Periodontitis is an inflammation of the vast majority of people
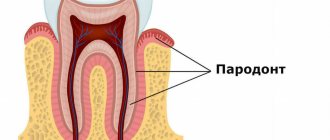
Periodontitis refers to inflammatory diseases that affect the gum tissue surrounding the tooth (periodontium), and is diagnosed to one degree or another in the vast majority of people. This is a progressive and very dangerous inflammation of the gums that destroys the tissue that supports the tooth.
If periodontitis is not treated in a timely manner, the risk of tooth loss increases many times over, so dentists never tire of warning patients that they should not delay seeing a doctor until the last minute.
At the initial stage, the symptoms of periodontitis are limited to bleeding and slight swelling of the gums, weakness of the dental ligament and discomfort when chewing, which for many people does not cause much concern. When the disease worsens, it is no longer possible to ignore the symptoms of periodontitis - severe inflammation of the gums, exposure of the neck of the teeth and purulent discharge from the periodontal pockets, pathological mobility and displacement of teeth, bad breath and enlarged local lymph nodes.
Periodontitis leads to heart disease
Periodontitis can lead to cardiovascular disease. We are talking about inflammation of the surrounding tooth tissues. This is an independent risk factor for the development of coronary heart disease, heart attacks and strokes.
Periodontitis can also cause cancer. Therefore, professional oral hygiene is needed, first of all, to prevent such violations.
Surgical methods for treating periodontal diseases
Inflammatory periodontal diseases are currently the most common diseases in the world. Any restoration, from a small filling to a complex implant bridge, can only be performed when the supporting periodontal structures are healthy and free of inflammation[1].
It is advisable to treat periodontal diseases in a comprehensive manner using general and local therapy. The surgical method in the complex treatment of the vast majority of periodontal diseases is a priority. It is carried out after conservative therapy and is aimed at eliminating local causes that support inflammation: removing dental plaque, including subgingival plaque. Curettage of granulations and deepitalization of the gingival pocket.
All periodontal interventions can be divided into two groups. The first group includes interventions aimed at eliminating periodontal pockets:
- Closed curettage of periodontal pocket.
- Open curettage of periodontal pocket.
- Gingivectomy.
- Flap operations.
- Apically displaced flap.
- Guided regeneration of periodontal tissues.
The second group includes interventions aimed at eliminating structural disorders of the soft tissues of the vestibule of the oral cavity, which not only aggravate the course of the inflammatory process in the periodontium, but in some cases are themselves the causes of its specific lesions. This:
- Plastic surgery of frenulum and cords (frenulotomy and frenulectomy).
- Vestibuloplasty.
- Operations to eliminate recessions. [2]
Curettage.
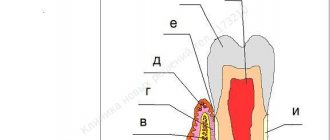
The purpose of curettage is to remove granulations, vegetative epithelium, decayed tissue, tartar, and damaged cement from the periodontal pocket. Scraping of the contents of the periodontal pocket is carried out with special instruments[3].
As a result of curettage, a clean wound surface should be obtained. Curettage is indicated in the presence of pockets no more than 4 mm deep, dense gums, and in the absence of bone pockets. For deeper pockets, preference is given to gingivotomy or gingivectomy, or one of the flap operations.
Curettage is contraindicated in the presence of acute inflammatory processes - abscesses, thinned and fibrously changed gums (regardless of the depth of the pocket), since the fibrously changed wall does not adhere well to the wall of the tooth. And also in the presence of bone pockets and tooth mobility of 3-4 degrees [4].
Gingivectomy.
Kinds:
- Simple.
- Radical.
- Partial.
Indications for simple gigivectomy are gingival pockets more than 4-5 mm deep with horizontal, uniform destruction of the alveolar bone; hypertrophic gingivitis; fibrous gum compaction; the need to lengthen the clinical crown of the tooth before orthopedic treatment; providing better support for the clamps of the rubber dam system, during patchwork operations, and with gingival fibromatosis.
Gingivectomy is contraindicated in the presence of deep bone pockets and a narrow zone of attached gum.
Flap operations.
Used to eliminate periodontal pockets, restore lost supporting tissue, i.e. formation of new connective tissue attachment and resumption of bone growth[5].
These surgical interventions are based on the Cieszynski-Widman-Neumann operation, which is performed when the pocket depth is more than 6 mm. The essence is to cut out and fold back the mucoperiosteal flap, followed by careful treatment of the roots of the teeth, bone pockets, and the inside of the flap. To date, several dozen modifications of this operation have been proposed. The advantage of these operations is the complete removal of pathologically altered tissues under visual control, ensuring longer-term stabilization of the periodontal process. The disadvantages are exposure of the necks of the teeth, some trauma, decreased alveolar process height, increased tooth mobility, dentin hypersthesia, and cosmetic defects[3].
Guided regeneration of periodontal tissues. (NRT)
The histological development of the root from the Hertwig epithelial sheath has been well studied. As in the case of embryonic development and healing of any other tissues, the process is regulated by genetically determined mediators. These include growth and differentiation factors, including bone morphogenetic proteins and special matrix proteins of the Hertwig epithelial sheath.
The classic NRT procedure involves installing a physical barrier (membrane), without the use of biological factors. A physical barrier placed in the desired location prevents apical epithelial proliferation or the formation of long junctional epithelium during defect healing.
All barrier materials are divided into the following groups:
- Synthetic non-resorbable.
- Synthetic resorbable.
- Naturally resorbable.
When using absorbable membranes, a second surgical intervention is not required. Therefore, such membranes are preferred in periodontics. There is a wide range of membranes on the market, none of which are universal and suitable for all cases. Directed regeneration requires sustainable materials[1].
An ideal membrane should have the following characteristics:
- Safety in terms of transmission of infections.
- Biocompatibility (lack of toxic and immunogenic properties).
- Easy adaptation to root and bone surfaces.
- Rigidity (the membrane should not sink into the bone defect).
- Permeable to some molecules, but not to cells.
- Immobility after integration into tissue.
- Long lasting stability to maintain tissue space.
- Controlled biological resorption.
- Additional antimicrobial and biostimulating properties.
Frenulotomy.
It is carried out with a shortened frenulum of the tongue by cutting it. It is advisable to perform this operation as early as possible - in infancy and childhood.
Frenulectomy.
It is performed when there is a short frenulum of the tongue or lip, as a result of which a diastema subsequently develops. Two semi-oval vertical incisions are made, excising the frenulum along with compact osteotomy. Having mobilized the mucous membrane along the edges of the wound, the latter is sutured tightly [6].
Vestibuloplasty.
It is carried out with a shallow vestibule of the oral cavity and involves moving the facial muscles attached to the crest of the alveolar process deep into the vestibule of the oral cavity.
Vestibuloplasty is used to create conditions for the anatomical retention of complete removable dentures, to restore the buffer function of the oral vestibule in case of periodontitis of the anterior teeth, in the case of a small vestibule of the oral cavity, as well as for endosseous implantation, when high muscle attachment to the alveolar process causes ischemia and inflammation of the gingival tissue. cuffs of functioning dental implants. Healing occurs by secondary intention or the wound is closed using free mucosal grafts[2].
Operations to eliminate recessions.
To date, the Muller classification is most often used: Class 1.
The recession does not reach the mucogingival border. 2nd Grade. The recession crosses the mucogingival boundary. 3rd Grade. Loss of attachment is also proximal (loss of gingival papillae) Class 4.
Proximal loss of attachment combined with tooth position abnormalities. Recessions 1 and 2 are eliminated surgically. For recessions of classes 3 and 4, only partial elimination is possible[7].
Before carrying out manipulations, it is necessary to eliminate factors that may be the causes of recessions. Currently, there are many modifications of surgical interventions to eliminate recessions:
- Coronal displacement flap.
- Laterally displaced flap technique.
- “Envelope” technique using a subepithelial palatal flap.
When performing interventions, it is desirable that the thickness of the mucoperiosteal flap in the intervention area be at least 1.5 mm.
The success of surgical treatment of periodontitis depends on a set of measures, including conservative therapy and adequate orthopedic treatment.
Literature:
- Wolf G.F., Rateitskhak E.M., Rateitshak K. “Periodontology”, 2008, “MED-press-inform”, Moscow
- Grudyanov A.I., Erokhin A.I. “Surgical methods for the treatment of periodontal diseases”, 2006, “Medical Information Agency”, Moscow
- Tsepov L.M., Nikolaev A.I. “Diagnostics and treatment of periodontal diseases”, 2002, “MED-press-inform”, Moscow
- Ivanov V.S. “Periodontal diseases”, 1998, “Medical Information Agency”, Moscow
- Borovsky E.V., Ivanov V.S., Vagner V.D. “Therapeutic Dentistry”, 2004, “Medical Information Agency”, Moscow
- Robustova T.G., Romacheva I.F., Afanasyev V.V., 1996, “Medicine”, Moscow
- Müller H.-P. “Parodontology”, 2004, “GalDent”, Lviv
Symptoms of periodontitis
To external reasons
The occurrence of periodontitis can be attributed to the presence of tartar, irregular tooth brushing and microtrauma.
Internal causes of periodontitis
deterioration in the nutrition of periodontal tissues, endocrine disorders, blood diseases, and hypovitaminosis are considered.
To the symptoms of periodontitis
include bleeding gums, loose teeth, discomfort when chewing. At a later stage, the neck of the tooth is exposed, the lymph nodes swell and bad breath appears. All this can lead to complete tooth loss.
Why is curettage needed?
The process of development of periodontitis is slow and occurs in a certain sequence. First, due to poor oral hygiene, the active proliferation of microorganisms begins, which in the process of their vital activity release a large number of toxins. These toxins have a negative effect on the gums and cause inflammation.
If the patient does not seek medical help at this stage, the inflammation gradually leads to the detachment of the gum from the tooth and the formation of periodontal pockets. These pockets contain food debris and soft dental deposits, which over time mineralize and become hard. Ideal conditions are created for the proliferation of microorganisms that affect not only the gums, but also the bone structures. As a result, granulation tissue is formed, which contributes to the rapid destruction of bone and loosening of teeth. If it is not completely removed, periodontitis will progress further, leading to more severe consequences. In order to effectively clean periodontal pockets from dental plaque, hard deposits and granulations, curettage is used.
Causes of periodontitis
The causes of the disease can be both general and local: in the first case, periodontitis develops against a background of weakened immunity, diabetes, blood diseases and various chronic diseases, and local causes include infections and injuries.
Microbes that produce toxins first affect the mucous membrane of the gums (gingivitis), and then penetrate into the deeper layers of tissue, destroying the supporting apparatus of the tooth.
Traumatic periodontitis occurs due to microtraumas (one-time or permanent) - to prevent it, it is recommended to avoid any mechanical impact on the gums.
During a visit to the dentist, the condition of the oral cavity is not only assessed and the origin of periodontitis is determined, but the depth of the gingival sulcus is also measured, which allows us to judge the stage of this disease. For example, if the depth of periodontal pockets does not exceed 3.5 mm, and there are no pronounced signs of exacerbation, then mild chronic periodontitis is diagnosed.
How to treat?
The treatment method will depend on the nature of the disease itself. For catarrhal form, rinsing with antiseptic and anti-inflammatory solutions and herbal decoctions is sufficient. Chamomile, sage or calendula work best. For best results, it is recommended to rinse the area under the hood.
Treatment of the purulent form is more complex. Antibiotics, angihistamines and anti-inflammatory drugs are prescribed. Surgical treatment has 2 options:
- Removal of a tooth;
- Excision of the mucous hood.
The first option is more drastic, but it allows you to completely get rid of the cause. Excision of the hood is used for correct but difficult tooth eruption. An incision is made under local anesthesia, the cavity is washed and drainage is installed. After surgery, the patient is prescribed antiseptic rinses.
Chronic pericoronitis is treated only by tooth extraction.
The use of a laser provides a good therapeutic effect. The affected area is exposed to infrared radiation, which penetrates deep into the tissue. To completely eliminate all signs, it is recommended to carry out 7-10 daily procedures. The result of treatment will be a reduction in inflammation and swelling.
Of course, treatment can begin at home. Rinsing will relieve acute symptoms, but will not get rid of the main cause of the condition - the tooth. Self-administration of antibiotics will also alleviate the condition, but only a doctor can prescribe the correct dose and regimen.
Diagnosis of periodontitis
Diagnosis begins with a consultation with a general dentist or periodontist. The doctor examines the oral cavity and prescribes additional examination, which may include the following methods:
- X-rays of the jaws. This basic examination provides general information about the condition of the teeth and bone tissue.
- Rheoparodontography. This method is used to determine the condition of the vessels of periodontal tissues.
- Ultrasonic osteometry. The study shows bone density.
- Schiller-Pisarev test. It involves staining the mucous membrane with a special solution that reveals foci of inflammation.
- Microbiological culture from the oral cavity. Allows you to determine the composition of microorganisms and their sensitivity to antibacterial drugs.
- Determination of periodontal index and bleeding index.
A comprehensive examination allows you to determine the degree of periodontitis, identify concomitant diseases and complications, and based on this information, plan further treatment.
Where to contact?
Modern treatment methods used in the CELT clinic can significantly slow down the development of the disease, and often stop it for a long period. Our experts recommend regular dental examinations, which allow you to identify the disease at an early stage, but even if the disease is advanced, we will do everything to stop it.
Surgical methods for the treatment of periodontitis are selected by our specialists based on diagnostic studies and examination of the patient. Our specialist will explain the current situation to you and tell you about the treatment methods that will be optimal in your case. He will provide full information about their advantages and disadvantages, calculate the cost of treatment and answer any questions you may have.
Make an appointment through the application or by calling +7 +7 We work every day:
- Monday—Friday: 8.00—20.00
- Saturday: 8.00–18.00
- Sunday is a day off
The nearest metro and MCC stations to the clinic:
- Highway of Enthusiasts or Perovo
- Partisan
- Enthusiast Highway
Driving directions
Causes of gum recession
Quite often, gum recession is one of the manifestations of periodontitis (periodontal disease). In this case, as a result of poor circulation in this area, gum atrophy and exposure of the tooth root occurs.
As a rule, this condition is diagnosed in middle and older age, although there are exceptions - for example, juvenile periodontitis.
Gum recession due to periodontitis
Chronic mechanical trauma to the gums - for example, from an overhanging edge of an artificial crown or filling, which happens very often, trauma from a removable denture or its fixing element - a clasp, which, due to the rapid development of implantology, is much less common today. The presence of tartar is also a risk factor for the development of gum recession.
Chronic gum trauma with wide crowns
Acute trauma to a tooth, leading to its displacement towards the lip or cheek.
Acute trauma – tooth dislocation
Anatomical features of the structure of the alveolar process - a thin layer of cortical bone located on the anterior surface of the alveolar process or the so-called “thin gum biotype”.
In the latter case, the problem is not the thickness of the bone, but rather the thickness of the gum covering the bone along the anterior (vestibular) surface. However, in both cases, the problem is associated with insufficient blood supply to the area.
Gingival recession as a consequence of thin biotype
Incorrect (low on the upper jaw or, conversely, high on the lower jaw) location of the frenulum of the lip or frenulum of the tongue.
Gingival recession of the lower incisor due to a labial frenulum
If in the case of a lip frenulum, the recession will be located on the front surface of the tooth root, then in the case of a lingual frenulum, the posterior (lingual wall) of the tooth will be exposed.
Another cause of gum recession can be orthodontic treatment, which can result in thinning of the vestibular bone.
And, of course, oral hygiene can also cause recessions and wedge-shaped defects. Moreover, oddly enough, too thorough brushing of teeth is not at all a good thing, because as a result of excessive mechanical action, both the gums and teeth suffer, in the cervical area of which wedge-shaped defects are formed, which we wrote about above.