A newborn baby is a big responsibility for young parents. When visiting a pediatrician, parents usually ask a lot of questions. Especially if the child is the first. In my personal top list, feeding and colic take first place. Second - rashes!
In photographs on social networks, babies have clean, rosy cheeks and an angelic smile. And in life, redness, pimples, peeling and other unexpected things appear on the skin. Moms are not ready for this. They get scared and start looking for the reason. Neighbors advise you to follow a diet, grandmothers complain about “bad milk.” If you are unlucky, the doctor will scare you with allergies or prescribe tests, half of which will turn out to be unnecessary.
Let's try to figure out which skin problems in infants do not require treatment and are normal in infancy, and which do not. Let’s agree right away: any rash should be examined by a doctor in person. A diagnosis cannot be made from a photograph, because the doctor examines the elements of the rash, touches it by touch, and sometimes special diagnostic tests are needed. In doubtful cases, the pediatrician gives a referral to a dermatologist.
The information below is given so that young mothers stop being afraid of every pimple, understand conditions that do not require medical attention, and understand when to take their child to the pediatrician.
What does a newborn look like?
If the birth goes well, immediately after the birth of the newborn baby, the mother is placed on her stomach. His skin can be bright pink, or it can be pale, his hands and feet have a bluish tint. This scares young mothers if they have heard or read something about hypoxia and cyanosis before. But if the doctors in the delivery room are calm and do not provide resuscitation measures, then this is a variant of the norm. A healthy child can be like this in the first minutes of life. In addition, the newborn's body is covered with vernix - the baby looks as if it has been smeared with cream cheese. And this is also normal, although unattractive. Lubricant plays an important role in protecting the skin from germs, so the baby’s skin is only lightly blotted without being completely wiped.
5-10 minutes after birth, the newborn’s skin becomes bright pink, almost red. This is a normal condition - physiological erythema . The air pressure is less than the pressure of the fluid in which the baby was in utero. When the skin ceases to experience resistance, blood actively flows to it. The body gets used to the new form of life. Gradually, the blood vessels will narrow, and the skin will become its usual pink color by the end of the week in full-term babies and after 2-3 weeks in premature babies.
How a newborn changes
The baby is born, and we expect him to look like the beautiful and pink babies in the advertising pictures. And it is somehow red, then suddenly turns yellow, there is either a rash or peeling on the skin. And in addition, the weight is unstable, the stool is unclear - is the child healthy? Healthy, and all these changes are so-called transient (transitional) states. Where do they come from, what do they look like and what to do with all this?
The child sat in his mother’s belly for nine months, swam in the water and received oxygen through the placenta. As soon as the baby was born, his world immediately became different: instead of water there was air around him, the ambient temperature dropped from 36.6–37 °C to 22–25 °C, plus gravity, sounds, smells, bright light. And now you have to breathe yourself (with your lungs), eat differently, and then remove metabolic products. And just like that, it’s not easy for a newborn to immediately switch from one way of life to another; it takes time. That is why, from a physiological point of view, in the first month of life “something happens all the time” to children, and much more often and more vividly than in later life. These are transient (transitional, borderline) states. All of them surprise and even frighten young parents, especially since transitional states arise and disappear very quickly. But for newborns they are completely natural. What moms and dads most often see are transitional states of changes in skin, stool, weight, plus or minus a couple more conditions.
how skin changes
The child was born, and we see that he is all some kind of bluish-purple, and then the color of his skin immediately turns red. On the second day after birth, the baby “blushes” the brightest. Doctors call this redness “simple erythema,” and it appears because the skin is adapting to a new environment. Then the baby’s skin turns pale and by the end of the first week of life it becomes the usual pale pink color.
But that is not all. On the third to fifth day of life, the baby's skin may begin to peel, especially on the stomach and chest. What is this? Does the child lack vitamins, is there something wrong with the diet, is the air in the house too dry? No, this is also a transitional state - physiological peeling, and it is also due to the fact that the skin adapts to a new life. The skin peels for about a week, and then everything goes away. You don't need to do anything about it. Of course, you can treat the skin with various softening lotions and creams, but they will not have a significant effect. Very soon the baby's skin will become smooth and soft on its own.
What frightens parents most is the rash on the baby’s skin, which does not often, but sometimes still appear in the first week of life. This is the so-called toxic erythema - spots with grayish-yellow compactions in the center. The rash is most often located on the extensor surfaces of the arms and legs, around the joints, and on the chest. Less commonly, such spots can appear on the entire body (except for the palms, feet and mucous membranes). “Maybe it’s chickenpox, rubella or some other disease?” - Parents are scared. No, this is a peculiar reaction of the skin of a newly born child to its environment, especially to hypothermia, overheating, contact with clothing, and nutrition. New spots may appear within one to three days, but more often, two to three days after they appear, they all disappear without a trace. The child’s well-being is not affected, his body temperature is normal and he does not require any medications. The only thing is that you need to be careful about the bubbles on your skin: for example, gently blot them after bathing. You also need to be careful not to rub the blisters and burst them (otherwise they may become infected).
physiological jaundice
The changes visible on the skin do not end there. Very often (in 60–70% of children) the skin turns yellow on the second or third day of life, maximum yellowness occurs on the third or fourth day, and by the end of the first week it disappears. This is how physiological jaundice of a newborn manifests itself - a condition in which the amount of bile pigment, bilirubin, increases in the child. In some children, jaundice will look like a light tan (parents may not notice it), while in others the skin will become a bright yellow color. Very quickly, the bilirubin level returns to normal and the skin color returns to normal. If the jaundice is mild and goes away quickly, then no additional treatment is needed. But if the jaundice does not disappear or the skin color is intensely yellow, you should consult a doctor.
weight loss
Do you think the baby will be born immediately well-fed, with folds and cute roundness? No, immediately after birth this is still a long way off. In the first days of life, an already not very well-fed newborn will lose even more weight. This weight loss is a natural process, the so-called physiological weight loss. Weight decreases because immediately after birth the baby loses some of its water through the skin, its umbilical cord dries out, meconium (the first feces) and urine are released, and also because the baby still eats a small amount of milk. Maximum weight loss usually occurs by the third to fifth day and is normally no more than 6–8% of birth weight. At this time, mother and baby are usually discharged from the hospital, but there is no need to worry. By the seventh to tenth day of life, a healthy baby will restore its previous parameters.
stool changes
On the first or second day, all newborns pass their first stool (meconium): it is thick, viscous and dark green in color. Time passes, the baby begins to receive colostrum, and on the third or fourth day of life, transitional stool appears. Now areas of dark green color alternate with greenish and yellow, and some lumps and mucus are also visible in the stool. This all sounds like some kind of intestinal disorder, but it is not it. The gastrointestinal tract simply switches to a new job, now it is ready to digest food. By the end of the first week of life, most children's stools are yellow and mush-like, and they will continue to be that way.
warm-cold
A typical fear of all grandmothers is that the child is freezing! Yes, indeed, in newborns the processes of regulating body temperature are still imperfect, so babies easily cool down, but they also overheat just as easily. For example, if a newborn is dressed too warmly or placed next to a radiator, he will quickly overheat, even if this is the normal temperature in the room. At the same time, a child easily loses heat when he is undressed for a long time or lies in wet clothes. Therefore, in the room where there is a newborn, the air temperature should be adequate - 20–22 °C. And if she rises higher, and the child is dressed warmly, then this will also be bad.
Sometimes, very rarely (in 1% of children born), body temperature on the third to fifth day can temporarily rise to 38–39 °C. There are no other symptoms of the disease, the body temperature quickly returns to normal, but the parents manage to get scared. It’s difficult to figure out on your own whether it’s temporary hyperthermia or a disease, so it’s better to call a doctor.
hormonal crisis
An infrequent occurrence, but it also occurs sometimes. In some children, on the third or fourth day of life, the mammary glands become engorged (both girls and boys). They increase to their maximum by the seventh or eighth day, and liquid discharge may even appear from them. Some girls sometimes have very scanty bleeding from the vagina for a very short time. This is the so-called hormonal crisis - it occurs due to the action of maternal hormones - estrogens (they penetrate through the placenta during childbirth). At the peak of estrogen action, the signs of a hormonal crisis are maximum, then the hormones are eliminated from the body and the symptoms gradually disappear. Therefore, there is no need to apply a cabbage leaf to your chest, make compresses with camphor or anything else: everything will go away on its own.
Usually, all these transitional states are clearly expressed in the first week of life, less often, but it happens that they drag on for up to three to four weeks. Another point is that it is not necessary that the child will exhibit all transitional states, but physiological loss of body weight and transitional stool occurs in almost everyone. And many of the transitional states are completely invisible to parents, but they also exist; they can only be identified only by laboratory methods.
So we don’t rush to get scared when we notice that the child’s skin suddenly begins to peel off or he turns slightly yellow. We remember that he must adapt to the new life, that in the first time after birth the baby has the right to some changes. Especially if, despite all this, the baby is cheerful, calm and eats well. Well, if you are still somehow worried, ask your pediatrician questions. He will definitely be able to put everything in its place.
Insertion
Maximum weight loss in a newborn usually occurs by the third to fifth day and normally amounts to no more than 6–8% of birth weight.
From a physiological point of view, in the first month of life with children, “something happens all the time,” and much more often and more vividly than in later life. These are transient (transitional, borderline) states.
In infants, the processes of regulating body temperature are still imperfect, so they easily become hypothermic and overheated. In this regard, in the room where there is a newborn, the air temperature should be about 20–22 °C.
Physiological jaundice of a newborn:
– appears on the 2–3rd day of the baby’s life, reaches a maximum on the 4–5th day, and disappears by the 10th day;
– the child’s general condition does not suffer;
– the level of bilirubin in the blood does not exceed 180 µmol/l
Marbled leather
During the first month of life, a baby's skin sometimes looks marbled. A uniform mesh pattern of white, purple, and reddish spots is the reaction of skin vessels to cold. Therefore, this phenomenon is most often noticed during swaddling. If the marbling is symmetrical and disappears when warmed, then there is no cause for concern. In other cases, it is worth discussing this symptom with your pediatrician so as not to miss the early diagnosis of diseases of the heart, lungs or skin itself.
Peeling
On the second or third day after birth, the newborn’s skin begins to peel off. Peeling is observed in everyone, but to varying degrees of severity. Most severe if the baby is post-term. The reason is the same restructuring of the body to exist in the air. The skin loses moisture, and the top layer gradually peels off. Physiological peeling does not require treatment and goes away on its own within a few days.
If the peeling is profuse and leads to deep cracks, the skin is lubricated with special moisturizers - emollients. In case of pronounced peeling, it is necessary to exclude congenital skin diseases such as ichthyosis, hyperkeratosis and others.
Skin rashes on babies: causes, treatment and prevention
In the first months of life, babies are prone to various types of irritation and rashes on parts of their body. This phenomenon is quite normal and in most cases is considered normal. This is due to the fact that the baby’s body is still very vulnerable, and it is just beginning to adapt to external and internal factors that can negatively affect the child’s condition. In addition, up to two or three months the baby is faced with hormonal changes, which often causes similar reactions. Consequently, a rash is not always a cause for concern and panic, but a specialist can best determine the nature of its occurrence and methods of treatment. There are a number of reasons that provoke the appearance of pimples, spots or redness on the skin of a newborn:
- hormonal rash;
- prickly heat;
- dermatitis;
- hives;
- food allergies;
- infections and viruses.
In 70% of cases, the rash occurs precisely on a hormonal background, which is completely normal and does not require treatment, especially medication. This is due to the receipt of maternal hormones while still in the womb, and subsequent adaptation to new conditions. Distributes on the forehead, temples, and on the back of the head under the hair. It goes away on its own, usually within a few days. In this case, the mother is recommended to simply bathe the baby daily in boiled water with the addition of a herbal solution (series). During the hot season, the baby’s delicate skin is doubly prone to various manifestations due to drying out in the sun. All areas exposed to sweat also become vulnerable. Miliaria is not life-threatening for the baby, but it can cause discomfort in the places where it is localized. You should bathe your child more often, ventilate the room, and, if possible, maintain optimal humidity where the baby spends most of his time. Of course, you should not dress your child in clothes that will make him hot and uncomfortable. It is useful to give the baby time to be without clothes and diapers so that the skin has the opportunity to breathe. In addition, it is recommended to always wash small items only using a special children's powder, and then iron them on both sides.
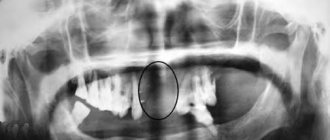
Erythema toxicum
By the second or third day of life, 70% of full-term newborns develop a small red rash on the skin. Rarely, this condition occurs in premature babies. First, spots appear, and within an hour a yellow bump 1-2 mm in size forms in the center. Elements of the rash are located on the face, torso, arms and legs, and can merge with each other. The cause of erythema toxicum is unknown, but the rash goes away without treatment in 1-7 days and is not dangerous.
If the clinical picture is atypical or other symptoms are present, the doctor will prescribe additional examination to rule out other causes of the rash, such as infection.
Newborn acne
20% of newborns develop a rash similar to teenage acne from the third week of life. Small pustules surrounded by a red halo. They are located on the face, head, chest, shoulders, and less often on the stomach. The condition is called “acne,” although in the literature the term “cephalic pustulosis” (from the words “cephalo” - head and “pustule” - abscess) or “neonatal pustulosis” is more often used. The main two reasons are the influence of maternal hormones during breastfeeding and the colonization of the skin by microorganisms. Elements of the rash resolve without treatment after 1-3 months. This condition is not dangerous, does not cause discomfort to the child and leads to independent recovery, so there is no need to prescribe medications. The exception is severe cases when the rash is profuse, leads to secondary infection or heals with the formation of scars.
Infant acne
The same rash in children after three months of age is called infant acne. It persists as persistent acne of newborns or reappears at 2-3 months. It differs from newborn acne only in the age of the children and the duration of the rash. Self-resolution occurs within 6-12 months. Infantile acne may be a risk factor for acne during adolescence.
Prickly heat
Develops in children from the second week of life when overheated. The rash has different manifestations: small red spots, nodules, pustules or blisters in the thickness of the skin. Miliaria can occur on any part of the body: in the folds, on the face, scalp, torso, arms and legs. The cause of the rash is blockage of the sweat glands.
There are several factors contributing to this:
- high room temperature;
- increased body temperature in a child;
- thick clothing, non-breathable fabric, for example, an oilcloth mattress cover;
- lying in one position for a long time.
Treatment consists of general care:
- daily bathing without soap and other chemicals;
- using lighter and looser clothing;
- maintaining the air temperature in the room at 22-24 degrees C;
- ventilation.
When these conditions are met, prickly heat disappears within a few hours. The recommendations listed above also apply to prevention.
For walks outside, the child is dressed like an adult plus one layer of clothing. No need to re-wrap. There is also no need to wear a cap in warm weather.
During the cold season, undress your child during a long stay in a store, shopping center or other premises. While awake, place your baby on his stomach and hold him vertically in your arms to diversify his movements.
Causes of the rash
The most likely causes of abdominal rashes in childhood are:
- Irritation of an allergic nature. There are a lot of allergens that provoke a reaction from the immune system. A skin rash can be caused by formula or mother's milk (if the mother herself consumed allergenic foods). The main method of therapy for allergic rashes is identifying the allergen and eliminating it.
- Infectious lesions of the body. In such cases, the rash is usually severe and is accompanied by other symptoms (high fever, signs of general intoxication of the body).
- Impact of external factors. Prolonged contact with wet underwear and untimely diaper changes can cause prickly heat in infants and older children.
- Insect bites - mosquitoes, bedbugs, fleas.
- Taking medications - any medications can have side effects in the form of rashes, itching and other manifestations.
You should not try to determine the cause of the rash on your own - a qualified specialist in childhood diseases will do this more effectively. If a rash on a child’s stomach is accompanied by additional symptoms, calling a doctor is mandatory.
Read also: Allergies in children
Diaper rash
A more serious skin reaction to overheating is diaper rash. Occurs in natural folds. It looks like redness, sometimes with weeping and erosion. With a long process, a bacterial or fungal infection may develop, then the surface of the affected skin is moist, bright red, with clear or purulent discharge. Prevention measures are the same as for prickly heat.
The skin in the folds is treated with powders. If normalizing the microclimate and caring for the newborn does not lead to a reduction in diaper rash, you should see a doctor. If complications occur, antibiotic therapy or topical steroid ointments may be needed.
White spots on the skin of children – vitiligo, pityriasis alba
Authors : Christophe HSU, Global Dermatology Information Portal
Typical causes of white spots on the skin of children are: 1) Pityriasis alba 2) Vitiligo
What is “Pityriasis alba”?
- Pityriasis alba is a mild form of dermatitis (skin inflammation).
- This condition is characterized by the appearance of numerous oval, slightly scaly, smooth, hypopigmented (white) patches on the face, arms, and upper torso.
- The boundaries of these spots are unclear.
- The disease occurs in children aged 3 to 16 years; about 30% of children at this age may be susceptible to this disease.
- The spots are not accompanied by itching.
- This disease is often mistaken for a fungal infection (mycosis).
- The condition tends to worsen with exposure to sunlight.
Treatment of pityriasis alba and preventive measures
- This disease is safe. It occurs in cases of hereditary predisposition or against the background of atopic dermatitis. The treatment essentially involves moisturizing the skin.
- The disease can last from several months to several years with a slow spontaneous recovery process.
- Sometimes steroid creams can improve the condition.
- Do not self-medicate.
- Avoid using antifungal creams.
- Limit the use of soap when washing your skin and use detergents that do not contain irritants.
What is vitiligo?
- Vitiligo is the loss of skin pigmentation in certain areas of the skin. These areas of skin appear as smooth white spots with clear contours. The hair in the area of vitiligo spots is often also white.
- There are two types of vitiligo:
- Type A: Vitiligo appears as numerous white patches, widespread and symmetrical. This type of vitiligo most often affects areas of the body such as the limbs, face and neck.
- Type B: Vitiligo appears as localized patches of segmental distribution. This type of vitiligo is most common among children.
- Vitiligo type A tends to spread to other areas of the skin, forming new lesions over time.
- Vitiligo type B tends to spread rapidly and then stop progressing after about one year.
- The causes of vitiligo are not fully known. Among people suffering from vitiligo, the most common cases are diabetes mellitus and thyroid disease.
How is vitiligo treated?
- Your doctor may prescribe one or more of the treatments listed below:
- Topical steroid creams. This method may promote skin repigmentation in some patients.
- PUVA (psoralen + ultraviolet A) is a combination treatment that involves using the drug Psoralen (P) and then exposing the skin to ultraviolet A (UVA). Psoralen can be applied to the skin as a lotion or taken orally in tablet form to increase the skin's sensitivity to ultraviolet rays. Patients undergoing PUVA treatment should be aware that the duration of therapy may be more than a year to achieve optimal results. It is best if this treatment is carried out under the supervision of a dermatologist.
- Concealing cosmetics. Using some cosmetics, you can choose a color that most closely matches your natural skin color. Concealing cosmetics are found to be effective in covering up white spots on the face and back of the hands.
- Sunscreens. Areas of skin affected by vitiligo are prone to sunburn. It is recommended to use sunscreen on affected areas exposed to sunlight.
- Response to treatment may vary across different affected areas of the skin and may vary between patients.
Source
Diaper dermatitis
The distinctive feature of this rash is that it appears only in the area under the diaper, other areas of the body remain clean. The reason is increased humidity and irritating feces.
The rash is found in the buttocks, thighs, lower abdomen in the form of individual elements or continuous areas of changed skin. The elements of the rash are varied: red spots, bumps, pustules or peeling.
To alleviate the condition, you need to change the diaper and wash the baby immediately after bowel movement. While changing clothes, you can arrange air baths, that is, leave the child to lie naked, you can cover it with a regular dry diaper. Lubricate the skin with a special diaper cream.
Change the diaper every 3 hours, even if it is only slightly full. More often when very full. If these measures are ineffective, you should consult a doctor. Local glucocorticoid agents may be needed.
Dermatitis due to food allergies
- Symptoms
An allergic reaction to various foods can be accompanied by the development of edema, the appearance of rashes on the skin in the form of blisters, red spots, rashes in the form of pustules and papules with serous contents, often itching. These symptoms usually occur within minutes to hours after eating the allergen. In addition to skin damage, nausea, diarrhea, and manifestations of hypersensitivity reactions from the respiratory tract are possible. In very young children, food allergies are sometimes accompanied by diaper rash in the folds of the limbs, eczema, and increased dryness or, on the contrary, moisture of the skin.
- Treatment
To treat skin breakouts, you must first follow an elimination diet. In this case, the product that presumably causes a specific reaction is excluded from the diet (in children in the first year of life, most often cow’s milk protein). Local anti-inflammatory therapy using creams and ointments is used as needed. Modern antihistamines are also often recommended to relieve symptoms. Additionally, sedatives can be used (as prescribed by a doctor).
If a child has a food allergy, the doctor may recommend that the child and mother follow a diet (reduce or eliminate milk and dairy products from the diet) if she is breastfeeding.
Formula-fed children need medicinal formulas based on highly hydrolyzed (broken-down) proteins, which do not cause allergies and help normalize the function of the gastrointestinal tract. For example, Nutrilak Peptide MCT , which also contains such important components as omega-3 and omega-6 fatty acids, nucleotides and a balanced vitamin and mineral complex, is recommended for allergies to cow's milk protein and food allergies.
Children are also bottle-fed, but to prevent allergies or for mild manifestations of allergies (taking into account the causally significant allergen and in agreement with the doctor), there are special hypoallergenic mixtures, for example Nutrilak Hypoallergenic . This mixture contains lactobacilli L.Rhamnosus LGG ® - a probiotic with proven effectiveness in the prevention and treatment of atopic dermatitis and eczema in infants. Nutrilak Hypoallergenic contains hydrolyzed protein, as well as bifidobacteria BB-12, which enhance the effect of the probiotic and help improve the balance of microflora.
Seborrheic dermatitis
Appears in infants soon after birth and lasts up to a year. Yellow scales and peeling are most often located on the scalp and behind the ears, but can also be in other folds - axillary, elbow, inguinal. In everyday life they are called “milk crusts”. Because of its similarities to atopic dermatitis, seborrhea is sometimes considered a manifestation of allergies. The causes of this condition are not fully understood, but the relationship with allergies has not been identified.
Seborrhea goes away without treatment, in most cases in the first year of life. Unlike atopic dermatitis, the rash does not cause itching and does not cause discomfort to the child. If for the sake of aesthetics you want to get rid of seborrheic crusts, before bathing the baby’s head is lubricated with oil and then combed out with a soft comb.
In doubtful cases, when seborrhea is located on the body, it makes sense to consult a doctor to clarify the diagnosis.
What diseases can be accompanied by a rash on the stomach?
There are dozens of diseases that can cause spots, rashes, itching and redness on the skin on the abdomen.
The most common options:
- Chickenpox is an acute viral disease accompanied by a small rash on the body, including in the abdomen;
- Scabies is a disease caused by scabies mites (characterized by the appearance of small vesicles mainly in the navel area);
- Measles is a viral pathology accompanied by high fever and the appearance of dark spots on the skin;
- Scarlet fever is a bacterial disease, which, in addition to general symptoms, is characterized by the appearance of a small rash in the lower abdomen;
- Lyme disease is a pathology transmitted by ticks (the earliest symptom of the disease is red spots at the site of the bite);
- Dermatitis is the most common type of allergy.
If you detect a rash in a timely manner and classify its nature, you can quickly identify the disease, prescribe adequate and correct therapy, and prevent the consequences and complications of the pathology. Sometimes rashes on the abdomen require immediate therapeutic intervention. The most appropriate and reasonable course of action for parents who discover spots on their child’s belly is to seek help from a professional pediatrician. An experienced doctor sometimes only needs one look at the rash to understand what he is dealing with.
Atopic dermatitis
This is a chronic inflammatory skin disease. It occurs in 15% of children, of whom two thirds experience the first symptoms before one year of age, sometimes even in infancy. The rash appears on the face, torso, and extensor surfaces of the arms and legs. There may be redness, peeling, crusts, and when scratching, infection and the presence of pustules may occur. Elements of the rash itch and bother the child.
Only 30% of children have atopic dermatitis associated with food allergies. Therefore, a nursing mother does not always need a diet.
The cause of atopic dermatitis is increased skin permeability. For treatment, first of all, creams that restore barrier function are used. They are called emollients. There are quite a few brands that produce such products. The choice is based on personal preference. From a medical point of view, there is no advantage to any particular drug.
If you suspect atopic dermatitis, you need to see a doctor to clarify the diagnosis and receive recommendations for treatment. You can contact your pediatrician or dermatologist. If the diagnosis is confirmed, keep in mind: treatment will be long. It includes skin care and constant use of emollients; in more severe cases, hormonal ointments may be needed; for food allergies, a diet. It is important to understand that with strict implementation of the recommendations, stable long-term remission can be achieved.
Contact dermatitis
- Symptoms
This hypersensitivity reaction is accompanied by redness and swelling of the skin immediately after contact with the allergen or several hours later. Small blisters, papules, and weeping erosions may appear on the affected area. A characteristic symptom of skin allergies is itching. As the inflammation subsides, scales and crusts form at the site of the blisters and inflammation. With chronic contact dermatitis, peeling of the skin is common.
- Treatment
To stop the development of an allergic reaction in an infant, it is necessary to avoid contact with the irritant substance. These can be food products, certain components of detergents and cosmetics, the juice of certain plants, etc. To treat red spots due to skin allergies, local anti-inflammatory drugs in the form of creams and ointments can be used. If swelling is severe, wet-dry dressings may be indicated. In severe cases, systemic hormonal therapy is used to treat the symptoms of contact dermatitis.
Mastocytosis
A rare disease that can appear at an early age, sometimes even from birth. Outwardly, it resembles allergic urticaria, but spots and blisters last longer, and when the exacerbation subsides, pigmentation remains. A typical diagnostic test is the appearance of blisters on the skin due to mechanical irritation of areas of pigmentation.
Treatment for childhood forms of the disease is not required; recovery occurs spontaneously within several months, sometimes several years. If itching is present, antihistamines are used.
Skin rashes on babies: causes, treatment and prevention
In the first months of life, babies are prone to various types of irritation and rashes on parts of their body. This phenomenon is quite normal and in most cases is considered normal. This is due to the fact that the baby’s body is still very vulnerable, and it is just beginning to adapt to external and internal factors that can negatively affect the child’s condition. In addition, up to two or three months the baby is faced with hormonal changes, which often causes similar reactions. Consequently, a rash is not always a cause for concern and panic, but a specialist can best determine the nature of its occurrence and methods of treatment. There are a number of reasons that provoke the appearance of pimples, spots or redness on the skin of a newborn:
- hormonal rash;
- prickly heat;
- dermatitis;
- hives;
- food allergies;
- infections and viruses.
In 70% of cases, the rash occurs precisely on a hormonal background, which is completely normal and does not require treatment, especially medication. This is due to the receipt of maternal hormones while still in the womb, and subsequent adaptation to new conditions. Distributes on the forehead, temples, and on the back of the head under the hair. It goes away on its own, usually within a few days. In this case, the mother is recommended to simply bathe the baby daily in boiled water with the addition of a herbal solution (series). During the hot season, the baby’s delicate skin is doubly prone to various manifestations due to drying out in the sun. All areas exposed to sweat also become vulnerable. Miliaria is not life-threatening for the baby, but it can cause discomfort in the places where it is localized. You should bathe your child more often, ventilate the room, and, if possible, maintain optimal humidity where the baby spends most of his time. Of course, you should not dress your child in clothes that will make him hot and uncomfortable. It is useful to give the baby time to be without clothes and diapers so that the skin has the opportunity to breathe. In addition, it is recommended to always wash small items only using a special children's powder, and then iron them on both sides.
Infantile hemangioma
Hemangioma is a benign tumor of endothelial cells (endothelium is the inner lining of blood vessels). It may be congenital or appear at 1-2 weeks of life. Superficial hemangiomas are bright red and protrude above the surface of the skin. Deep - blue-purple, sometimes warm to the touch. The element size ranges from a few millimeters to an entire anatomical area (hand, buttock, etc.). In the first 5-6 months, the hemangioma may increase in size and become brighter, then the growth ends and spontaneous regression begins.
Up to 90% of hemangiomas can resolve without treatment.
In this regard, surgical treatment is no longer used routinely. The child is observed by a pediatrician and a surgeon; if hemangiomas are located on the face and neck, in the genital area and near large vessels, conservative treatment is prescribed. The operation is indicated only if it is ineffective.
Types of rash
Rashes on the abdomen of a child are quite variable in nature and etiology (origin).
Pediatricians distinguish the following types of rash:
- Spots are areas with clear boundaries on the surface of the skin of a discolored color (spots do not protrude above the skin and cannot be felt during palpation);
- Papules are tubercles up to 5 mm in diameter, without an internal cavity and protruding above the skin;
- Plaques are formations raised above the surface of the epidermis, significant in area, having a flattened shape;
- Vesicles are formations with liquid contents;
- Bubbles are vesicles more than 5 mm in diameter;
- Pustules are cavities limited by the membrane with purulent contents.
Some diseases are also characterized by peeling of the skin. Any changes in the appearance of the skin surface are a signal that not everything is in order in the baby’s body. Of course, not all diseases accompanied by a rash require special therapy, but such signs should not be ignored in any case.
Vascular abnormalities
Congenital anomalies of vascular structure are varied
- A simple nevus is a capillary anomaly. It appears as a pale pink spot or several small spots. The common name “stork bite” or “angel kiss” arose due to its location on the back of the neck and head, on the forehead, bridge of the nose and upper eyelids. The spots fade by the age of two, but can appear when crying or physical activity. No treatment required.
- Port wine stain or flaming nevus. A dark red spot that looks like a hemangioma. It may be one of the manifestations of pathological syndromes. Lasts for a long time. Treatment is not necessary, but can be done if the spot creates a cosmetic defect.
- Venous anomaly - blue-violet painful nodules under the skin. They can also masquerade as a hemangioma. Occur alone or in combination with other anomalies. The danger lies in the possibility of thrombosis of the altered veins. Treatment consists of wearing compression clothing and using aspirin to prevent blood clots. Surgical excision is possible.
- More rare lymphatic, arteriovenous and combined anomalies are found as part of various pathological syndromes.