Osteomyelitis of the jaw is a dangerous inflammatory disease that is caused by infection. A purulent-necrotic process develops on the tooth bone - most often on the lower jaw. Next, the inflammation affects the bone tissue of the head and spreads to soft tissues - gums, salivary glands, skin, chewing and facial muscles. In severe cases, pus forms and necrosis of bone tissue occurs.
If the process turns into purulent inflammation of the soft tissues of the face, the patient suffers not only from local inflammation of the bone, but also from general intoxication.
Inflammatory processes in the mouth do not always develop into osteomyelitis. This disease most often affects people with weakened immune systems.
General information
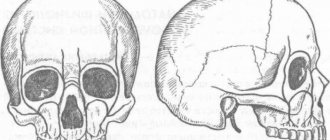
Osteomyelitis of the mandible is more common, more severe and has more complications. With chronic osteomyelitis of the lower jaw, the bone is affected deeper, which can lead to jaw fractures. Inflammation affects a dangerous area - the jaw processes. Acute osteomyelitis of the lower jaw easily turns into subacute and then chronic.
Osteomyelitis of the upper jaw develops more rapidly and can lead to inflammation of the maxillary sinuses. However, since the bone tissue here is less dense, abscesses and phlegmons develop less often with osteomyelitis of the upper jaw, and the disease itself is easier.
The entry point for infection is a diseased tooth, and the causative agents of inflammation are Staphylococcus aureus and Staphylococcus alba, pneumococci, Escherichia coli and typhoid bacilli. This microflora is usually located in areas of chronic infection of the tissues surrounding the tooth.
Inflammation in osteomyelitis does not occur suddenly; initially, a chronic infection develops in the gum for a long time - for example, in periodontitis or periodontitis. Then, if the outflow of waste products from the infection is disrupted, the microflora from the lesion spreads to the surrounding tissue.
Osteomyelitis of other parts of the skeletal system is caused by only one type of pathogen - staphylococcus (streptococcus), which penetrates the tissue through the bloodstream. Since osteomyelitis of the jaw can be caused by different pathogens, the course of the disease has much more distinctive features than with ordinary osteomyelitis.
Complications
An incorrect diagnosis or untimely initiation of therapy for osteomyelitis leads to the development of severe complications, which have a high mortality rate and often cause disability.
The most common complications of osteomyelitis of the jaw are:
- Abscesses of soft tissues, perimaxillary phlegmons and purulent leaks, which tend to quickly spread to the cervical region and the mediastinum. This pathology is extremely dangerous, since the sepsis associated with it (in non-medical vocabulary the term “blood poisoning” is used) quickly leads to damage to vital organs with the development of septic shock and death.
- Thrombophlebitis of the facial veins, mediastinitis, pericarditis or severe pneumonia.
- Purulent damage to the membranes of the brain with the development of meningitis.
- If the purulent focus is localized in the upper jaw, the infection may spread to the orbital region with damage to the eyeball, atrophy of the optic nerve, which leads to irreversible loss of vision.
Classification
Osteomyelitis of the jaws (photo) is classified according to several parameters.
Osteomyelitis may be caused by:
- Infectious
a) Single-gene. It is a consequence of dental disease - caries, stomatitis. The most common type of pathology accounts for 75% of all cases of osteomyelitis.
c) Non-odontogenic (hematogenous). The pathogen enters the bloodstream from other foci of infection. May be a consequence of chronic tonsillitis, diphtheria, scarlet fever.
- Non-infectious (traumatic). The result of mechanical damage to the jaw or a wound through which infection enters. Osteomyelitis can occur under the influence of a growing malignant tumor or become a complication after dental surgery. For example, if the nerve tissue is not carefully removed from the tooth socket.
According to the course of the disease, osteomyelitis of the jaw occurs:
- Spicy. It lasts 7–14 days, then passes into the subacute stage - when a fistula forms at the site of inflammation and exudate flows out from the site of inflammation.
- Chronic. Lasts from a week to several months. It ends with the rejection of dead bone areas through the fistulous tract. Treatment at this stage is mandatory.
- Subacute. The transitional form between acute and chronic disease lasts 4–8 days. The painful signs subside, but the infection is actively spreading.
According to the location of the pathology:
- Osteomyelitis of the upper jaw.
- Osteomyelitis of the lower jaw.
By coverage:
- Limited. The inflammation covers the alveolar process or the area of 2–4 teeth of the jaw.
- Diffuse. The pathology covers most or all of the jaw.
According to clinical and radiological forms, chronic odontogenic osteomyelitis is:
- productive. During the healing process, it does not form sequesters (dead bone areas);
- destructive. Upon recovery, it forms sequesters.
- destructive-productive.
Prevention
Preventive measures are not only the key to preventing the development of osteomyelitis, but also a factor that reduces the risk of complications and shortens the recovery period if the disease cannot be avoided:
- Timely treatment of caries, even if it has no clinical manifestations.
- Maintaining normal immune status through regular physical activity, rational and nutritious nutrition.
- Sanitation of all chronic foci of infection in the body.
- In case of injury, in the postoperative period or after tooth extraction, compliance with all preventive medical prescriptions.
In conclusion, it should be noted that, despite all the achievements of modern medicine, osteomyelitis of the jaw in adults and children does not lose its relevance. Timely detection of its signs and adequate treatment increase the patient’s chances of a full recovery and maintaining a high quality of life.
»
Causes of osteomyelitis of the jaw
Odontogenic osteomyelitis is caused by advanced diseases of the oral cavity. The infection penetrates into the bone tissue through the affected pulp or tooth root. Among the most common gates of infection are:
- caries;
- pulpitis;
- periodontitis;
- pericoronitis;
- alveolitis;
- granuloma or dental cyst.
With hematogenous osteomyelitis, infection through the bloodstream can come from abscesses on the neck or face (boils, carbuncles) or result from:
- purulent otitis;
- tonsillitis;
- umbilical cord infections in infants;
- inflammatory foci in diphtheria and scarlet fever.
With traumatic osteomyelitis, the infection from the external environment enters the open wound, then into the bone tissue. This may happen:
- with a gunshot wound;
- jaw fracture;
- damage to the nasal mucosa.
If a person has good immunity, his body successfully resists the invasion of pathogenic bacteria and in 60% of cases can prevent the development of the disease. If the patient suffers from chronic ailments - diseases of the blood, liver, kidneys, endocrine system, arthritis and polyarthritis, he will most likely develop osteomyelitis of the jaw.
Osteomyelitis in dentistry
Osteomyelitis of the jaw bones accounts for approximately a third of all identified cases of this disease. This statistical feature is not accidental and is determined by the presence of teeth, which are often a source of infection of bone tissue. In addition, there are a number of features in the jaw that predispose to the development of such a disease:
- a very abundant network of arterial and venous vessels in the maxillofacial region;
- active growth of the jaw and rapid changes in its structure during the period of replacement of milk teeth with permanent ones;
- the presence of relatively wide Haversian canals;
- very thin and delicate bone trabeculae;
- high sensitivity of myeloid bone marrow to infection.
All this leads to the fact that the penetration of almost any microorganism deep into the bone tissue provokes the development of osteomyelitis.
Symptoms of osteomyelitis of the jaw
At the initial stage, osteomyelitis of the jaw has no characteristic signs. The person feels unwell, as with most inflammatory diseases. Unaware of the real cause of poor health, the patient may assume another disease and self-medicate. Not only will this not help, but it will also delay the moment of recovery. Therefore, if you feel unwell, it is important to consult a doctor.
External symptoms of maxillary osteomyelitis:
- General weakness, sweating, headache. The person is depressed, he sleeps poorly, refuses to eat.
- Depending on the type of infection and the patient’s immunity, the body temperature rises to 38 or higher or remains normal. If there is no temperature, then the body is not fighting the infection.
- In the acute form of odontogenic osteomyelitis, the tooth affected by the infection hurts. The pain intensifies with pressure and is not relieved by taking painkillers. The tissue around the tooth is swollen and has a reddish tint. Not only the diseased tooth moves, but also those nearby.
- Sometimes an abscess develops on the periosteum of the tooth root. Inflammation affects neighboring teeth, and acute pain shoots into the ear, temple and eye area.
- With osteomyelitis of the lower jaw, the lower lip, mouth and chin become numb. When inflammation invades the jaw tissue, pain spreads throughout the face and neck. The submandibular and cervical lymph nodes become enlarged and painful.
- A periodontal pocket filled with pus forms in the space between the tooth and gum.
Symptoms of acute osteomyelitis of the jaw:
- it hurts to chew;
- at the site where the infection develops, the skin turns pale and becomes covered with plaque;
- the sclera of the eyes turn yellow;
- blood pressure surges;
- with osteomyelitis of the lower jaw, part of the lower lip becomes numb and stops moving, this is due to the fact that the source of inflammation compresses the alveolar nerve.
In subacute osteomyelitis, the inflammatory process continues and sequestration is formed. The teeth in the affected jaw retain and even increase mobility.
With chronic osteomyelitis, the patient feels satisfactory. During remission, the pain subsides. However, the following warning signs remain:
- lack of appetite;
- poor sleep;
- soreness of the facial skin;
- lymph nodes are enlarged;
- fistulas in the mouth do not heal, pus is regularly discharged from them;
- the mucous membranes of the mouth are swollen;
- The teeth on the affected jaw are mobile, and their mobility increases over time.
During an exacerbation, the patient again feels pain spread throughout the jaw and cannot always accurately indicate the location of its localization.
Infants and young children can also develop osteomyelitis of the jaw (usually the upper jaw). The disease develops against the background of sepsis or becomes a complication of ARVI. The symptoms of osteomyelitis in children are pronounced; the disease progresses rapidly and can lead to severe complications, including pneumonia and meningitis. Therefore, it is important to consult a doctor as soon as possible and begin treatment if your baby has the following symptoms:
- high temperature that cannot be reduced with antipyretic drugs;
- cheeks, eyes, lips swell, facial asymmetry appears, it is difficult for the child to open his eyes, and the swelling of the nose makes it difficult to breathe. If you do not see a doctor, the swelling spreads to the neck;
- lymph nodes enlarge;
- purulent foci are noticeable on the gums, and over time infiltrates and fistulas open;
- pain in the eye area.
Diagnostics
Osteomyelitis cannot go away on its own; without medical help, the patient’s condition will worsen.
Periodontitis, cysts and tumors of the jaw, as well as lesions of oral tissue due to syphilis, tuberculosis, and fungal skin infections have similar symptoms. Therefore, self-diagnosis is highly not recommended.
When visiting the clinic you must:
- Undergo an initial examination of the jaw by a dentist. With osteomyelitis, tapping and palpating the affected areas will be painful.
- Take an x-ray. In the acute form, it is not very informative, but in subacute and chronic pathology, areas of change in bone density and areas of dead bone tissue will be noticeable.
- Take a general urine and blood test, a biochemical blood test, and bacteriological culture to identify the type of pathogenic microorganisms.
- Get a CT scan.
Differential diagnosis
Differential diagnosis of osteomyelitis with other diseases that have similar symptoms is important, since an incorrect diagnosis can lead to an incorrect choice of treatment tactics and ineffective therapy. All this increases the risk of an unfavorable outcome of the disease and a poor prognosis for future health.
The differential diagnosis of osteomyelitis should include such diseases as:
- acute form of periodontitis,
- acute pulpitis,
- periostitis,
- suppuration of a tooth cyst,
- acute sinusitis of odontogenic origin,
- abscess of soft tissues in the maxillofacial area (MFA).
Treatment of osteomyelitis of the jaw
Treatment of osteomyelitis of the jaw is complex and consists of surgery, drug treatment and restorative therapy, which promotes tissue regeneration.
During surgery:
- the surgeon removes the affected tooth;
- treats fistulas and boils in the oral cavity;
- drains pus;
- removes dead (sequestered) areas of bone;
- fills hollow areas with bone materials;
- strengthens mobile teeth with splints.
At the same time, drug treatment is carried out:
- antibiotics;
- immunostimulants;
- vitamin complexes.
To consolidate the result, you must undergo a course of physical procedures:
- UHF;
- magnetic therapy;
- ultrasound therapy.
During the treatment process, the patient is prescribed plenty of fluids and a gentle diet of light, crushed and nutritious foods. It is necessary to carefully monitor oral hygiene.
Treatment
Treatment of osteomyelitis of the jaw bones consists of simultaneously solving two important problems:
- The fastest elimination of the focus of purulent inflammation in the bones and surrounding soft tissues.
- Correction of functional disorders that were provoked by the presence of a severe infectious process.
All patients, without exception, are subject to hospitalization in a surgical department specializing in maxillofacial surgery. If there is no such hospital, then treatment is carried out in a department with experience in dental surgery.
The complex of treatment measures includes:
- Surgical intervention with opening of the purulent focus, cleaning it of necrotic masses and complete drainage.
- The use of antibacterial drugs with a wide spectrum of activity.
- Detoxification and anti-inflammatory treatment, strengthening the immune system.
General care is also important, with strict bed rest, nutritious but gentle nutrition (hypoallergenic diet including all necessary nutrients, vitamins and minerals).
Forecast and prevention of osteomyelitis of the jaw
If the patient sought medical help on time, followed the doctor’s recommendations and received the correct treatment in full, osteomyelitis will be successfully cured. Incorrect treatment in combination with a weakened immune system can lead to the following complications:
- sepsis;
- acute purulent inflammation;
- general intoxication;
- the formation of multiple abscesses;
- meningitis;
- inflammation of the facial nerves;
- bone deformities;
- purulent sinusitis and destruction of the walls of the maxillary sinuses;
- infection of the orbit and formation of phlegmon;
- jaw fractures.
To prevent osteomyelitis of the jaw, it is important to:
- Have dental checkups every year.
- Properly brush your teeth, maintain oral hygiene, and use interdental floss and rinses.
- Treat teeth and gums in a timely manner.
- Protect your jaw from injury.
- Strengthen immunity.
- Do not start treatment for infectious diseases, including tonsillitis and ARVI.