Anatomy, physiology
The periodontium
is a complex organ of the oral cavity surrounding the teeth, formed from specialized tissues. It is located on the jaws and its main functions are to support (support) the teeth and their nutrition and innervation.
Nutrition (trophism) is provided by blood and lymphatic vessels that supply oxygen and metabolic products to the periodontal tissue.
There are four main anatomical and functional elements of the periodontium:
- gum,
- periodontium,
- alveolar bone with periosteum,
- root cement
The gum is a soft tissue - a mucous membrane covering the alveolar processes, with an underlying connective tissue layer.
It contains lymphatic vessels (they are involved in regulating fluid pressure in tissues and protecting against microbial agents).
Through the periodontium - the ligament of the tooth, the latter is fixed in the jaw bone.
Periodontium
(otherwise known as desmodont) is a connective tissue formation surrounding the tooth and located between the root cement and the inner cortical plate of the alveolar bone.
This ligament, consisting of the main substance, fibers and cellular elements, like an elastic gasket, absorbs the load on the tooth, giving it minimal mobility. When periodontal disease and death occur, fusion of the bone with the tooth – ankylosis – can occur.
The next element of the periodontium is cement, which is also a hard tissue covering the root of the tooth. It is formed by collagen fibers directed along the root and an adhesive substance.
Bone
The alveolar process, in which the tooth is strengthened by periodontium, is composed of outer and inner dense plates and a spongy part between them.
Spongy bone consists of trabecular septa, the direction and shape of which is determined by the load on the jaws and teeth, and bone marrow.
Bone tissue contains mainly crystals of hydroxylapatite (inorganic) and small amounts of water and organic substances.
The cellular elements of bone - osteoblasts, osteoclasts and osteocytes, under the influence of the nervous and humoral system, determine changes in the shape, volume and quality of this tissue.
The bone tissue of the alveolar process is covered with a dense connective tissue structure - the periosteum; it, with the vessels located in it, plays a significant role in the blood supply to the bone.
The blood supply provides tissues and anatomical formations with organic and mineral substances.
At the level of the enamel-cement junction (neck of the tooth), an anatomical formation stands out in the marginal part of the gum - a vascular cuff, which, like an elastic band, ensures a tight fit of the gum to the tooth due to hydrostatic pressure.
The main source of blood supply to periodontal tissue is the external carotid artery with the maxillary and mandibular arteries branching from it.
Venules and veins collect blood into the internal jugular vein. The periodontium is innervated by the trigeminal nerve and the superior cervical sympathetic ganglion.
Among others, there is an anatomical formation - the dentogingival junction
. This is the connection between the gum epithelium and the neck of the tooth.
It is physicochemical: molecules of epithelial cells adhere to cement structures through gingival fluid cells.
Gingival fluid produced by periodontal tissue plays the role of a protective barrier against microorganisms through the activity of phagocytes and its chemical properties. It should be noted that the periodontium is washed by saliva. It is secreted by the major and minor salivary glands.
In addition to water (99.42%), saliva contains organic substances, salts and trace elements. Organic substances enter the oral fluid from blood serum and are secreted by the salivary glands and microorganisms present in the mouth.
Of the inorganic substances, calcium phosphate and calcium bicarbonate (they take part in the formation of tartar), phosphate and sodium chloride are important.
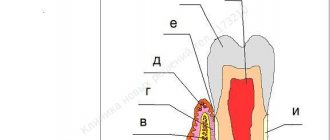
Diagram 1: periodontium
. a – submucosal layer with lymphatic vessels; b — mucous membrane of the attached gum; c - spongy bone of the alveolar process between the plates of the compact substance; d – periodontal fibers are woven into the root cement; e – gingival margin with vessels of the gingival cuff; e – dentogingival junction; g – tooth enamel; h – dental pulp; and – root cement; j – root dentin.
Age-related changes in periodontium
In the periodontium, with age, there is a decrease in the number of collagen fibers and a decrease in their quality. The epithelial layer of the mucosa becomes thinner, and keratinization is disrupted.
The bone tissue of the alveoli becomes less dense, the cortical layer atrophies.
Periodontitis
In children, periodontitis is more common, localized in the area of 1–2 or groups of teeth in the frontal area of the jaws with crowded teeth or dental anomalies, with anomalies in the structure and attachment of the frenulum of the tongue, lips, and the small vestibule of the oral cavity. The following signs are characteristic of periodontitis:
- complaints of bleeding gums, sometimes pain in them during exacerbation, bad breath; with initial changes, complaints may be absent;
— symptomatic gingivitis (catarrhal, hypertrophic);
— deposition of supra- and subgingival soft plaque and tartar;
— destruction of the periodontal epithelial attachment;
- formation of periodontal pockets with serous or purulent contents;
— destruction (destruction) of the edge of the alveoli (interalveolar septa), determined on an x-ray;
- exposure of the necks and roots of the teeth;
- tooth mobility and traumatic occlusion.
In the initial form of periodontitis, there may be no complaints; mildly expressed symptoms of catarrhal gingivitis, plaque deposition, false periodontal pockets up to 2–2.5 mm are clinically determined, the teeth are stable, the necks of the teeth are not exposed. X-rays reveal vagueness or destruction of the cortical plate at the apexes of the interalveolar septa and slight osteoporosis of their spongy substance.
In mild forms of periodontitis, patients complain of bleeding gums when brushing their teeth; symptomatic catarrhal gingivitis, small amounts of plaque and tartar deposits, periodontal pockets up to 3.5 mm deep, and slightly or 1st degree tooth mobility are clinically determined. The radiograph reveals the absence of a cortical plate at the apexes and lateral sections of the interalveolar septa, expansion of the periodontal fissure in the cervical region, and subsequently destruction of the interalveolar septa up to 1/3 of the root length; foci of osteoporosis of the interalveolar septa. In the chronic course, osteoporosis is not clearly expressed, and during exacerbation it is diffuse in nature.
In the moderate form of periodontitis, complaints of bleeding gums appear during brushing teeth and eating, symptomatic gingivitis, deposition of tartar and plaque, periodontal pockets up to 5-6 mm with serous or purulent discharge are clinically determined; mobility of teeth of the 1st–2nd degree, exposure of the roots of the teeth occurs. The X-ray shows destruction of the interdental septa from 1/3 to 1/2 of the root length, expansion of the periodontal fissure, osteoporosis is insignificant in the chronic course, and diffuse in case of exacerbation.
Severe periodontitis is characterized by complaints of bleeding and sore gums when brushing teeth and eating. Clinically, symptoms of catarrhal or hypertrophic gingivitis are detected, significant deposits of supra- and subgingival calculus and soft plaque, pockets more than 5-6 mm deep, filled with granulations and purulent contents. The radiograph shows destruction of the interalveolar septa within 2/3 of the root length, diffuse osteoporosis of the remaining bone tissue of the septa, mobility of teeth of the 2nd–3rd degree, exposure of the roots, displacement of teeth and traumatic occlusion.
Diagnosis of periodontitis in children
Examination of a child with periodontitis begins with a study of complaints, medical history and life history. Anamnestic data includes information about the physical and intellectual development of the child, common and infectious diseases suffered and existing at the time of examination. When examining a child, pay attention to his posture, since it is a factor in the full development of the child and a risk factor for anomalies in the development of the dental system.
Examination of the face in front and profile at rest and when closing teeth, during conversation and facial movements allows us to determine functional deviations in accordance with facial characteristics. Thus, the “thimble” symptom in the form of pinpoint retraction of the skin on the chin is a sign of impaired swallowing function. Pay attention to the state of tone of the facial and chewing muscles at rest and during function. The type of breathing (nasal, oral, mixed), the position of the lips (closed, open, tense or atonic), the state of the red border of the lips (color, volume, turgor, architectonics, etc.) are determined, which makes it possible to establish a violation of the basic functions of the dental system and bad habits. The condition of the temporomandibular joint and the lymphoid apparatus of the maxillofacial skeleton is assessed.
A study of the vestibule of the oral cavity allows us to judge its depth, severity and nature of attachment of the labial frenulum to the alveolar process, the state of the mucous membrane covering it, the degree of teething, their position in the dentition and the relationship of the jaws. The depth of the vestibule of the oral cavity is determined by horizontal abduction of the lower lip by the distance from the edge of the marginal gum to the level of the transition of the mucous membrane to the lip. The vestibule is considered shallow if the specified distance does not exceed 5 mm, medium with a depth of 5 to 10 mm, and deep over 10 mm. The area of the attached (alveolar) gum is measured in millimeters, as well as the depth of probing of periodontal pockets using a graduated blunt probe. In addition, the localization of the gingival margin relative to the enamel-cementum boundary (degree of root exposure) and the presence of bleeding upon light probing must be determined.
When examining the oral cavity, the condition of the salivary glands, the position, size of the tongue, the structure and nature of the attachment of the frenulum of the tongue, the shape and relationship of the dental arches, and the presence of crowding of teeth in the frontal area are assessed. The teeth are examined to identify carious lesions, and the quality of the applied fillings is assessed. The mobility of teeth and their occlusal and interdental relationships, the presence of plaque and tartar are determined.
To objectively identify the symptoms of gingivitis and its prevalence, the Schiller-Pisarev test is used, and the degree of gum inflammation is determined using the PMA index. The degree of destructive changes in the periodontium is determined by the periodontal index. Assessment of the hygienic state of the oral cavity is carried out using the Fedorov-Volodkina, Green and Wermillion hygienic indices. It is mandatory to determine the uniformity of the occlusal load using the fingerprint method (occlusiogram), as well as radiographic examination of the periodontium. If X-histiocytosis is suspected, an X-ray examination of the jaws and skull bones is performed.
In addition, a study of the child's developmental history is necessary; conducting clinical blood tests (general, for glucose levels to exclude diabetes), as well as determination of immunoglobulin levels to exclude immunoglobulinemia, a general urine test, and if X-histiocytosis is suspected, for neutral fat. According to indications, cytological and microbiological methods are used to examine periodontal pockets. The child must be examined by a pediatrician, hematologist, endocrinologist, immunologist, pediatric gynecologist, psychoneurologist, etc. in order to identify and treat systemic diseases that may affect the course and outcome of treatment of gingivitis and periodontitis.
Differential diagnosis
Periodontitis must be differentiated from chronic gingivitis and changes in the periodontium with X-histiocytosis, diabetes mellitus, constant and cyclic neutropenia, etc. Some difficulties arise in the differential diagnosis of the initial forms of periodontitis with gingivitis. X-ray data are decisive in this case. With chronic gingivitis, as a rule, there are no changes in the alveolar bone on the radiograph; only in rare cases, with long-term and untreated gingivitis, osteoporosis of the interalveolar septa is observed. When analyzing radiographs, it is necessary to take into account the variability of the shapes of the interalveolar septa in children, as well as the fact that the periodontal gap in the area of the necks of the teeth before the formation of the permanent dentition is wider than in other areas; during the period of teething, the interalveolar septa are not formed, the cortical plate at their apexes is not determined.
When differentially diagnosing periodontitis with changes in the periodontium with X-histiocytosis, one must keep in mind that with X-histiocytosis, along with changes in the alveolar bone, there are foci of bone tissue destruction in the body and branches of the lower jaw. In diabetes mellitus, vertical resorption of the interdental septa with funnel-shaped, crater-shaped pockets predominates, which does not extend to the body of the jaw. With constant and cyclic neutropenia, the process is limited to the interalveolar septa and has clear contours.
With cyclic neutropenia, exacerbation of the process occurs at strictly defined intervals, characteristic of a particular child (usually 21 days) and lasts 4-5 days.
Prepubertal periodontitis
Occurs in children under 11 years of age. The most common form is a generalized one. The disease begins during or shortly after the eruption of baby teeth and is manifested by a violation of the attachment of the gums to the teeth and severe destruction of the alveolar bone, leading to premature tooth loss in children from the age of three. The early and aggressive course is due to the fact that such patients have immune defects - there are few monocytes and polymorphonuclear leukocytes in the blood. All children from birth have decreased resistance to infections, furunculosis, pustular skin diseases, otitis, and pneumonia. The children are pale and have low nutrition. This disease is associated with microorganisms of the bacteroid type: Porphyromonas gingivalis, Actinobacylus actinomycetemcomintans. Infection occurs from parents, the window of infection is from 1 to 3 years. It begins with the primary destruction of the periodontium, while at first there are no symptoms of gum inflammation. Subsequently, the architectonics of the gingival margin changes, the gums seem to recede, the necks of the teeth are exposed, deep periodontal pockets form, and then inflammation develops. X-ray reveals vertical destruction of the alveolar bone. Subsequently, mobility, movement and loss of teeth occur. There are no symptoms of bleeding or pain. There is no tartar, the teeth are covered with a soft plaque. Children first lose their milk teeth, then the process spreads to the rudiments of permanent teeth, they erupt early, similar changes occur with them, and by the age of 14–15 all teeth fall out. However, the pathological process does not extend beyond the alveolar bone. With the loss of permanent teeth, the destructive process in the jaws stops.
The same changes in the periodontium, combined with palmoplantar hyper- or dyskeratosis in the form of cracks on the palms, feet, forearms, and increased sweating, are also observed in Papillon-Lefevre syndrome. There is evidence in the literature that taking tetracycline antibiotics for Papillon-Lefevre syndrome during the primary dentition period prevents the development of generalized periodontitis in the permanent dentition and the loss of permanent teeth.
Pubertal (teenage) periodontitis
There are 2 forms: localized and generalized. Localized pubertal periodontitis is observed in practically healthy children and adolescents without systemic diseases. It is characterized by rapid and severe destruction of the alveolar bone in the area of the first permanent molars, and sometimes the incisors. Clinically, mild inflammation (which may be absent) and a small amount of plaque or tartar are observed. Bone tissue destruction progresses 3–4 times faster than with periodontitis in adults. Currently, this disease is associated with a bacteroid of the Actinobacylus actinomycetemcomintans type. In most cases, it occurs in children whose parents are carriers of this microorganism. It enters the periodontal tissue soon after teeth erupt. The process occurs with minimal inflammatory reaction. The rapid spread of the process is due to the fact that specific microflora not only populates the groove and subsequently the periodontal pocket, but also penetrates deep into the periodontal tissues, including bone tissue, where it is quite persistently preserved. On the other hand, this microorganism has the ability to suppress the chemotaxis of leukocytes, and antibodies in such cases do not have time to form. The periodontium is rarely damaged after the eruption of permanent teeth, since by this time specific antibodies have time to form and exert their protective effect. Previously, this disease was described as local desmodontosis, local monoalveolysis according to Orban.
Generalized pubertal (teenage) periodontitis is rare. In this case, the process often involves the periodontium of both jaws. It is characterized by an aggressive course, rapid and severe destruction of the alveolar bone. It is commonly called aggressive, or rapidly progressive, periodontitis. According to foreign and domestic literature, a large number of facultative anaerobic gram-negative rods, mainly Porphyromonas gingivalis, accumulate in the area of the affected teeth. The most aggressive course is associated with the combination of this microorganism with Actinobacylus actinomycetemcomintans and Prevotella itermedia. It is with this combination that microorganisms exhibit a sharply positive mutual influence.
Classification of periodontal diseases.
Gingivitis
Gingivitis is an inflammatory superficial disease of the gum tissue.
With gingivitis, there is no disruption of the periodontal junction and bone. Based on the form of manifestation of periodontal disease, the following are distinguished:
- catarrhal gingivitis,
- hypertrophic gingivitis,
- ulcerative gingivitis.
According to the type of course, gingivitis is divided into acute, chronic, aggravated and remission. According to the distribution, gingivitis can be localized and generalized. Without active treatment, gingivitis progresses to periodontitis.
Periodontitis.
Periodontitis is a deep inflammatory disease of the periodontium with destruction of the periodontal junction and bone tissue of the alveoli.
There are acute, chronic course of periodontitis, exacerbation of the disease and remission. Periodontitis can be mild, moderate or severe.
According to the prevalence, this gum disease is divided into generalized and localized periodontitis.
Photo 1. X-ray picture of severe periodontitis. The roots of the teeth are exposed by two-thirds.
2. 1.
Additionally, there is a condition known as
an aggressive form of periodontitis.
This diagnosis can be made by a doctor based on the presence of a set of signs of gum disease. In this case, periodontal destruction is generalized and rapid.
Such periodontitis is typical for ages from adolescence to 35 years. Often the aggressive form of periodontitis is accompanied by gum growth and granulation. During the period of remission, inflammatory manifestations may subside and even disappear.
Periodontal disease
Periodontal disease is a chronic degenerative periodontal disease.
In European and American classification as a separate gum disease
doesn't stand out. Periodontal disease is characterized by a long-term, benign course and almost does not lead to loosening and loss of teeth.
Periodontal diseases - as symptoms of other diseases
There are idiopathic periodontal diseases with progressive destruction of periodontal tissue (periodontal syndrome).
Such conditions can occur when exposed to physical factors (radiation), poisoning, immunodeficiency, diabetes mellitus, eosinophilic granuloma, Papillon-Lefevre syndrome, neutropenia, etc.
Periodontomas. Epulis (epulid) and gingival fibromatosis
Periodontomas are tumors and tumor-like conditions of the gums. The most common of them are epulis (epulid) and gingival fibromatosis.
Gingival fibromatosis is characterized by the proliferation of periodontal tissues, which causes tumor-like damage to the gum tissue. Gingival fibromatosis is most common in adults, but is sometimes diagnosed in children.
The diagnosis of gingival fibromatosis is made by a specialist based on the patient’s complaints, examination data, radiography, and histological examination.
The main reason for the growth of gum tissue, as a rule, is a violation of metabolic processes; drug-induced fibromatosis of the gums is also identified. Treatment of the disease is surgical and consists of excision of the overgrown gum to the periosteum.
Photo 2. Gingival fibromatosis
Periodontal diseases and measures for their prevention
Periodontal diseases, as well as dental caries, have become very widespread. According to WHO, about 95% of the world's adult population and 80% of children have some form of periodontal disease.
What is periodontium? The periodontium is a complex of tissues that surround the tooth and ensure its fixation in the jaw bones. This complex includes the gum, periodontal ligament connecting the tooth root to the bone socket, bone tissue of the alveolar processes and cementum of the tooth root. With various periodontal diseases, the pathological process may involve any part of the periodontal complex or the entire periodontium as a whole. The nature of the pathological process can also be different: dystrophic, inflammatory or tumor.
Among all periodontal diseases, 90-95% are inflammatory, such as gingivitis and periodontitis. Therefore, we will focus on them in more detail.
Gingivitis is an inflammatory process in the tissues of the gingival margin, in which only the superficial tissues of the gums are affected.
Periodontitis is an inflammatory process that involves all periodontal structures. It is characterized by the destruction of the periodontal junction and the progressive destruction of the alveolar processes of the jaw bones.
In fact, gingivitis and periodontitis are two interrelated forms of the disease, since the inflammatory process occurs first in the gum tissue, and gradually the underlying periodontal structures are involved: the periodontal ligament and alveolar bone.
Currently, the main local pathogenetic factors underlying inflammatory periodontal diseases have been established. This is the accumulation of dental plaque (microbial factor), disruption of the structure of the vestibule of the oral cavity, dental anomalies and supracontacts.
The inflammatory process in the gum tissue initially occurs due to massive microbial accumulations and the enzymes and toxins they secrete. While the inflammation is limited only to the gums, and the underlying tissues are not affected, we are dealing with gingivitis, which occurs with periods of exacerbation and remission, with varying degrees of activity in different patients.
| Figure 1. Chronic gingivitis. |
The difference in the nature of the course of gingivitis is determined by the state of the general protective mechanisms in patients. That is why, with the absolute recognition of the microbial factor as a causative factor, the “interest” of the entire organism in the development and course of this seemingly purely local process was never questioned.
What complaints do patients have with gingivitis?
Most often these are complaints of bleeding gums.
Bleeding gums during brushing are noted by almost all patients with gingivitis. There may also be complaints of pain and bleeding gums while eating. The general condition, with rare exceptions, is not disturbed.
When examining patients, as a rule, a large amount of soft dental plaque is determined, especially in the area of the necks of the teeth. The gingival margin is usually hyperemic, swollen, and the gums bleed easily upon probing.
Since with gingivitis only superficial tissues are inflamed, easily accessible for viewing and targeted therapeutic interventions, the treatment of this disease is very effective.
The main method of treatment and prevention of gingivitis is the removal of microbial accumulations, that is, hygienic measures.
Hygiene products - pastes and toothbrushes - are the main weapon against inflammatory periodontal diseases. Moreover, they act equally effectively against inflammation in the periodontium and against caries, since the microbial factor is the main factor in both cases.
However, despite the presence of such an effective and affordable preventive and therapeutic agent, the problem of inflammatory periodontal diseases remains very relevant. Already in childhood, in 30-80% of cases, the initial stage of the disease is diagnosed in the form of superficial inflammation - gingivitis, the course of which is characterized by alternating periods of intense inflammatory reaction and relatively favorable periodontal condition. With age, the intensity and prevalence of the inflammatory reaction in the periodontium increases: in adolescents with gingivitis, destructive changes in the periodontium are observed in 2-6% of cases. Later, the frequency of superficial inflammatory changes, manifested in the form of gingivitis, decreases, and the prevalence of deeper destructive phenomena in the periodontium of varying degrees of severity increases significantly.
| Figure 2. Chronic periodontitis. |
The problem of adequate hygienic oral care and instilling the necessary hygiene skills in children is extremely difficult. Today, the domestic market offers hygiene products (pastes and brushes) of fairly high quality. The question is different: in order to achieve the necessary cleaning of the teeth and gums, it is necessary to brush at least 20 times on one surface of the tooth, the total time of brushing the teeth - from the outside and inside - should be at least three minutes, otherwise the microbial plaque will persist. In addition, it is necessary to treat the interdental spaces with floss (dental floss). It is necessary to teach children this from a very early age in order to develop in them the need for such brushing of their teeth at least twice a day.
Until the child is consistently motivated for this type of care, it is difficult to expect tangible results in relation to the condition of the gums and teeth. It should be remembered that the quality of teeth cleaning largely depends on individual manual skills. Many children, no matter how hard they want, simply cannot brush their teeth well, even if they try very hard. The above directly applies to children with general developmental disorders.
What could be the way out of this situation? The doctor should regularly carry out appropriate treatment or prescribe drugs that effectively suppress the activity of microorganisms and slow down the formation of microbial accumulations. For these purposes, today the most effective drug is chlorhexidine bigluconate, which sharply inhibits the vital activity of all microbial accumulations that cause damage to periodontal tissue and hard tooth tissue. In addition, it actively suppresses herpes viruses and fungi, and has a weak analgesic effect. The disadvantage of this remedy is its persistent bitter taste, which limits the use of this drug, especially in children. The drug Corsodil, which recently appeared on our market, does not have this disadvantage. Because of this, it has become widespread in many countries around the world. Staining of the surfaces of the tongue and fillings - a property of chlorhexidine - is a temporary phenomenon that passes fairly quickly. But the effect of using chlorhexidine both as a therapeutic and as a prophylactic agent is very high and stable. Patients use the drug independently, the course of treatment is 5-7 days.
As soon as inflammation overcomes the main barrier - the periodontal junction - it rushes into the underlying tissue - the periodontium and alveolar bone. Being a logical continuation of gingivitis, this form takes on completely new features. Firstly, a periodontal pocket is formed, in which microbial accumulations are securely hidden and are not removed during tooth brushing. Secondly, in the depths of periodontal pockets, the most aggressive microbial species actively multiply - anaerobes, spirochetes, the damaging potential of which is extremely high. Thirdly, from the pockets the microorganisms themselves, and their enzymes and toxins, easily penetrate into the underlying structures, dissolving them. As a result, the stability of the teeth decreases, they become mobile, and the mechanical load on the teeth during chewing turns out to be traumatic. As a result of this injury, the destruction of the supporting apparatus of the tooth occurs especially quickly, which, in turn, further contributes to the spread of microbial accumulations. Periodontitis forms.
| Figure 3. Rapidly progressive periodontitis. |
The complaints that patients usually make are mobility of teeth, bleeding gums, bad breath, fan-shaped discrepancy of the upper front teeth, exposure of the necks of the teeth.
On examination, hyperemia of the gingival margin is noted, often with a cyanotic tint; the gum does not fit tightly to the neck of the teeth.
When probing, periodontal pockets of varying depths are determined, depending on the severity of the process. There are supra- and subgingival dental deposits. When the process is severe, purulent discharge from periodontal pockets and significant tooth mobility may occur. Radiologically, with periodontitis, a decrease in the height of the alveolar process is noted due to resorption of bone tissue of the interalveolar septa.
Treatment of periodontitis is aimed primarily at removing microbial accumulations, tartar and granulations from periodontal pockets. If the periodontal pockets are deep enough, their thorough treatment is only possible through surgery. And after the operation, the main task is to prevent active penetration of microbial masses deeper into the tissue. This is more difficult to achieve, but again the main method of prevention in this case is high-quality controlled oral hygiene, the prescription of effective antimicrobial rinses, among which Corsodil is today recognized as the most effective.
There are a number of forms of inflammatory periodontal diseases that are characterized by increased aggressiveness. Their main difference is in the presence of specific microorganisms and their combinations.
Prepubertal periodontitis. The process occurs in childhood and involves the teeth of the permanent and even primary dentition. The early development and aggressive course is due to the fact that such patients have defects in general defense - monocytes and polymorphonuclear leukocytes. In such cases, the tactics of specialists boil down to more thorough antimicrobial control. But the result can only be achieved through the efforts of general specialists - if it is possible to eliminate blood cell defects with the help of targeted medication.
Focal juvenile periodontitis. With this form of periodontitis, selective damage to the supporting apparatus of the first permanent teeth occurs. The disease is caused by the species Actinobacillus Actinomycetes comitans. In most cases, it occurs in children whose parents are carriers of the microorganism. The process occurs with minimal inflammatory reaction. Its rapid spread is due to the fact that this type of microorganism has the ability to suppress the chemotaxis of leukocytes, and antibodies do not have time to form under such conditions. Therefore, subsequent permanent teeth are rarely damaged, since specific antibodies later have time to form and exert their protective effect. Treatment includes active antibiotic therapy - for at least 3 weeks - in combination with local interventions. The duration and need for general antibiotic therapy are due to the fact that microorganisms not only inhabit the periodontal sulcus, and subsequently the periodontal pocket, but also penetrate deep into the tissues and bone structures, where they persist quite persistently.
Rapidly progressive periodontitis, as well as periodontitis resistant to therapeutic interventions , is caused by a specific microflora: Porphyromonas gingivalis (formerly bacterioids), Actinobacillus Actinomycetes comitans and Prevotella intermedia. Moreover, it is usually their combination that occurs. In this case, these microorganisms exhibit a sharply positive synergistic mutual influence, and the microbial composition not only causes a sharp destructive effect on tissues, but also suppresses the effect of protective cells. In addition, invasion of these microorganisms deep into tissues is characteristic.
| Figure 4. Periodontal disease. |
Medical tactics consist of careful mechanical treatment of periodontal pockets and intensive antimicrobial therapy. Local application of metronidazole or tetracycline orally is effective. It is advisable to perform patch surgeries no earlier than 3-4 weeks after the start of antimicrobial therapy, otherwise, if the viability of the listed microorganisms remains, surgical treatment will be ineffective. Corsodil has a good effect after surgical treatment. Considering the relative local unresponsiveness, the most reliable criterion for the effectiveness of treatment is microbiological analysis of the contents of periodontal pockets and tissue biopsies. It follows from this that in some cases it is advisable to treat such patients only in specialized institutions that have the necessary facilities. And of course, no treatment can be effective, especially when it comes to long-term prognosis, if there is no proper oral care.
One of the diseases that is based on the degenerative process is periodontal disease. Periodontal disease is an atrophic-dystrophic process in periodontal tissues. This disease has rather sparse symptoms. What brings patients to the doctor?
This is mainly a cosmetic defect, expressed in the fact that the roots of the teeth are exposed and their clinical crown is enlarged. Patients complain that “the gums sag and the teeth become long,” this especially bothers them in the frontal region. In some cases, patients are bothered by itching in the gums, as well as pain from the exposed necks of the teeth.
During examination, most often, uniformity of atrophic manifestations is observed in the area of all teeth and the involvement of dental tissues directly in the process - this is expressed in the presence of so-called wedge-shaped defects. This pathology is characterized by a slow course and relative asymptomaticity.
The cause of this pathology is unclear; it is considered either as a premature development of involutional processes, or as a manifestation of general disorders in the periodontium, that is, a syndrome or symptom of general disorders. However, a very specific and clearly defined clinic makes it possible to distinguish this form of the disease.
There is no adequate treatment for periodontal disease because the cause of the disease has not been established. The doctor provides only symptomatic treatment - eliminates increased tooth sensitivity, prescribes massage or automassage of the gums to correct trophic disorders, and also fills wedge-shaped defects. In an effort to meet the wishes of patients, some surgeons perform vestibuloplasty operations. However, this should not be done, since the effect of such interventions is very short-lived.
What is actually effective is the use of products that eliminate the pain sensitivity of the exposed cheeks of the teeth. To do this, use fluoride varnish, fluogel, and baking soda powder. Currently, Sensodyne paste has appeared on the market, which successfully relieves increased sensitivity of teeth, and the patient can use it independently. The doctor should warn patients with this disease that they should not use a hard brush or make horizontal movements so as not to increase the depth of the wedge-shaped defects.
Tumor and tumor-like lesions are also among the diseases that are difficult to predict, since they develop only in individuals with a predisposition to this process. And the impetus for the beginning of the development of the process can be hormonal changes, in particular the accumulation of somatotropic hormone during puberty or pregnancy, the presence of a chronic traumatic factor, and previous inflammation. However, all of these are just additional risk factors that provoke the development of such lesions in individuals predisposed to this process.
Treatment and prevention measures consist of eliminating trauma, inflammation and, if necessary, surgical removal of overgrown tissue (for gingival fibromatosis, hypertrophic gingivitis, epulis, interradicular granuloma). Currently, another rather serious factor has emerged that provokes the development of this kind of pathology: the use of anabolic steroids by young people when engaging in bodybuilding and professional strength sports. The doctor’s capabilities here are modest: clarification and advice.
What really leads to a positive result in such cases? Maximum thorough oral hygiene, the use of effective antiseptic and antibacterial rinses by the patients themselves after an active treatment course.
Etiology and pathogenesis (causes and development) of periodontal diseases
Calculus
The main point in the development of gum diseases such as gingivitis and periodontitis is dental plaque (plaque), which turns into tartar (calculus).
Photo 3. Soft plaque (plaque). Marginal periodontitis.
It is believed that organic soft dental plaque, which is formed from food debris due to poor hygiene, is gradually saturated with calcium from saliva and serum exudate of the gum pockets and is converted into hard tartar.
The latter can be of different hardness and color, which is determined by its composition. It consists of 18-25% organic matter (microbes and dead cells) and 75-82% inorganic matter (calcium, phosphorus, metal salts).
Tartar causes traumatic compression of the gums and prevents the cleaning of the periodontal pocket, promoting the development of microbial agents.
Microorganisms diffuse deep into periodontal tissues, lingering on the surface of the basement membrane and further into the bone tissue of the alveolar process.
Traumatic closure of teeth
In the absence of part of the teeth, in case of violation of the position of the teeth, in case of partial destruction of teeth and other traumatic factors, the remaining teeth are subjected to excessive and inadequate load. The latter, in turn, destroys the periodontium of the teeth.
Improper functioning of the temporomandibular joint (TMJ).
The ANS may be a significant factor in the development of gum disease.
Medical Internet conferences
The need for orthodontic treatment has increased significantly in recent years. But at the same time, the number of dental diseases that are directly related to the presence of structures in the oral cavity is growing [3]. This is explained by the fact that orthodontic appliances are not indifferent to the human body and, when exposed to the oral mucosa, change the activity of salivary enzymes, causing dental diseases. These complications of orthodontic treatment lead to changes in homeostasis: the destruction of normal microflora or a disproportionate change in the number of components of the oral microbiocenosis, which ultimately leads to the development of dysbiosis and the occurrence of both inflammatory processes in periodontal tissues and processes of demineralization of hard dental tissues [2, 7, 10, 12, 13].
The main etiological factor causing inflammation in periodontal tissues, as well as dental caries, is dental plaque. In patients undergoing orthodontic treatment, the cariogenic situation in the oral cavity increases due to the fact that around the elements of the orthodontic structure, in the spaces between the teeth and in the cervical areas, due to difficulty in hygiene, food residues accumulate in which microorganisms multiply, producing acids in the process of their vital activity, leading to a decrease in the pH of the oral fluid, increased enamel permeability and demineralization [5, 9, 11, 14–16].
Plaque contributes to the development of not only caries, but also periodontal disease. Pathological processes in the periodontium begin with gingivitis, which is manifested by redness and bleeding. Bleeding gums during orthodontic treatment occurs quite often when brushing teeth, as well as while eating solid foods. If left untreated, gingivitis progresses to periodontitis. With periodontitis, tooth mobility appears, pathological periodontal pockets form, and patients may be bothered by bad breath.
To avoid complications during orthodontic treatment, it is necessary to follow the rules of hygiene and a balanced diet. It is very important to teach the patient the rules of hygiene and monitor its implementation even before installing the device. It should be explained to the patient that toothpaste and toothbrush alone will not be enough to maintain the oral cavity in good condition. It is necessary to use a soft toothbrush and a special paste to clean the surface of the removable appliance from plaque, a gel or mouthwash for daily use that dissolves dirt and destroys bacteria that accumulate on the appliance. Once a week you need to soak the device in cleaning concentrate for more thorough care. An integral part is the use of the following additional hygiene products: brushes - for cleaning interdental spaces and removable orthodontic appliances; floss - will clean the interdental spaces and gum pockets; irrigator - for thorough cleaning of dental spaces, cleansing the surface of teeth from newly formed plaque and improving blood circulation in soft tissues; plaque indicator tablets – allow you to evaluate the quality of hygiene.
During meals, it is necessary to remove the orthodontic device and put it on after carrying out hygienic measures [1, 6].
It is well known that after tooth eruption, active mineralization of the enamel occurs within 2–3 years. Therefore, it is advisable to carry out local preventive measures during this period. One of the most effective modern methods of preventing dental caries, stimulating the process of “maturation” of enamel, is fissure sealing. For this purpose, special materials are used - sealants. Most sealants contain silanes - fluorine-containing substances that split off fluoride ions over a long period of time, which diffuse into the layers of hard tooth tissue adjacent to the sealants, stimulating their mineralization. The use of sealants leads to stabilization of the carious process for 1–9 years.
The next important point is diet correction. It is necessary to reduce the consumption of easily digestible carbohydrates (chocolate, sweets, flour products), and, on the contrary, increase the consumption of foods containing easily digestible Ca2+ (milk, low-fat cottage cheese) in order to increase the mineralizing function of saliva. At the same time, it is useful to consume foods that help shift the pH to the slightly alkaline side, for example, cheese [4, 8, 16].
Such an integrated approach to prevention will help improve the hygienic state of the oral cavity and reduce the incidence of dental caries and periodontal diseases in patients during orthodontic treatment.