Sometimes tooth extraction is the only possible help that a doctor can provide to a patient. Remnants of rotting dental tissue decomposed due to advanced caries, roots affected to the top. Removal is seen as a salvation from all problems, including the pain that haunts the patient. But the source of pain has been successfully eliminated. The anesthesia works well. The patient thanks the surgeon and leaves happy. And after some time he returns with a swollen cheek. A tumor after tooth extraction - normal or pathological, why it forms, and what to do with this post-surgical phenomenon.
Tumor after tooth extraction
Dental treatment
If the dentist does not treat the tooth correctly or completely, it can cause swelling in the cheek.
Causes:
- Allergic reaction.
It appears in the patient as a result of intolerance to the components of the filling. To eliminate swelling, you should visit a doctor and replace the installed filling with a hypoallergenic one.
- Removal of a tooth.
If the cheek is swollen after surgery, then the patient probably ignored the doctor’s recommendations and ate solid or hot foods.
- Nerve removal.
Swelling occurs if part of the nerve is not removed. It is important to see a dentist immediately so as not to lose a healthy tooth.
- Gum section.
Usually required to remove accumulated pus. If the swelling does not subside while taking anti-inflammatory drugs, this may be a serious symptom that requires the attention of a specialist.
Swelling that is not dangerous
For each patient, tooth extraction is a serious surgical action aimed at healing through injury. When a tooth is extracted, blood vessels rupture and gum tissue is damaged. The longer and more difficult the surgery, the longer the damaged tissue will remain swollen and painful.
Important! Even uncomplicated extraction of a single-rooted tooth leads to swelling, which naturally subsides when impaired blood circulation returns to normal. Physiological tumor of the gingival tissue after extraction is not a complication and does not pose a threat to the patient’s health.
When edema develops, it is important to understand whether the situation is within normal limits or requires medical intervention
Gum swelling is not dangerous in the following cases:
- general condition, despite the presence of a tumor, is satisfactory;
- the temperature is normal or slightly increased only on the day of removal;
- the tumor is localized in one place and does not spread to facial tissues;
- the pain is present, but is fading and lasts no more than five days;
- immediately after the operation, the cheek swells, but no increase in pain is observed, and the swelling subsides within a few hours;
- facial skin or oral mucous membranes are of normal color, without redness;
- there is no tissue decay, there is no unpleasant odor from the gums, and there is no unpleasant taste in the mouth.
As for postoperative pain, it is always present in the background. Simple removal is accompanied by aching pain for three to four days. A difficult one can cause pain for a week.
Pain after tooth extraction is common
The main evidence that everything is normal is a gradual decrease in swelling and pain. If everything happens this way, you don’t need to do anything about the swelling, just watch it. You can take painkillers for pain.
What to do if your cheek is swollen
To reduce swelling, you can use one of the following tips:
- Rinse your mouth with a solution of salt and soda.
This remedy has an antiseptic effect and helps destroy pathogens. You can enhance the effect by adding a couple of drops of iodine to the solution.
- Use chamomile infusion to rinse
, sage or other medicinal herbs that have anti-inflammatory properties.
- Apply a cold compress to the swollen cheek
if the swelling is caused by a bite or mechanical injury. This method is contraindicated in patients who have an elevated body temperature or a tumor that develops due to inflammatory processes. Warming compresses are not recommended.
- Lotions with aloe or Kalanchoe juice.
A cotton wool soaked in the juice of the plant is applied to the inside of the affected cheek.
If the described methods do not eliminate the problem, you should seek help from a doctor. The day before, you should not take painkillers and anti-inflammatory drugs, so as not to complicate the diagnosis.
How to treat gumboil on the cheek
Once a tumor develops, antibiotics are often indispensable. The dentist selects them taking into account the stage of the pathology and the characteristics of the body. Antibiotic therapy should be completed to the end, otherwise further treatment will be greatly complicated.
If surgery is required, all activities are carried out in a dental clinic. For any complication, the patient is given local or general anesthesia. The gum is incised and the accumulated pus is completely pumped out. A drainage is placed to quickly remove fluid. The patient is prescribed antibiotics to allow the soft tissues to recover faster. In case of severe damage, the gum is sutured. In the absence of complications, this is not required.
How to remove swelling from the gums through surgery:
- In case of complicated flux, urgent hospitalization in a dental clinic and an operation performed by a dental surgeon are necessary.
- If an inflammatory process is diagnosed due to dental problems, endodontic therapy (cleaning and filling the canals) or root removal will be required.
- Broad-spectrum antibiotics are prescribed to treat infection in many situations. In case of serious complications, combination drugs are used to treat severe swelling, selected taking into account the sensitivity of the pathogens.
- Surgical treatment - incision of the abscess (on the face and oral cavity - the incision is made in both areas), removal of purulent discharge, treatment with disinfectants, installation of drainage. In severe cases, general anesthesia is used.
- Additional therapy - analgesics to eliminate discomfort, antipyretic drugs, large amounts of fluid (if necessary, fluid is introduced into the body by infusion during hospitalization).
Chronic pathology often occurs without pronounced symptoms, pus appears gradually. In this situation, the dentist uses a therapeutic approach, both surgical and conservative. Surgery can be replaced with herbs or antibiotics, or used as an additional treatment after consultation with a specialist.
Swelling of the cheek does not always indicate the presence of a serious pathology.
A tumor after depulpation is normal and does not require serious treatment. When the gumboil gradually grows, pain is observed against this background, and the help of a dentist is required. In case of serious complications, surgical intervention while taking antibiotics is indicated. The doctor's consultation
Swelling in the cheek area, causes
The most common dental causes of cheek swelling are:
- advanced caries;
- complication of pulpitis;
- complication of gingivitis;
- periostitis, periodontitis and other diseases of teeth and gums.
If you suspect flux, call: 8 (495) 558-88-77
Flux is inflammation of tissues of various origins, for example, periostitis, an inflammatory process in the periodontal gap - periodontium. Such inflammation can occur in acute and chronic forms; the chronic form can periodically enter an exacerbation phase and then subside again.
By origin, periostitis is as follows:
- infectious;
- non-infectious;
- spicy;
- chronic;
The main role in the development of flux of infectious origin belongs to microorganisms, as well as their toxins. Microbes penetrate into the periodontium through the root canal, periodontal pocket, as well as through the blood or lymph flow.
Most often, flux is caused by an infection that enters through the root canal and is a consequence of acute diffuse and chronic gangrenous pulpitis, as well as pulp necrosis.
Microorganisms and their toxins, penetrating into periodontal tissue, cause dangerous acute inflammation
Non-infectious periostitis/periodontitis (fluxes) can develop as a result of trauma (blow, bruise, periodontal trauma after pulp extirpation, sharp, uncomfortable biting on a tooth; cracking nuts, gnawing bones) or chronic microtrauma (smoking pipe, brass band instruments, biting threads, pressing on the tooth with a pencil, pen, etc.); also as a result of the influence of medications - the ingress of potent substances into the periodontium during the expansion of root canals (trilon B, aqua regia), their sterilization (formalin, silver nitrate, etc.) and in the ingestion of arsenic paste.
Potential complications leading to swelling
When swelling does not go away for more than seven days, we can talk about the constant progression of inflammation. In this case, it is recognized that the patient has complications. It is very important to establish their causes and nature, and then quickly eliminate them.
There are several most common types of complications that patients usually complain about:
Alveolitis
There is always a small blood clot in the hole that remains in place of the extracted tooth. This is a natural reaction of the body aimed at preventing infection. The clot does not allow bacteria to penetrate inside - the wound gradually heals and heals.
But sometimes the clot is removed. As a result, the tissues remain defenseless, infection can occur and pus can begin to accumulate. In this case, inflammation will become more and more intense and will cover large areas.
Inflammation of bone tissue
Not the most common complication, but you won’t be able to insure against it either. It is usually characterized by the appearance of severe swelling that begins to spread throughout the jaw. In this case, the patient experiences severe pain and is practically unable to open his mouth or chew food normally.
The big danger is potential blood poisoning. Therefore, at the first signs of worsening inflammation, you should contact your doctor as soon as possible.
Gum abscess
Characterized by severe suppuration. If it is not addressed, you may lose other teeth in the row.
Flux
Also called “periostitis of the jaw” in the medical community. An intense inflammatory process, which, in addition to swelling, also manifests itself as severe pain in the jaw, radiating to the temples. The temperature rises and the patient feels very weak. Among the dangers are transition to a chronic form and the development of osteomyelitis.
Neuritis
In this case, severe damage to the facial nerve occurs. Not only the area next to the extracted tooth swells, but also the cheeks, tongue, and larynx.
Why does cheek swelling occur?
A common cause of edema is odontogenic periostitis, or gumboil. The inflammatory process of the periosteum is accompanied by the formation of purulent contents at the base of the root. The causes of gumboil are the spread of infection from a diseased tooth - carious or pulpy. In this case, only surgical treatment of periostitis, an incision in the gum and cleaning out the pus will help relieve swelling.
Another cause of cheek swelling is gingival cysts. If the cystic formation is localized not strictly under the root, but on the side, the gums and along with it the patient’s cheek swell. Getting rid of cysts involves performing tooth-preserving operations or, in advanced cases, tooth extraction. Often the cyst itself does not cause swelling, but after surgery to resect it, the patient receives swelling, which goes away within 2-3 days.
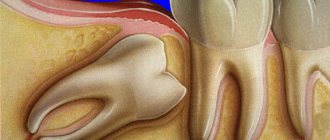
Patients with impacted and dystopic wisdom teeth often suffer from swelling during periods when the tooth is actively trying to erupt.
The dangers of flux and the dentist's tasks
It is the identification of such foci and their elimination, especially in persons suffering from inflammatory processes of internal organs and in pregnant women, that is one of the essential tasks of a dentist. Untimely sanitation of the oral cavity or its absence in the presence of teeth affected by chronic periodontitis can lead to the development of a number of more severe inflammatory processes, the first of which is acute purulent periostitis.
Purulent periostitis
This disease is an acute purulent inflammation of the periosteum of the alveolar process of the jaw and accounts for up to 40% of complications of odontogenic infection, mainly chronic periodontitis. The cause of the development of this disease is most often large molars, which are primarily affected by the carious process.
The clinical picture of acute purulent periostitis is diverse and depends on the nature of the microflora, localization and extent of the inflammatory process. When the upper jaw is affected, the external manifestations of acute inflammation, in particular hyperemia, infiltration and swelling of soft tissues, are usually more pronounced than when the flux is localized in the lower jaw. However, the phenomena of general intoxication are more pronounced when the alveolar process of the lower jaw is affected, which is due to the difference in the anatomical and topographic relationships of soft tissues and jaw bones.
When examining the oral cavity, smoothness or swelling of the transitional fold of the mucous membrane of the vestibule of the oral cavity, its hyperemia, and sharp pain when touched by the dentist’s hands or instruments are noticeable.
It should be borne in mind that the pain in the “causal” tooth due to the release of exudate (liquid released into the tissue or cavity of the body from small blood vessels during inflammation) beyond the periodontal gap subsides to a certain extent, but slight mobility of the tooth appears. This circumstance sometimes serves as a justification for delaying visiting a doctor and as a cause of aggravated course of the inflammatory process in the future.
The diagnosis of “acute purulent periostitis” is an absolute indication for surgical intervention in the form of opening and drainage of the periosteal purulent focus and removal of the “causal” tooth.
Options for non-drug treatment (physiotherapy) depend on the patient’s general condition, age, and concomitant chronic diseases. In the latter case, the volume and nature of drug treatment is determined by the dentist of the appropriate profile. It is especially important to carry out adequate treatment in patients suffering from rheumomyocarditis, diabetes mellitus, nephritis and some other chronic diseases.
Another complication of chronic granulating periodontitis is the development of acute odontogenic osteomyelitis , accompanied by the formation of phlegmons and abscesses of the cellular spaces of the face and neck.
These complications of flux are the most severe and dangerous result of the progression of odontogenic infection, and depending on the location and nature of the microflora, they can lead to severe complications including the development of sinus thrombosis and mediastinitis.
It is their timely diagnosis in somatic patients that largely determines the outcome of the disease.
The clinical manifestations of phlegmon are different and depend on the location of the flux (deep, superficial), the nature of the pathogen (aerobic, anaerobic flora), body resistance, concomitant diseases, age, etc.
Today, persistent, sluggish chronic necrotic processes in the bone and soft tissues of the face often occur against the background of drug addiction.
Deep phlegmons of the pterygomaxillary, infratemporal, peripharyngeal spaces are manifested by sharp pain of the corresponding localization, severe manifestations of general intoxication up to acute intoxication psychosis, severe inflammatory contracture of the masticatory muscles, pain when swallowing, with an almost complete absence of external manifestations: hyperemia, infiltration, fluctuations, etc. .
Underestimation of certain symptoms of gumboil can lead to a delay in seeking dental care, ineffective therapy and progression of the inflammatory process.
Flux symptoms
Clinical manifestations of acute periodontitis/periostitis are quite characteristic. Flux manifests itself as sharp pain in the tooth area, intensifying even with light pressure on it. Swelling and redness of the lips, cheeks, enlarged gums, and the tooth is often mobile.
There is an unpleasant odor from the mouth, and sometimes fistulas on the gums. A characteristic sign of gumboil is the appearance of independent pain, weak at first, then intensifying, becoming pulsating and tearing. Its difference from pain with pulpitis is that it is strictly localized and becomes sharp when pressing on the diseased tooth, especially in the form of tapping. The closing of teeth is so painful that many people refuse to eat even liquid food.
Clinical manifestations of acute periodontitis/periostitis are quite characteristic. Flux manifests itself as sharp pain in the tooth area, intensifying even with light pressure on it. Swelling and redness of the lips, cheeks, enlarged gums, and the tooth is often mobile.
There is an unpleasant odor from the mouth, and sometimes fistulas on the gums. A characteristic sign of gumboil is the appearance of independent pain, weak at first, then intensifying, becoming pulsating and tearing. Its difference from pain with pulpitis is that it is strictly localized and becomes sharp when pressing on the diseased tooth, especially in the form of tapping. The closing of teeth is so painful that many people refuse to eat even liquid food.
It is also possible to increase body temperature to 37.5-38.0°C. Severe pain and difficulty eating food force the patient to see a dentist within the next few hours from the moment of illness.
Chronic form of periodontitis
In chronic forms of periodontitis, a different picture is observed. The most formidable and insidious in its course and possible complications is chronic granulating periodontitis and exacerbation of its course. The pain reaction is mild, but often in the vestibule of the oral cavity, in the projection of the apex of the root of the affected tooth, a fistula periodically opens with small purulent discharge.
When the fistula is closed during periostitis, swelling and hyperemia of the mucous membrane in the area of the flux and pain when pressing on the diseased tooth are possible. Chronic granulating periodontitis is diagnosed based on a comparison of clinical manifestations with X-ray data, which shows destruction of the periodontal gap and changes in the jaw bone in the form of “tongues of flame” in the area of the apex of the tooth root. The purulent process in the medullary spaces of the jaw adjacent to the periodontium leads to the spread of infection over a considerable distance.
The vital activity of pathogenic microflora during the long-term existence of a chronic pathogenic focus ultimately leads to odontogenic chronic sepsis. This provokes the emergence, formation or exacerbation of chronic infectious diseases of the heart, liver, kidneys and other organs.
The presence of such infectious foci can dangerously affect the course of pregnancy at any stage; complications such as infection of the female genital area, miscarriage, and disruption of the formation of fetal tissue occur.
Why does alveolitis occur after wisdom tooth removal?
Edema, as a consequence of alveolitis, can occur for various reasons, namely through the fault of the doctor or the patient himself.
Causes of edema when the doctor is to blame:
- A cyst remained under the extracted tooth.
- The doctor incorrectly applied stitches, which came apart and exposed the alveolar bone.
- The doctor did not prescribe an antibiotic to the patient after the removal of a wisdom tooth due to a purulent process.
- The doctor left a foreign body in the hole - pieces of a tooth, bone, instrument, etc.
- Causes of edema, when the patient is to blame:
- The patient did not comply with recommendations for oral hygiene in the postoperative period.
- The patient rinsed his mouth vigorously, which led to the flushing out of the blood clot covering the wound.
- The patient chewed hard food on the side of the extracted tooth, which led to suture dehiscence and exposure of the alveolar bone.
- The patient did not take antibiotics prescribed by the doctor after a complex wisdom tooth extraction.
Whatever the cause of pathological swelling, it is necessary to get rid of it under the supervision of experienced specialists. Call ICDI ROOTT toll-free at 8 800 775–26–37 and make an appointment with a doctor at any of the clinics – on Dmitrovskaya and Proletarskaya. We will provide high-quality treatment - therapeutic, physiotherapeutic or surgical - to stop the processes that cause swelling of the soft tissues of the face.
When is swelling a sign of pathology?
- If swelling does not appear the next morning, but much later (on the third or fourth day);
- If swelling is accompanied by increasing pain;
- If, against the background of edema, the patient’s temperature rises;
- If the swelling is so severe that it makes speech and swallowing impossible;
- If there is a putrid odor from the mouth.
The listed symptoms may indicate that the patient has developed alveolitis. When wisdom teeth are removed, this phenomenon is not so rare, and according to statistics it happens in 20% of cases.