rule, the first molar of the upper jaw is in all respects - crown and individual roots - larger than the second molar, which in turn is larger than the third molar. The first and second molars most often have three roots: one mesiobuccal, one distobuccal, and one palatal. The mesiobuccal root is usually vertical, while the distobuccal and palatal roots are inclined. The distobuccal root projects distally, and the palatal root projects in the palatal direction (Figure below). The cross-sections of the distobuccal and palatal roots are usually circular. The palatal root is generally wider in the mesio-distal than in the bucco-palatal direction. The distal surface of the mesiobuccal root has a concavity that is about 0.3 mm in depth (Bower 1979a, b). This concavity gives the cross-section of the mesiobuccal root an “hourglass” configuration (Figure below). The three furcation entrances of the maxillary first and second molars vary in width and are located at different distances apical to the CEJ. Typically, the first molar has a shorter root shaft than the second molar. In the first molar, the mesial furcation entrance is located approximately 3 mm from the CEJ, while the buccal entrance is 3.5 mm and the distal entrance is approximately 5 mm apical to the CEJ (Abrams & Trachtenberg 1974; Rosenberg 1988). This means that the furcation vault is inclined; in the mesiodistal plane, the arch is relatively close to the CEJ on the mesial surface, but closer to the apex on the distal surface. The buccal furcation entrance is narrower than its distal and mesial counterparts. The degree of root separation and divergence decreases from the first to the second and from the second to the third maxillary molar. The mesiobuccal root of the first molar is often positioned more buccally in the arch than the distobuccal root. If the buccal bone plate is thin, the mesial buccal root often protrudes through the outer surface of the alveolar bone and bony fenestrations and/or dehiscence may occur. Maxillary premolars In approximately 40% of cases, maxillary first premolars have two roots, one buccal and one palatal, and therefore have a mesiodistal furcation. A concavity (about 0.5 mm in depth) is often present in the buccal root furcation. In many cases, the furcation is located in the middle or apical third of the root complex (Figure below). The average distance between the CEJ and the furcation entrance is approximately 8 mm. The width of the furcation entrance is about 0.7 mm. Molars of the mandible The first molar of the mandible is larger than the second molar, which in turn is larger than the third molar. In first and second molars, the root complex almost always includes two roots, one mesial and one distal. The mesial root is larger than the distal root. The mesial root has a predominantly vertical position, while the distal root projects distally. The mesial root is wider buccolingually and has a larger cross-sectional area than the distal root. The cross-section of the distal root is circular, while the mesial root is hourglass shaped. In addition, grooves and concavities are often found on the distal surface of the mesial root (Fig. below). The distal concavity of the mesial root is more pronounced than that of the distal root (Bower 1979a, b; Svärdström & Wennström 1988). The root shaft of the first molar is often shorter than the shaft of the second molar. The furcation entrances of the mandibular first molar, similar to those of the maxillary first molar, are located at different distances from the CEJ. Thus, the lingual inlet is often found more apical to the CEJ (>4 mm) than the buccal inlet (>3 mm). Thus, the furcation vault is inclined in the buccolingual direction. The buccal furcation inlet is often <0.75 mm wide, while the lingual inlet is generally >0.75 mm wide (Bower 1979a, b). The degree of separation and divergence between the roots decreases from the first to the third molar (Fig. below). It should also be noted that the buccal bone plate is thinner outside the roots of the first than of the second molar. Fenestration and dehiscence of bone tissue, as a result, are more common in the area of the first molar than in the area of the second. Other Teeth Furcations may also be present in teeth that usually have only one root. In fact, there may be double-rooted incisors (picture below), canines (picture below) and mandibular premolars. Sometimes there are three-rooted maxillary premolars (Fig. below) and three-rooted mandibular molars (Fig. below).
Periodontal regeneration: clinical approaches and opportunities
Source of the article: https://stomatologclub.ru/stati/parodontologiya-15/regeneraciya-parodonta-klinicheskie-podhody-i-vozmozhnosti-2922/#cut
Maximum preservation of one's own teeth is, in fact, a manifesto for all periodontists, and a goal that all dentists have been pursuing for many years. Technological improvements have made this goal more achievable than before, but even despite the possibilities of periodontal regeneration and reconstruction of the periodontal ligament, cementum, gums and alveolar bone, the problem of periodontal lesions has not been completely solved.
In June 2014, 52 international representatives, including clinicians, researchers and scientists, came together at an American Academy of Periodontology (AAP) workshop to collate all available evidence on periodontal regeneration. During the seminar, participants were able not only to discuss the mechanisms of biological reactions in the structure of the periodontium, and how these aspects can be used in practice, but also to identify prospects for further research. The AAP initiated the work of this congress with good reason: at that time in the United States, the prevalence of periodontal pathologies was critically high. Data obtained by the Centers for Disease Control and Prevention (CDC), which were collected for the period 2009-2012, indicate that almost 50% of the entire US population over the age of 30 years have some form of periodontal tissue damage, and 70% Americans aged 65 years and older suffer from destructive forms of periodontitis. Mild to moderate periodontitis has been reported among 38% of the US adult population. Preserving the integrity of the natural dentition while ensuring remission of periodontal disease is an extremely complex clinical task that goes beyond the usual correction of the parameters of aesthetics and function of the structural elements of the oral cavity.
A growing body of evidence suggests a link between periodontal pathology and systemic diseases of the body: for example, an association has been found between moderate-to-severe periodontitis and an increased risk of developing diabetes. Epidemiological evidence also suggests that periodontitis increases the risk of developing cardiovascular disease. Although the available data is still limited, scientists have already noted the possibility of a pathophysiological link between periodontitis and chronic obstructive pulmonary disease, pneumonia, chronic kidney disease, rheumatoid arthritis, cognitive impairment, obesity, metabolic syndrome and cancer. Regenerative methods for correcting periodontal disorders are not aimed at slowing down the progression of the disease, but at restoring existing defects in soft and hard tissues, protecting still intact dentition and preparing affected areas for further rehabilitation using implants. However, the inflammation associated with periodontitis can still be reduced during physiological tissue repair through natural biological mechanisms.
Types of regenerative periodontal intervention techniques
Many new emerging methods of regenerative periodontal interventions, including those that involve the use of delivery systems for certain cells, matrix scaffolds, bone anabolic agents and mesenchymal stem cells, are at an early preclinical stage of testing and require additional scientific research for their further implementation in the clinical setting. dental practice. Hard tissue augmentation procedures allow the restoration of bone tissue, periodontal ligament and root cement, which together provide stabilization of the tooth. Soft tissue augmentation procedures can stimulate the growth of new gums in the area of recession, improving the aesthetic appearance of the mucous membrane. The three most common types of periodontal iatrogenic interventions in clinical practice are bone augmentation, the use of biological agents, and guided tissue regeneration (GTR).
Bone grafting
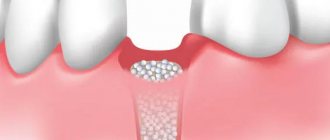
Bone grafting is one of the longest used techniques for regenerative iatrogenic interventions, which can use the patient’s own bone tissue (autograft), bone tissue from another patient (allograft), bone tissue from different animal species (xenotransplantate), or artificially synthesized bone tissue. tissue (alloplastic graft). Over time, the augment used is replaced by the patient's bone.
Guided tissue regeneration
Guided tissue regeneration procedure uses a barrier membrane to protect and stabilize the blood clot during the healing process of the bone graft area. Any interference with the structure of the blood clot during wound healing can cause disruption and the formation of scar tissue instead of new bone and ligament. The membranes used can be resorbable or non-resorbable. The former are ideal for interventions directly on the periodontium, while others work best during the reconstruction of the alveolar ridge and its preparation for future installation of implants. Resorbable membranes eliminate the need for repeated surgical interventions to remove them, which is very convenient for the patient. But at the same time, they must also be characterized by appropriate degradation parameters that will allow maintaining a sufficient amount of space for bone tissue to perform it. In cases where the main barrier function of the membrane may be compromised by anatomical features in the area of intervention, the physician must resort to an alternative method of treatment. So, instead of a membrane, you can use a bone graft, which is characterized by fairly rapid resorption. Membranes that resorb too slowly can impede blood flow to the regenerated structures and are more likely to become infected. As in any clinical situation, the clinician should use NTP only in clinical settings that are optimally suited for this type of intervention. In addition, to ensure the success of scientific and technological progress, the doctor must carry out precision decontamination of the tooth root in the area of the main surgical intervention. It should be noted that proper tooth root disinfection also requires special technical skills and relevant experience.
Biological products
Biological agents have demonstrated significant potential in the process of periodontal wound repair. Such drugs include growth factors, enamel matrix derivatives, and bone anabolic agents that stimulate cells to proliferate, migrate, biosynthesize, or differentiate the matrix. As a rule, most techniques for using biological products are in the early stages of testing, but some of them are already quite widely used in clinical practice. In the future, it is planned to carry out individualized periodontal interventions taking into account the genetic background of the patient, using biomarkers for prognosis, three-dimensional technologies for planning, and cell scaffolds as the main materials for transplantation.
Regenerative procedures for furcation defects and intraosseous defects
As a rule, patients requiring regenerative periodontal interventions are characterized by the presence of tissue defects in the furcation area and intraosseous defects. Classification of defects in the furcation area is carried out by assessing the level of loss of periodontal attachment in areas of “bifurcation” of the tooth roots. Clinicians are often faced with a choice: whether to remove such teeth or to try to restore tissue in the area of the existing defect.
The results obtained by Huynh-Ba and colleagues indicate that the NTR of the furcation defect region provides a high survival rate of treated teeth at the level of 83.3-100% during 5-12 years of monitoring. Intraosseous defects develop with internal periodontal damage to the alveolar ridge. Lang et al recommend assessing the morphology of the intraosseous defect by the number of affected bone walls.
The Goldman and Cohen (1958) classification suggests four classes of defects:
- with damage to three or four bone walls;
- with damage to two bone walls;
- with damage to one bone wall;
- combined defects (for example, with damage to walls 3 and 2, etc.).
The goal of periodontal therapy for any type of defect is the direct regeneration of periodontal tissue, including the apposition of new cement with the penetration of periodontal ligament fibers into it. Reynolds et al found that regenerative treatment of intraosseous periodontal defects increases clinical attachment levels, promotes periodontal pocket reduction, and improves overall periodontal health. The algorithm for the restoration of intraosseous defects, as a rule, involves bone augmentation using different types of grafts, but for the same purpose, methods of directed tissue regeneration and the principles of using biologically active agents can be used.
From theory to practice
Proceedings of the AAP Regeneration Workshop were published in the Journal of Periodontology and included consensus reports and systematic reviews on soft tissue restoration of root surfaces, furcation defects, and periodontal reconstruction. Accompanying practical recommendations were published in the journals Clinical Advances in Periodontics and the Journal of Periodontology, which formed the transition from theory to practice.
Treatments for gingival recession defects represent a key challenge to the potential for periodontal regeneration. Gingival recession is a fairly common condition, and the workshop participants agreed that the results of its correction should be assessed in terms of reducing the depth of the defect, improving the level of clinical attachment and the growth of keratinized soft tissues. In order to restore the coverage of the exposed tooth surface, you can use the techniques of a subepithelial connective tissue flap, a coronally displaced flap, a free gingival graft and its analogues, such as acellular dermal matrix, ketogenic collagen matrix and bioactive agents (recombinant growth factor obtained from platelets or derivatives of the enamel matrix) .
Richardson and colleagues Fr.
For situations that do not require root soft tissue restoration, John et al found that gingival augmentation procedures must be accompanied by patient education on oral hygiene and reduction of potential risk factors: “Understanding that minimal gingival attachment and suboptimal level of oral hygiene are determining clinical conditions - this is the first step towards objective diagnosis. Analysis of patient-specific factors helps to adequately approach the choice of surgical procedure aimed at increasing the parameters of keratinized tissues/attached gums.”
Reynolds et al summarized that the choice of the most effective method of treating intraosseous defects depends on a complete diagnosis and consideration of patient-associated risk factors. However, the authors also summarized that therapeutic approaches involving the use of combined treatment techniques are also quite successful. For example, acellular defect replacement grafts used in a guided tissue regeneration protocol help achieve proper stability of the augmentation site, protect the blood clot, and form new tissue. However, this approach, in fact, does not involve the use of biologically active agents. The choice of treatment method for intraosseous defects should involve the analysis of parameters such as the number of residual intact walls, loss of tissue height, proximity of the defect to other structures, and the possibility of achieving proper vascularization in the future.
Aichelmann-Reidy, when treating pathology in the furcation area, recommend taking into account systemic patient-associated factors, localized anatomical possibilities and characteristics of the furcation area itself. Class II furcation defects can generally be treated predictably using regenerative techniques, while Class I furcation defects can be repaired through a combination of bone augmentation and isolating membranes. Lin et al point out that modern technology is progressively facilitating the development of new periodontal regenerative treatments, and published clinical reports indicate even greater variability in current periodontal intervention techniques. However, one more problem remains - the lack of evidence base, but this aspect depends only on the time and results of the implementation of various approaches.
A systematic consensus report by Cochran et al on priorities for future research in new periodontal technologies can be summarized as follows:
- It is necessary to develop non-invasive methods for assessing the clinical results of regenerative periodontal interventions. This approach should also allow the effectiveness of new treatments to be assessed.
- It is necessary to validate those treatment methods that are used off-label, because some periodontal intervention techniques were originally developed for completely different purposes.
- To personalize treatment, it is necessary to provide an analysis of the patient's genetic and epigenetic profiles.
- To select a specific treatment method, it is necessary to evaluate the influence of pathogenesis, etiology and potential for regeneration in different forms of periodontal lesions.
- For more predictive treatment and restoration of periodontal structure and function, the physician must systematize all potential risk factors associated with iatrogenic intervention.
- The molecular and cellular mechanisms of each treatment modality need to be determined using in vitro and in vivo models.
- It is necessary to determine the paths of development of periodontal lesions to optimize the use of various methods of regenerative therapy.
- Researchers should focus on developing minimally invasive technologies to minimize postoperative pain and discomfort without compromising rehabilitation outcomes.
- There is a need to develop criteria to determine the clinical success of interventions.
- It is necessary to assess the impact of the chosen method of regenerative periodontal therapy on the patient’s quality of life.
Conclusion:
Regenerative therapy using soft and hard tissue grafts, biological agents, or guided tissue regeneration has a promising future in the periodontal field. A number of additional regenerative methods, including new cell delivery systems, are highly promising but require further scientific research to determine their effectiveness. The results of consensus workshops on periodontal regeneration indicate a strong evidence base confirming the effectiveness of reconstructive therapy for periodontal defects, allowing to restore not only the structure of soft and hard tissues, but also their full function. The use of regenerative periodontal interventions also helps preserve the patient's own teeth, which is one of the most important goals in periodontics.
Authors: William V. Giannobile, DDS, DMSc Pamela K. McClain, DDS
Diagnosis[edit]
The Nabers probe is used to clinically test for the presence of a furcation. [ citation needed
] Recently, computerized cone beam technology (CBCT) has also been used to detect furcation.
[5] Periapical and interproximal intraoral radiographs can help diagnose and locate the bifurcation. [ citation needed
]
Only multi-rooted teeth have branching. Therefore, the maxillary first premolar, maxillary and mandibular molars may be involved. The upper premolars consist of one buccal and one palatal root. Maxillary molars have three roots: mesiobuccal, distobuccal and palatine. Mandibular molars have one mesial and one distal root, etc.