Alveolitis is an inflammation of the socket (alveoli) left after tooth extraction. This pathology does not always develop; its development depends on many factors. The disease is characterized by severe pain in the area of the hole formed after surgery, general weakness, fever, headache, enlarged submandibular lymph nodes, bad breath and other unpleasant symptoms.
Alveolitis is not only physically painful, but also a dangerous disease. In the absence of proper treatment for several days, the inflammatory process can result in limited osteomyelitis, purulent melting of the jaw bone, and then surgical intervention will be required again.
With timely diagnosis of pathology and proper sanitation of the socket, the treatment prognosis is favorable. The main thing is to detect the symptoms of the disease in time and begin to treat it.
Classification
Depending on the nature of the healing of the hole, dentists distinguish several main forms of dental alveolitis:
- Serous. The initial stage of the disease usually appears 2–3 days after tooth extraction. This form is characterized by continuous pain that worsens while eating. Although the patient does not yet complain of feeling unwell, his lymph nodes are not enlarged, but he already feels that the disease is progressing.
- Purulent. If the serous form of alveolitis is not treated, the disease turns into a purulent form. Most often it is diagnosed 6–7 days after tooth extraction. The painful sensations can no longer be ignored, the pain intensifies, radiating to the ear or temple. Exploring the affected area also causes severe pain. Purulent alveolitis is characterized by a dirty gray coating inside the socket, significant swelling around the wound, thickened alveolar process and other problems. The patient's general health deteriorates significantly. Lymph nodes enlarge and become painful on palpation. Often the patient cannot even eat or open his mouth.
- Hypertrophic. At this stage, the symptoms of the disease subside. The patient notes a decrease in body temperature, improved well-being and decreased pain. However, at the hypertrophic stage, dangerous tissue proliferation occurs, which is clearly visible upon examination. When touched, pus is released from the inflamed area, and the mucous membrane acquires a bluish tint.
Ask a Question
Complications
If you do not take measures to disinfect the hole in a timely manner, you may encounter a number of unpleasant consequences.
Among the dangerous complications it should be noted:
- Inflammatory process in the tissues of the periosteum. The disease is accompanied by severe pain in the jaw and swelling of the gums. The intensity of discomfort increases at night and when a person eats. The inflammation gradually spreads to the neck, lips and chin. Advanced stages of the disease occur with fever, headaches and the formation of white plaque in the alveoli. The pathology is eliminated by washing the wound with antiseptic solutions and taking antibiotics.
- Alveolitis. It may be asymptomatic, but most often manifests itself as pain. At first the symptom is aching in nature, and then pulsating and constant. More often, the disease manifests itself after the removal of a wisdom tooth. Another sign of a problem is bad breath. Over time, it becomes difficult for the patient to open his mouth, and severe redness is observed in the gum area. Therapy is carried out using anti-inflammatory medications and drugs with antibacterial effects.
- Abscess. A complication occurs if the soft tissues of the mouth are injured during tooth extraction. Purulent processes develop in the area of the injuries received. The situation is aggravated if the patient does not comply with postoperative recommendations.
Osteomyelitis is one of the dangerous complications of tooth extraction
Causes of inflammation
The disease can develop only after tooth extraction. Most often, the hole formed after removal heals within a day after the operation, and the patient feels better. But if the blood clot that covers the open wound moves or becomes deformed, an infection can penetrate into the hole, in which case alveolitis of the gums develops. As a result, the surface of the wound heals for a long time, and the patient suffers from complex discomfort.
Predisposing factors for the development of inflammation:
- Surgical injuries during complex removal. The more complex the operation, the more pronounced the postoperative inflammation of the bone tissue will be, and the more likely the release of direct plasminogen activators.
- Complex extractions associated with tooth segmentation, osteotomy, detachment of the mucoperiosteal flap. Complex operations increase the chance of developing alveolitis 10 times.
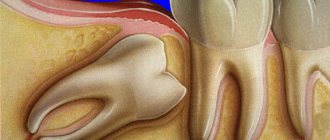
- Removal of wisdom teeth. The denser, less vascularized bone tissue adjacent to the figure eights is prone to the formation of dry sockets.
- General diseases of the patient. Alveolitis often occurs against the background of concomitant diseases. For example, patients with diabetes mellitus or immunocompromised patients are more susceptible to alveolitis due to impaired healing processes in the tissues.
- Taking oral contraceptives. The estrogen contained in these drugs may indirectly enhance the fibrinolytic process, causing the breakdown of the blood clot.
- Smoking. The direct connection between smoking and alveolitis has been repeatedly proven clinically. According to studies, the risk of socket inflammation in smokers increased 4-5 times compared to non-smokers. The incidence increased by more than 20% in patients who smoked 1 pack per day and by 40% in patients who smoked immediately before and after surgery.
- Dislocation of a bunch. If the socket is handled carelessly and there is negative pressure (for example, due to drinking through a straw), alveolitis may develop.
- Bacterial infections. Dentists agree that bacterial infections are the main risk factor for dry socket.
- Poor oral hygiene. The incidence of alveolitis increases significantly with poor oral hygiene.
- Excessive use of local anesthetics. According to some studies, excessive use of an anesthetic with a high concentration of a vasoconstrictor can provoke ischemia and make it difficult for the socket to fill with blood. This condition also increases the risk of alveolitis.
In fact, alveolitis is a fairly rare disease. According to statistics, it affects approximately 3% of patients who have undergone tooth extraction surgery. More often than not, the socket is not formed properly when lower incisors and molars are removed.
But alveolitis is especially common when removing lower wisdom teeth: according to experts, in approximately 20% of cases, the removal of “eights” with difficult eruption is complicated by alveolitis. In addition, it is believed that the risk of developing the disease is inextricably linked with age. This is explained by the fact that metabolism slows down, immunity is weakened, and the regenerative abilities of the body deteriorate.
Why does a tooth abscess develop?
The main cause of abscess development is bacteria. They are always present in the oral cavity, but in order for an infectious process to develop, provoking factors are needed. The development of an abscess can be provoked by:
- Violation of the rules of daily hygiene. Bacteria multiply quickly in the favorable environment of dental plaque. When there are a lot of them, a pathological process develops.
- Dental procedures. During tooth extraction, an antiseptic treatment of the oral cavity is performed. When this treatment is insufficient or the procedure was carried out in violation of antiseptic rules, pathogenic bacteria can penetrate the tissue.
The risk of developing a tooth abscess increases if the patient has a weakened immune system or has systemic diseases, for example, diabetes, cancer. Chronic tonsillitis often provokes the development of a purulent process. This is due to the fact that with chronic inflammation of the upper respiratory tract, there is a focus of infection in the body. It may spread to other areas.
Patients with dental problems are also at risk:
- Caries.
- Mechanical damage to the enamel (chips, cracks).
- Periodontal diseases.
- Gingivitis.
Symptoms of alveolitis
As a rule, the patient ignores the first symptoms of inflammation without due attention, considering them to be the norm after surgery. After tooth extraction, as already noted, pain within 24 hours is considered normal. As the hole heals, the pain subsides and completely disappears after a few days.
If the patient develops an inflammatory process, then the unpleasant sensations do not subside after a day or two, and 3–5 days after the operation, severe, throbbing pain in the socket occurs, which intensifies as the infection develops.
With alveolitis, patients may complain of both unbearable and moderate pain. Pulsation and pain are focused, as a rule, only in the removal area. However, in rare cases, the pain radiates to half of the face.
Other characteristic symptoms of alveolitis are:
- a sharp rise in body temperature;
- tooth sensitivity to hot/cold food;
- enlargement of the submandibular lymph nodes;
- decreased appetite;
- increased salivation.
In rare cases, the disease causes weakness, increased fatigue, and secondary infectious foci appear on the oral mucosa.
First aid
If after tooth extraction there is mild inflammation and there is no suppuration, it can be removed at home and prevent the spread of discomfort.
- For 30 minutes after tooth extraction, do not remove the antiseptic tampon placed in the hole.
- Do not eat for 2 hours after removal.
- If there is bleeding after tooth extraction, apply a cold compress, such as an ice cube, to the gum.
If a doctor prescribes rinses for the treatment of inflamed gums, they should be done as carefully as possible. It is important not to wash the protective clot out of the hole. On the first day after surgery, you should avoid rinsing, and on the second day, use antiseptics and herbal decoctions.
During the healing period, it is also recommended to avoid food and drinks that are too cold or too hot, and never touch the socket with your fingers, toothpicks or other foreign objects.
A reliable rinse that will help eliminate gum inflammation is the ASEPTA ACTIVE mouth rinse. This unique two-component rinse with a combination of chlorhexidine + benzidamine has antimicrobial, anti-inflammatory and analgesic effects and provides an immediate anesthetic effect.
Diagnostics
The main symptom of the disease is the appearance of acute pain, which does not subside either 24 hours or 2–3 days after tooth extraction. Sometimes a dentist can identify chronic alveolitis during routine oral examinations. In this case, an empty socket without granulation tissue appears in place of the impacted tooth. The bone is already visible at the bottom of the hole.
The dentist will be able to determine the presence of tissue changes during the examination; radiography and radiovisiography of the affected area may also be prescribed.
Treatment of alveolitis
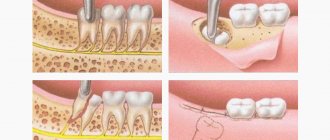
When the socket becomes inflamed, the main thing is to eliminate the source of infection, prevent the development of inflammation and preserve the dentition. In order to alleviate the patient’s condition, the dentist uses the following therapy methods:
- Mechanical cleansing of the hole, washing out purulent residues with a solution of nitrofural or hydrogen peroxide.
- Anesthesia of the hole. The pain syndrome is relieved with the help of local applications with anesthetics and analgesics. To do this, the doctor applies the lotion for half an hour and then removes it to prevent the proliferation of microbes in the area. The dentist will advise the patient to repeat the procedure several times a day. Taking painkillers orally is not recommended.
- Taking antibiotics. In the presence of concomitant diseases, alveolitis is treated with antibiotics.
With the right approach, the signs of alveolitis subside 2-3 days after the start of treatment. If therapy was not started on time, residual pain may drag on for 2–3 weeks.
With the permission of the dentist, additional treatment of alveolitis with folk remedies is possible:
- Sage rinses. To prepare the solution, brew a large spoonful of dry sage in 250 ml of boiling water, leave the mixture for an hour, wrapping the container in a towel. After this, the liquid should be filtered and used for rinsing.
- Gargling with chamomile flowers. To prepare the composition, brew a large spoonful of chamomile flowers in a glass of water for 15 minutes, insulating the container with a towel. The infusion should be strained and rinsed your mouth up to 12 times a day.
- Poplar buds. To prepare, take half a glass of buds, pour into a glass container and pour in 500 ml of vodka. The product should be infused for 10 days in the dark and cool, then filtered, soaked in cotton swabs and applied to the inflamed area.
- A soda rinse solution can also be an effective addition in the treatment of alveolitis. You should take a large spoonful of powder in a glass of warm water or mix soda with water to obtain a paste-like mass, which then needs to be used to treat the hole.
- Burdock leaves. To prepare a medicinal decoction of burdock leaves, you need to pour 20 grams of raw material with 2 glasses of water, and then simmer the mixture over low heat for about 40 minutes. The resulting solution should be cooled and filtered, and then used for rinsing.
- Aspen bark. Pour 1 tablespoon of crushed aspen bark into one glass of boiling water. It is important to leave the solution in an airtight container for 3 hours, and then use 100 ml of strained warm liquid at least 3 times a day.
- Anise infusion. To prepare the infusion, pour 1 tablespoon of anise into 200 ml of boiling water, and then keep in a thermos for 50 minutes. The liquid should be filtered and used to rinse 3 times a day.
Prevention
The best prevention of pathology after tooth extraction is to be attentive to yourself and follow all the surgeon’s recommendations. While the hole is healing, give up bad habits, eating too hot, spicy, sweet foods, and if possible, switch to pureed foods. And if you suspect inflammation, contact your dentist as soon as possible.
Under no circumstances should the first symptoms of alveolitis be ignored. Against the background of inflammation, more serious problems may arise:
- Phlegmon is an acute diffuse purulent inflammation.
- An abscess is a purulent inflammation of tissues with their melting.
- Osteomyelitis is a purulent-necrotic process that can develop in the bone and bone marrow, as well as in the surrounding soft tissues.
- Periostitis is inflammation of the periosteum.
- Sepsis is a severe systemic inflammatory reaction.
- Tissue necrosis is local tissue death.
Modern methods of treating alveolitis make it possible to quickly relieve the symptoms of inflammation and avoid the complex consequences of the disease. The sooner the patient consults a doctor, the less likely it is to develop complications.
Types of abscess
The type of abscess is determined by its location. Based on this feature, periodontal and periapical types are distinguished. Both can occur in acute or chronic form.
- Periodontal abscess. Develops in the space between the gum and the crown of the tooth. In the acute form there are pronounced symptoms - an abscess on the gum, severe pain when closing the teeth. In the chronic form, such pronounced symptoms are not observed. In case of chronic periodontal abscess of a tooth, a fistula develops at the site of purulent inflammation.
- Periapical abscess. The source of infection is located inside the tooth. Often this type of disease develops as a complication of periodontal disease. The process proceeds as follows. Pus begins to accumulate at the top of the tooth root. If the suppuration is deep and the pus cannot come out, it continues to spread inside the gums, under the mucous membranes. The bone is gradually affected and begins to deteriorate.
Treatment of alveolitis in STOMA clinics
Surgeons at STOMA clinics are required to examine patients and give recommendations on how to care for the hole formed after tooth extraction. If problems arise after extraction, the patient can always call the clinic and clarify whether inflammation has really begun and what to do to reduce pain.
At any time after removal, the patient can contact our clinics. The attending surgeon will examine him and prescribe appropriate therapy.
Feel free to call us at any time and consult about your condition. The sooner we start treating alveolitis, the lower the risk of complications.
SO WHAT TO DO IF PUS APPEARS AFTER TOOTH EXTRACTION?
The only correct solution in this situation is to contact a dentist. Before visiting the clinic, you can take painkillers, rinse or irrigate with herbal infusions, antiseptics or anti-inflammatory agents (this must be done carefully so as not to damage the clot, if it is still preserved). You should not delay visiting a medical facility for a long time, since the spread of infection can lead to osteomyelitis, abscess and other dangerous complications.
After diagnosis, doctors usually carry out:
- eliminating the cause of infection of the socket (for example, freeing it from bone fragments);
- cleansing from purulent masses;
- if necessary, suturing the wound;
- prescription of antibiotics and anti-inflammatory drugs.
To minimize the likelihood of complications, it is important to choose only reliable medical institutions for dental procedures. In addition, it is necessary to carefully follow the doctor's recommendations regarding oral care after the intervention.