From this article you will learn:
- what is tooth root cement,
- its structure and functions,
- histological preparations.
Dental cement (cementum) is a highly mineralized tissue, reminiscent in its structure of coarse-fiber bone, which covers the root of the tooth (up to its neck) with a thin layer. But unlike bone tissue, root cement is not subject to constant restructuring, it does not have vessels, and its trophism is carried out through the usual diffusion of nutrients dissolved in the main amorphous substance in the periodontal structure.
The main function of cement is to form the ligamentous apparatus of the tooth (periodontal attachment), which holds the tooth in the alveolus, and also contributes to the redistribution of chewing pressure from the tooth to the alveolar bone. Let us recall that periodontal fibers begin to grow simultaneously - both from the side of the root cement and from the side of the compact lamina of the alveoli. Next, with the help of immature collagen (procollagen) in the center of the periodontal fissure, the ends of these fibers are tied together, bundles of fibers are formed.
Tooth root cement: diagram and photo
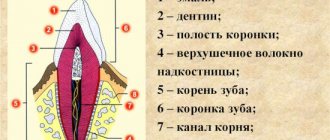
The cementum layer is present only on human teeth, as well as on the teeth of other mammals. In the area of the tooth neck, the thickness of the cement is less - from 20 to 50 microns, while in the area of the root apex - from 100 to 150 microns. I think you are familiar with the fact that “secondary dentin” is produced by odontoblasts throughout life, and in the same way, constant formation of cement on the root surface occurs throughout life. And therefore, if you live to retirement age, the cement of your teeth will most likely have time to at least triple its thickness (Fig. 3).
Structure of tooth dentin –
Dentin consists of calcified intercellular substance, which is penetrated by the so-called “dentinal tubules” (dentinal tubules), which ensure trophism and mineralization of dentin. Dentinal tubules run radially, in the coronal part of the tooth - in the direction from the wall of the pulp chamber to the enamel-dentin border, and in the root part of the tooth - from the wall of the root canal to the surface of the tooth root. However, if in the root part of the tooth, as well as in the area of the occlusal surface of the tooth crown, the dentinal tubules have an almost straight shape, then in the lateral parts of the crown they will already be S-shaped.
Dentinal tubules (electron microscopy) –
The diameter of the tubules ranges from 0.5 to 4 microns, and they will be wider in the internal parts of the dentin and gradually narrow outward (like a flattened cone). Inside the tubules there are processes of odontoblasts, unmyelinated nerve fibers, and tissue fluid also circulates. The odontoblasts themselves are located outside the dentin - their bodies are located in the superficial layer of the pulp, and their processes, passing along the entire length of the dentinal tubules, end in the area of the enamel-dentin border (Fig. 8).
The lateral canals extend from the dentinal tubules in a perpendicular direction. There are especially many of them in the predentin and inner layers of peripulpal dentin (100–200 µm from the border with the pulp). There are quite a few of them in the middle sections of dentin and again become numerous at the periphery - in the area of mantle dentin. In the lateral canals there are lateral branches of the processes of odontoblasts, which anastomose with each other. Let us recall that it is odontoblasts that participate in the formation of the organic dentin matrix and its further mineralization.
Odontoblasts, predentin and dentinal tubules (histology) –
Please note that on the histological specimen (Fig. 6) predentin looks like a light stripe, turning into a zone with spherical formations of a darker color (globules). The predentin layer has minimal mineralization and consists mainly of an organic matrix - intertwined collagen fibrils (Fig. 7). Spherical formations at the border of predentin and peripulpar dentin are nothing more than “calcospherites”, which are foci of mineralization. Low-mineralized dentin located around such globules is called “interglobular.”
Subsequently, the globules merge, forming homogeneous, highly mineralized dentin. It is also worth noting that when the dentinal tubules approach the enamel-dentin border or the cementum layer, their ends form large terminal branches (similar to tree branches). A number of terminal segments of dentinal tubules penetrate even through the enamel-dentin boundary, forming the so-called “enamel spindles”. According to most authors, these formations are involved in the mineralization of deep layers of enamel.
Architectonics of dentinal tubules –
The density of the tubules differs in different layers of dentin. Some of them are most densely located in the peripulpal dentin, where there are from 50,000 to 75,000 of them per 1 mm2 of dentin. For 1 mm2 of the mantle layer of dentin there will be only from 15,000 to 30,000. But let us draw your attention to the fact that in this case it decreases not the number of tubules as such, but precisely the density of their location in the surface layers of dentin (due to their radial direction and with a simultaneous increase in the area of the outer layers).
Functions of tooth root cement –
1) Protective function – the content of inorganic components in cement reaches 70%, which makes it resistant to mechanical loads. Consequently, one of its functions will be to protect root dentin from damaging effects.
2) Participation in the formation of periodontium - the formation of periodontal fibers occurs simultaneously both from the cementum of the tooth root and from the bone plate of the alveoli. According to a number of authors, these collagen fibers are subsequently intertwined with each other through immature collagen (procollagen), turning them into a single whole. The depth of immersion of periodontal fibers into the cement of the tooth root is from 3 to 5 μ.t.
3) Fixing (retaining) - cement of the tooth root together with the compact plate of the alveolus and periodontal fibers - ensures fixation of the tooth in the alveolus.
4) Compensatory function - when the length of the tooth decreases as a result of physiological abrasion of the enamel, increased production of cement occurs in the area of the apex of the tooth root. As a result, the tooth is pushed out of the alveoli into the oral cavity, and thus the size of the clinical crown of the tooth increases. This becomes especially noticeable in elderly patients.
5) Participation in reparative processes - for example, when the cause of root resorption is eliminated, its partial restoration may occur. Or, if there is a crack in the tooth root, cement may form between the fragments, which can lead to the elimination of the defect.
Structure of dentinal tubules –
Dentinal tubules pass in the so-called dentinal tubules. The wall of each dentinal tubule is formed by the so-called “peritubular dentin,” which is characterized by a very high degree of mineralization and the absence of collagen fibers. Between the dentinal tubules there is the so-called “intertubular dentin”, which is characterized by a lower degree of mineralization and a large number of collagen fibers (fibrils). Dentinal tubules are hollow inside, which is why they are often called dentinal tubules.
Each tube is internally coated with a thin layer of organic matter - this layer contains a high concentration of glycosaminoglycans and is commonly called the Neumann membrane. In the center of the dentinal tubules there are processes of odontoblasts (Toms fibers). The space between the odontoblast process and the wall of the dentinal tubule is filled with dentinal fluid, which is similar in composition to blood plasma. In addition to the processes of odontoblasts and tissue fluid, they also contain non-myelinated nerve fibers (however, they can only be found in peripulpar dentin).
Scheme of the structure of dentin –
Peritubular and intertubular dentin –
During the process of dentinogenesis, intertubular dentin, located between the dentinal tubules, is formed earlier than peritubular dentin (24stoma.ru). The deposition of peritubular dentin occurs from within the already formed dentinal tubules (the processes of odontoblasts take an active part in this). The thickness of peritubular dentin from the pulp end of the tube is from 40 to 50 nm, and from the enamel-dentin border from 500 to 700 nm.
As we said above, peritubular dentin has a significantly higher mineralization. For example, the content of hydroxyapatite in it will be 40% higher than in intertubular one, but there are practically no organic components in it. This leads to the fact that when moderate caries occurs, peritubular dentin will be destroyed much faster than intertubular dentin. And as a consequence, the ongoing processes of demineralization will lead to the expansion of dentinal tubules and an increase in dentin permeability, including for pathogenic bacteria.
In turn, intertubular dentin contains many organic components, for example, calcified collagen fibrils with a diameter of about 75 nm (hydroxyapatite crystals are located along the axis of the fibrils). Collagen fibrils form a so-called “framework”, which serves as a basis for the deposition of mineral salts. Below you can see what the collagen framework of dentin looks like in electron microscopy images taken after its forced demineralization.
Cementocytes and cementoblasts: functions and composition
These two types of cells make up the cellular cement. They have different compositions and perform different functions.
Cementocytes are located in lacunae and resemble osteocytes in structure. The short processes in their composition are directed towards the periodontium. In turn, functionally active cementoblast cells are located on the surface of the cement and are responsible for the regular appearance of new layers on it. They are the ones who take part in the restoration of damaged parts of the tooth, for example, in the event of a traumatic root fracture, they form a “coupling”.
Organic dentin matrix –
The organic matrix of dentin is located between the dentin tubules (in intertubular dentin). It consists of collagen fibrils and an amorphous substance located between them. It is interesting that the direction of collagen fibrils and their structure will differ in the mantle and peripulpar layers of dentin. This is due to the fact that during primary dentinogenesis, the organic matrix of mantle dentin is first produced, and only then the matrix of peripulpar dentin.
In mantle dentin, fibers running in a radial direction, parallel to the course of the tubules (“Korff fibers”) will predominate. But the peculiarity of Korff fibers is not only their directionality, but also the fact that they will consist of fairly thick fibrils united into conical-tapering bundles. Moreover, it is worth clarifying that the radial-parallel direction of Korff fibers is more typical for that part of the mantle dentin that is closest to the occlusal surface of the tooth crown. And on the lateral surfaces of the crown and in the root area, the Korff fibers acquire an increasingly oblique direction.
As we said above, the matrix of peripulpal dentin is formed later than that of mantle dentin. Odontoblasts during this period synthesize much thinner fibrils, which intertwine with each other (see figure below). These fibers will be located tangentially, i.e. they extend from the dentinal tubules at almost a right angle (they are called “Ebner’s fibers”). But collagen fibers are not the only component of the organic dentin matrix, and we must not forget about the amorphous substance surrounding them.
Collagen fibrils in peripulpar dentin –
Amorphous substance –
Collagen fibers are surrounded on all sides by a basic amorphous substance, which consists mainly of glycosaminoglycans (chondroitin sulfates). In addition to them, the organic matrix includes a large amount of non-collagen proteins (their share is about 20% of the organic dentin matrix). The amorphous substance also contains proteoglycans, which are formed as a result of the combination of chondroitin sulfates and non-collagenous proteins.
Non-collagenous proteins play an important role in the processes of dentin mineralization. Below we have listed their main varieties -
- calcium binding proteins
- bone morphogenetic proteins (BMPs),
- glycoproteins (fibronectin, osteonectin),
- calcium ATPase and alkaline phosphatase,
- collagenases and collagen-digesting enzymes necessary for the restructuring of the organic matrix.
In the organic basis of dentin, lipids (glycolipids and phospholipids) have also been identified, probably participating in the mineralization of the matrix.
Nerve fibers -
Unmyelinated nerve fibers penetrate into dentin from the peripheral parts of the pulp, and they can only be detected in predentin (they penetrate into it to a depth of several micrometers, and only rare fibers - to a depth of 100 to 200 microns). In addition, nerve fibers are not found in all, but only in some dentinal tubules. In the more peripheral layers of dentin, there are no nerve endings at all, and in this case the main role in the formation of pain impulses is played by dentinal fluid (changes in hydrodynamic conditions).
Composition of mature dentin
- Inorganic substances – phosphate salts of magnesium and calcium (70%);
- organic substances – type 1 collagen (20%);
- water (10%).
Dentin looks like bundles of collagen fibers containing mineralized intercellular substance. The bundles are penetrated by dentinal tubules with processes of odontoblasts, or Toms' processes. The fibers are arranged differently in different areas. In the outer, or mantle, dentin, formations of the radial direction predominate, in the inner - tangential.
Features of the inorganic matrix –
Dentin consists primarily of calcium phosphate (in the form of hydroxyapatite crystals), as well as small amounts of calcium fluoride and carbonate.
Hydroxyapatite crystals in dentin are much smaller and thinner when compared with tooth enamel, and have the following dimensions - length 20 nm, width 18-20 nm, thickness 3.5 nm. Those. The crystals are quite small and needle-shaped. Electron microscopy made it possible to establish that these crystals are located not only outside the collagen fibers, but also inside them (located even between the collagen fibrils). Dentin is characterized by a special form of deposition of crystals of mineral salts. If, for example, in the main substance of bone tissue the deposition of mineral salts occurs evenly (in the form of tiny crystals), then in dentin the mineralization process occurs in several stages. At the first stage, the formation of spherical crystalline structures occurs (in the form of “globules” - calcospherites), between which areas with non-calcified or slightly calcified basic substance - interglobular dentin - are still preserved.
Globular and interglobular dentin (histology) –
Globular and interglobular dentin are best visible at the border of peripulpar dentin and predentin (in the coronal part of the tooth), because It is in this zone that mineralization of secondary-formed dentin actively occurs. In addition, it is in this zone that the largest calcospherites can be found. Gradually, the globules increase in size and merge, forming homogeneous, highly mineralized dentin.
What are Owen's lines and Abner's lines?
Primary (physiological) dentin is formed during the period of tooth formation and eruption. It is produced by odontoblasts at a rate of approximately 4-8 µm/day, and the activity of odontoblasts has periods of activity and rest. This periodic change in odontoblast activity leads to the presence of so-called growth and contour lines in dentin.
Owen's contour lines reflect the daily rhythm of dentin deposition by odontoblasts. They are located at right angles to the dentinal tubules and correspond to “rest periods” in the activity of odontoblasts. During these periods, much less intense mineralization of dentin will occur - with the formation of very small interglobular spaces. The number of Owen lines can increase in pathological conditions of the body that affect the processes of mineralization of hard dental tissues.
Ebner's growth lines correspond to a slower 5-day cycle of formation of the organic dentin matrix by odontoblasts, i.e. periods of less mineralization of the dentin base substance.
Dead pathways in dentin –
Also, so-called dead paths (on thin sections of teeth) can be found in dentin, which arise when some of the odontoblasts die. Some authors say that only the exposure of 1 mm of the child’s area leads to the death of up to 30,000 odontoblasts. At the same time, the processes containing in the dentinal tubules undergo decay; accordingly, the cavities of the dentinal tubules will be filled with decay products and gaseous substances.
Due to the presence of gases, such dentinal tubules (dead paths) appear black on polished sections of teeth. By the way, the term “dead paths” was coined by E. Fish. It is also worth noting that the sensitivity of dentin in such areas is reduced, and from the side of the dental pulp in these areas there will be increased production of tertiary dentin.
What are dentinal tubules
They look like thin tubes that taper in the outer direction and penetrate the tissue from the pulp to the periphery. In the depths they branch, and inside they are filled with Toms fibers, which nourish dentin and saturate it with mineral salts. It is the dentinal tubules that ensure the high permeability of dentin, despite its dense structure. This allows the pulp to quickly respond to damage.
The dentinal tubules also contain dentinal fluid. Its movements cause pain and sensitivity in the teeth. It is believed that due to temperature, mechanical or other effects, the liquid begins to move, irritating the nerve endings in the pulp.
Secondary and tertiary dentin –
Secondary dentin is deposited (from the pulp chamber side) throughout the life of the individual, which leads to a gradual reduction in the volume of the pulp chamber. Secondary dentin, like primary dentin, is produced by odontoblasts. Secondary dentin differs from primary dentin (formed during the formation and eruption of teeth) by a less regular structure, which is expressed in a change in the direction and number of dentinal tubules and collagen fibers, as well as a lower degree of mineralization. The size of the dentinal tubules itself also decreases.
Deposits of secondary dentin occur more actively in the area of the roof of the pulp chamber, as well as in its side walls. In addition, secondary dentin is actively deposited in the area of the bottom of the pulp chamber (in multi-rooted teeth). In connection with all this, the shape of the pulp chamber gradually changes - the pulp horns become flattened, its volume decreases. An interesting fact is that in men the intensity of secondary dentin deposition is higher. In addition, it is noted that with age, the intensity of secondary dentin deposition decreases.
Another type of dentin is the so-called “tertiary dentin” (dentinum tertiarium), which is also called reparative or irregular. Unlike secondary dentin, which is produced fairly evenly from the inner surface of the pulp chamber, the formation of tertiary dentin occurs locally. Local dentin formation is caused by the influence of strong irritating factors on the tooth, for example, this occurs when the enamel is destroyed or increased abrasion, or dentin is exposed.
With slowly developing caries, the production of tertiary dentin allows, for some time, to prevent the penetration of pathogenic bacteria and their toxins into the pulp. Thus, tertiary dentin performs a protective function. It is also worth noting that tertiary dentin is also characterized by the incorrect direction of the dentinal tubules, or they may be completely absent.
Tooth dentin: histology
Below you can see the histology of tooth tissue in stunning resolution, as well as an excellent lecture on dentin morphology in English (if you wish, you can turn on subtitles and select translation from English into Russian in the settings).
How are cementum, tooth sensitivity and periodontitis related?
Loss of cementum contributes to a number of dental problems, such as tooth sensitivity, loss of enamel, and gum recession . When cementum is lost, the dentin underneath is exposed, and this, in turn, can cause tooth sensitivity. The latter manifests itself as short-term or acute pain in the area of one or more teeth. If you've ever winced and winced painfully after taking a sip of cold water or juice, you know the feeling!
While cementum loss can trigger the development of some dental diseases, other dental diseases can trigger cementum loss. Such diseases include, for example, periodontitis. Cementum loss occurs when there is irreversible damage to the bone and connective tissue fibers that hold the tooth in place. Such damage to bone tissue and cement is characteristic of progressive periodontitis and leads to tooth mobility, which in some cases even has to be removed.
Age-related changes in dentin –
We have already said above that with age, the deposition of secondary and tertiary dentin occurs, which also leads to a decrease in the size of the pulp. But in the teeth of older people you can often notice areas of dentin in which mineral salts are deposited not only in the main substance, but also inside the dentinal tubules themselves (this occurs against the background of degeneration processes of odontoblast processes). As a result, complete obliteration of the tubule lumen occurs, i.e. their physiological sclerosis.
Obliteration of the lumen of the tubules leads to a decrease in tooth sensitivity. In addition, the refractive indices of light in the tubules and in the main substance are aligned in this case, and therefore such areas of dentin appear transparent. Accordingly, such dentin is often called “transparent” or “sclerotic.” The formation of transparent dentin most often occurs first in the apical part of the root, and then slowly spreads towards the coronal part of the tooth. We hope that our article was useful to you!
Sources:
1. Higher professional education of the author in dentistry, 2. The European Academy of Paediatric Dentistry (EU), 3. “Anatomy of human teeth” (Gayvoronsky, Petrova). 4. “Therapeutic dentistry” (Politun, Smolyar), 5. “Histology of the oral cavity” (Glinkina V.V.).
Text of the book “Fundamentals of clinical dental morphology: a textbook”
5.2.1. The structure of the dental pulp
In general, the pulp is a richly vascularized and innervated specialized loose unformed connective tissue containing cells, fibers and an amorphous ground substance. In some parts of the tooth, these components are organized into clear demarcation zones.
The total pulp volume of all permanent teeth is 0.38-0.40 cm3, i.e., on average, about 0.02-0.03 cm3 in each tooth. The pulp of molars is 3–4 times larger in volume than the pulp of incisors. The volume of dental pulp is presented in table. 2.
table 2
Pulp volume of permanent teeth of the upper and lower jaws
The pulp of the tooth crown contains more cells and intercellular substance per unit volume than collagen fibers.
It contains a wide variety of well-differentiated cells. Odontoblasts in this part of the pulp are prismatic in shape and arranged in several rows.
The pulp that fills the canals of the tooth root is built like a fairly dense connective tissue with a predominance of bundles of collagen fibers over cellular elements.
The root pulp is less vascularized and innervated than the coronal pulp, its cellular composition is less diverse, and cubic or flattened odontoblasts are usually located in 1–2 rows. These differences in structure apparently depend on the nutritional characteristics of the hard tissues of the tooth in the area of the crown and root. In the crown area, dentin and enamel receive nutrients and calcium salts almost exclusively from the dental pulp; At the root, nutrition of the hard tissues of the tooth is carried out not only through the pulp, but also through the diffusion of nutrients from the pericementum. The consequence of this is a decrease in the trophic role of the root pulp and a change in its structure. In addition, a significant place in the root pulp is occupied by large blood vessels passing into the tooth cavity, the pulsation of which may affect the structure of the connective tissue surrounding these vessels.
In the crown pulp, 4 zones are distinguished according to the composition and properties of the tissue [48]:
1 – odontoblastic zone;
2 – Weyl’s light zone;
3 – subodontoblastic zone;
4 – central zone of the dental pulp.
In the first, outermost zone, elongated cells with basophilic cytoplasm - odontoblasts - are compactly arranged in one or several rows. The processes of these cells (Toms fibers) penetrate the dentinal tubules and penetrate the entire thickness of the dentin. Odontoblasts are closely connected by intercellular junctions, between which nerve fibers pass, traveling together with the processes of odontoblasts into the dentinal tubules.
Odontoblasts and their processes play an important role in the nutrition of the tooth and the delivery of mineral salts to the enamel and dentin. They remain in the pulp of an adult tooth throughout his entire life, while also performing their dentin-forming function, although not as intensely as during the period of tooth development.
With age, as the dentin layer thickens and the size of the pulp cavity decreases, the location of odontoblasts and their shape change. In a developing tooth they are usually located in one layer, and in an adult tooth - in several layers. Initially, the prismatic shape of the cells gradually turns into a pear-shaped or cone-shaped, vacuolization of odontoblasts is noted, which causes deformation and death of some odontoblasts.
In the root pulp of a formed tooth, the layer of odontoblasts is thinner than in the crown pulp. The cells are smaller and closely adjacent to each other.
Behind the layer of odontoblasts there is a cell-poor light layer of Weil, consisting mainly of collagen fibers and processes of cells of the subodontoblastic zone. It is well expressed in the crown pulp and absent in the root pulp. The Weyl layer usually forms quite late, often after tooth eruption. Modern research has shown that this area contains extensive networks of nerve fibers and blood capillaries. From the nerve plexus (Rashkov's plexus) branches originate, forming tree-like branches on odontoblasts, and also passing between them into the dentinal tubules, where they contact Thoms fibers. In teeth with a high rate of dentin formation (during their growth or during active production of tertiary dentin), this zone narrows or disappears completely due to the migration of cells from the subodontoblastic zone into it.
The third layer of pulp consists of a large number of stellate cells (preodontoblasts), which are classified as poorly differentiated cells. Numerous thin and long processes extend from the bodies of these cells, which branch repeatedly and anastomose with each other. According to a number of authors [33, 38, 40, 60], these cells are capable of differentiation and transformation into odontoblasts, as well as fibroblasts. Therefore, in the dental pulp of an adult, when some of the odontoblasts die, their replacement is possible due to the differentiation of stellate cells of the subodontoblastic layer. In addition, fibroblasts, lymphocytes, poorly differentiated cells, as well as capillaries, myelinated and unmyelinated nerve fibers are also located in this zone.
The central zone of the pulp is loose fibrous connective tissue rich in cells, vessels and nerves. In the pulp of permanent teeth with formed roots, four main cell groups are identified:
– odontoblasts;
– fibroblasts;
– poorly differentiated ectomesenchymal cells;
– macrophages.
In smaller numbers, dendritic cells, lymphocytes, plasma cells, mast cells, and blood granulocytes are constantly present in the central zone of the pulp. The first three groups originate from the cells of the head neural crest. They are constantly present in the pulp of the crown, in contrast to wandering macrophages, which originate from blood monocytes and, depending on the state of the pulp, pass from the blood to the tissue and back.
Odontoblasts are the largest cell population in the pulp (Fig. 110). These are specific pulp cells that form dentin and provide its trophism. Odontoblasts are located on the periphery of the pulp, located very densely in the crown pulp (40,000-50,000 per 1 mm2 of the surface of the dentinopulpal border) and, less often, in the root pulp. The shape of the cell body in the crown is prismatic or pear-shaped, which changes closer to the root to fusiform, and then to cubic or flattened in the root pulp. The shape of a cell changes not only depending on its location, but also in connection with its function: the higher the activity, the greater the height of the odontoblast.
Rice. 110. Structure and topographical features of odontoblasts (scheme according to R. Krstic).
1 – dentin; 2 – predentin; 3 – odontoblastic zone of the pulp; 4 – blood capillary; 5 – nerve fiber; 6 – odontoblast body; 7 – matrix vesicles; 8 – Toms fibers; 9 – Neumann vagina.
In prismatic cells, an oval nucleus with 1–2 nucleoli located in the basal part of the cell is clearly visible. In cubic odontoblasts, the spherical nucleus usually lies centrally. Euchromatin predominates in the nuclei of odontoblasts; small accumulations of heterochromatin are observed only near the nuclear membrane.
In the cytoplasm there are cisterns of the granular endoplasmic reticulum, a large number of lysosomes, mitochondria, glycogen granules, small lipid droplets, and in the apical region there are secretory granules containing precollagen and predentin proteoglycans.
The apical part of the odontoblast body tapers, continuing into the long branching process of Thoms, which is directed into the dentinal tubule. The process is characterized by well-developed cytoskeletal elements, oriented longitudinally, numerous smooth and bordered vesicles, rare mitochondria and short cisternae of the agranular endoplasmic reticulum.
Neighboring odontoblasts are firmly connected by intercellular junctions: desmosomes, gap junctions and tight junctions, thanks to which the odontoblast layer is able to perform a barrier function, regulating the movement of molecules and ions between the pulp and predentin. Odontoblasts are classified as terminally differentiated cells, so their lifespan can reach the lifespan of a tooth [5]. The most important functions of the pulp are nutrition and maintenance of the viability of odontoblasts.
Fibroblasts are found in large numbers in the central zone of the pulp, especially in the teeth of young people (Fig. 111). They originate from undifferentiated ectomesenchymal cells, which are also located in the pulp. Fibroblasts can exist in one of two functional states: active (fibroblasts) or passive (fibrocytes). The functional state of the cells depends on age, clinical characteristics of the pulp, etc.
Structurally, pulp fibroblasts are spindle-shaped process cells with a light nucleus containing fine chromatin and a large nucleolus, weakly basophilic cytoplasm, well-developed granular endoplasmic reticulum and the Golgi complex, as well as a large number of vesicles, microtubules, microfilaments and pinocytotic vesicles. The main product of the activity of pulp fibroblasts is collagen types I and III. They also synthesize and secrete components of the main amorphous substance of the pulp: glycosaminoglycans, proteoglycans, glycoproteins. During inflammatory processes (pulpitis), fibroblasts take part in the formation of a fibrous capsule that limits the source of inflammation. In addition to synthetic activity, they are able to absorb and digest components of the intercellular substance.
Rice. 111. Microphotograph of a section of a tooth. Hematoxylin and eosin staining.
1 – dentin; 2 – predentin; 3 – odontoblastic layer; 4 – fibroblasts; 5 – blood vessel; 6 – central zone of the dental pulp.
Alternatively, a fibrocyte is an inactive, resting cell with underdeveloped protein synthesis organelles. In principle, these are two states of the same cell, which manifest themselves depending on the state of the surrounding connective tissue. High synthetic activity is characteristic of fibroblasts in the teeth of young people. With age, the proportion of cells with low plastic characteristics increases. Recently, a 3rd condition has been described - the so-called fibroclast, or collagen-resorbing cell.
The presence of fibroclasts was shown for the first time in the periodontal ligament. Their presence in the crown pulp has not yet been noted, but some researchers consider this to be a matter of time.
The third major cell type in the central zone of the human pulp is undifferentiated ectomesenchymal cells. These are triangular-shaped cells with a large nucleus containing a significant amount of heterochromatin. The cytoplasm contains a large number of ribosomes and polyribosomes, lipid droplets and a well-developed granular endoplasmic reticulum. A variety of microfilaments and microtubules is also noted, which indicates sufficient mobility of these cells. Cells have a dense glycocalyx containing membrane receptors, antigenic zones, etc., which take part in the mechanisms of “recognition” of cells and their clusters. In many cases, these cells are interconnected through filopodia and microprocesses into a complex three-dimensional network.
The large population of undifferentiated ectomesenchymal cells in the pulp provides its high regenerative capacity.
When exposed to certain pathogens, these cells can undergo terminal differentiation into either fibroblasts or odontoblasts of the pulp. The latter replace old or dead cells, and also replenish the odontoblasts necessary for the formation of secondary and tertiary dentin. However, with age, there is a decrease in the number of undifferentiated pulp cells, which leads to a decrease in the ability of the pulp to regenerate with aging.
Unlike the three types of cells in the central zone of the pulp considered, which have a common origin from the cells of the head part of the neural crest, macrophages originate from circulating specific blood cells - monocytes. Their quantity in the pulp, morphology and metabolism depend on the functional state of the surrounding connective tissue. Macrophages are especially numerous in the dental pulp of young people. These are polymorphic cells with an eccentrically located nucleus.
The cytoplasm contains a well-developed granular endoplasmic reticulum and Golgi complex, as well as a large number of lysosomes and vacuoles. A pronounced cytoskeleton of microfilaments and microtubules ensures high mobility of these cells. The surface of the cell is covered with many folds and outgrowths, indicating its pronounced phagocytic activity.
The main function of macrophages is the capture and digestion of various microorganisms, bacteria, individual cells, etc. The process includes phagocytosis, pinocytosis and digestion using cellular hydrolytic enzymes located in lysosomes. This allows macrophages to actively participate in immune reactions, destroying various antigens, tumor cells, and parts of dead cells. It is logical to assume that dental pulp macrophages are capable of performing any of these functions.
The presence of macrophages in the dental pulp indicates that, in addition to performing its trophic and dentin-forming functions, it plays an important protective or barrier role.
Dendritic cells are also a permanent component of the pulp, making up 6–8% of the total cell population of the pulp. These are cells of variable shape with numerous branching processes, a clearly defined nucleus and a well-developed lysosomal apparatus. They are antigen-presenting cells, i.e. their function is to absorb various antigens, process them and present them to lymphocytes. In the pulp, the ratio of dendritic cells and macrophages is 4: 1. Dendritic cells are much superior to macrophages in their ability to induce the proliferation of T-lymphocytes. Therefore, the number of these cells increases sharply with antigenic stimulation.
The largest number of dendritic cells is concentrated in the horns of the crown pulp. They are located along the vessels, near the odontoblasts and in the subodontoblastic layer. Their content in the pulp is small after birth, but increases as the pulp matures.
Lymphocytes, predominantly small lymphocytes (about 90% of their total number), are present in the pulp in small quantities in its peripheral areas. These are most often different subpopulations of T cells. B lymphocytes are almost never found in normal pulp. Only a few plasma cells are observed, which are the final stages of B cell differentiation. These cells actively synthesize immunoglobulins, providing humoral immune responses.
It should be noted that the content of lymphocytes in the pulp increases sharply during inflammation. During the same period, mast cells containing biologically active substances (heparin, histamine, eosinophilic chemotactic factor, leukotrienes) are detected in the pulp, the release of which causes a number of effects, including dilation of blood vessels and an increase in the permeability of their walls. According to some authors, mast cells are constantly present in the dental pulp of children.
In addition to the described cells, other types of cells are also noted in the pulp. Most of these cells are found in connection with the vascular wall - endothelial cells, pericytes, smooth muscle cells, and rare eosinophilic granulocytes.
In addition to cells, the central pulp also contains collagen fibers. Collagen makes up 25–30% of the dry mass of dental pulp, and its content increases with age. Modern biochemical studies have shown that this is collagen types I and III.
The collagen fibers themselves (type I collagen) create a system of supporting elements for cells, blood vessels and nerves. In the central parts of the crown pulp they are located loosely, in the peripheral parts they form denser clusters. In the root canal, the fibers are oriented along its length, forming dense bundles. Some of the fibers penetrate between the odontoblasts, mixing with predentin fibers. Throughout the pulp, reticular fibers formed by type III collagen are also located in the form of a network. During the formation of dentin, these numerous fibers initially lie between the odontoblasts and are called Corff fibers.
Precollagen, oxytalan and elastic fibers were also identified in the pulp. The latter are, strictly speaking, components of the wall of blood vessels. Oxytalan fibers are numerous in the peripheral part of the pulp, do not have a strict orientation and are usually associated with blood vessels. They are classified as preelastic fibers.
As stated, the pulp, in addition to cells and fibers, contains a thin amorphous substance, which is a component of the extracellular matrix of the pulp. It consists of water, glycosaminoglycans (chondroitin sulfates and hyaluronic acid), glycoproteins, proteoglycans. Possessing high diffusion abilities, the amorphous intercellular substance promotes the distribution of nutrients between cells, vessels and nerves.
Blood supply to the pulp.
Vascularization and angioarchitecture of blood vessels in the pulp have their own characteristics. All blood and lymphatic vessels, as well as nerves, enter (and exit) the pulp mainly through the opening of the apex of the tooth root, forming a neurovascular bundle in the root canal. In some cases, additional vessels and other structures enter the pulp through accessory canals on the side walls of the tooth root. these channels are clinically important because they can facilitate the spread of infection from the periodontium to the pulp and vice versa.
After entering the root pulp, vessels - arterioles with a diameter of 50-150 microns have an almost straight (vertical) direction and penetrate into the coronal pulp, occupying its central zone. A feature of the blood vessels of the pulp is the relatively small thickness of their walls compared to the lumen. Smaller precapillary arterioles with a diameter of 10–12 μm depart from the central vessel, which then form an extensive capillary plexus in Weil’s layer, feeding the pulp and odontoblasts.
Pulp capillaries with a diameter of 8-10 microns are divided into two groups: fenestrated (about a third), located mainly near odontoblasts, and somatic (2/3 of all capillaries). The latter are characterized by the presence of many pinocytotic vesicles in the cytoplasm of the endothelial cells of the vascular wall. Both capillaries provide nutrition to all structural elements of the dental pulp.
The presence of fenestrated capillaries facilitates the rapid transport of metabolites to odontoblasts during dentin formation and its subsequent mineralization. Therefore, they are especially developed during the period of active dentinogenesis. After tooth eruption and dentin formation slow down, the number of these capillaries decreases, and they usually shift somewhat towards the central sections of the pulp.
The volume of the capillary bed in the pulp can vary significantly, which is facilitated by the presence of arteriovenular anastomoses. At rest, most of the anastomoses and capillaries do not function, but their activity increases sharply when the pulp is irritated and causes the development of a hyperemic reaction. The frequency of pain during pulpitis is also associated with the operation of this mechanism.
From the subodontoblastic capillary network, blood flows into muscle-type venules (containing smooth myocytes in the wall), emerging from the pulp through the opening of the tooth apex. As a rule, venules are located centrally in the pulp, while arterioles occupy a more peripheral position.
A unique feature of the pulp circulatory system is that the diameter of the efferent venules is smaller than the diameter of the arterioles entering the pulp. Therefore, even in a normal pulp there are always phenomena of hyperemia and blood stasis, which allowed A. Fisher (1995) to call the pulp a stagnant organ. The pressure in the pulp chamber is 20–30 mmHg. Art., which is significantly higher than interstitial pressure in other organs. The indicated structural features of the vascular system probably ensure slow blood flow through the pulp, which has a certain physiological significance for the nutrition of tooth tissue.
The question of the lymphatic vessels of the pulp remains largely open. Some researchers believe that the pulp contains lymphatic capillaries and vessels, others advocate the presence of endothelial-lined tissue spaces and crevices that communicate with venous vessels. The outflow of lymph from the pulp occurs in the submandibular and submental lymph nodes.
Innervation of the pulp.
Sufficiently large myelinated and unmyelinated nerve fibers of the trigeminal nerve enter the pulp through the opening of the tooth apex along with blood vessels, forming a neurovascular bundle in the root canal that provides nutrition and innervation to the tooth.
Unmyelinated fibers make up up to 60–80% of the total number of fibers. In the root pulp, only about 10% of the fibers form terminal branches; most of them reach the crown, where they fan out to the periphery of the pulp. In the coronal pulp they branch abundantly, forming a subodontoblastic nerve plexus (Rashkov's plexus) in Weil's layer, containing both thick myelinated and thin non-myelinated fibers, from which branches extend to odontoblasts and dentinal tubules. Some of them end on the bodies of odontoblasts, others on odontoblastic Toms fibers, penetrating generally only 1/3 of the thickness of the dentin of a mature tooth. More careful and in-depth studies in recent years have shown that some unmyelinated nerve fibers can reach the mantle dentin, perhaps even the dentinoenamel junction.
Some of the nerve fibers end in the walls of the blood vessels in the central part of the dental pulp. Currently, connections between the nerves of the dental pulp and the sympathetic and parasympathetic parts of the autonomic nervous system have been established.
Most of the nerve endings in the area of odontoblast bodies are classified as receptors. Irritation of these receptors, regardless of the nature of the acting factor (pressure, cold, heat, chemicals), causes pain. At the same time, effector endings in the pulp of a formed tooth have recently been described.
Among the myelinated fibers of the pulp, there are more numerous a-fibers with a diameter of 1–6 µm, which mediate pain sensitivity, in particular, the sensation of acute localized pain, and p-fibers with a diameter of 6-12 µm, which presumably provide tactile signals.
Unmyelinated fibers with a diameter of 0.5–1.5 µm are also divided into several groups. Some fibers are predominantly vasomotor, regulating the tone of arterioles and blood flow in the pulp. Others contain neuropeptides (leu- and metenkephalins, cholecystokinin, somatostatin, vasointestinal polypeptide, etc.) and, being associated with blood vessels and odontoblasts, take part in the regulation of blood flow in the pulp, provide pain sensitivity, and also influence the development of inflammation.
Pulp of primary and permanent teeth.
There are three periods in the development of the pulp of primary teeth:
– a growth period of 4.2 years – from the beginning of prenatal crown formation to the completion of root development in the postnatal period;
– a ripening period of 3.7 years, which lasts from the completion of root development to the beginning of its resorption;
– a regression period lasting 3.5 years – from the beginning of root resorption to tooth loss.
The structure of the pulp of primary teeth generally corresponds to the structure of the pulp of permanent teeth. At the same time, in the central zone there is a higher cell content with fewer collagen fibers. Differences in the structure of the coronal and root pulp in baby teeth are less distinct than in mature teeth.
The pulp of baby teeth is abundantly supplied with blood, but the neural elements are much less developed in it.
The pulp of a permanent tooth during the formation of the crown is morphologically similar to the pulp of a baby tooth and is also characterized by a high concentration of dividing cells. The periods of pulp development in permanent teeth are longer. Thus, the growth period - from prenatal crown formation to the completion of root development takes about 12 years, the maturation period - up to 7-8 years, the regression period lasts most of a person’s life.
Innervation of the pulp -
The common sensory or afferent nerve for the maxillary and mandibular teeth are the II and III branches of the trigeminal nerve (i.e., the maxillary nerve and the mandibular nerve). In turn, nerves depart from them, which form plexuses - the superior dental plexus in the upper jaw and the inferior dental plexus in the lower jaw. In turn, bundles of myelinated nerve fibers branch off from these plexuses, which penetrate into the tooth cavity along with blood vessels - through the apical openings at the apexes of the roots. And, accordingly, forming a neurovascular bundle (tooth pulp) there.
The nerve fibers form a subodontoblastic nerve plexus, which is located under the layer of odontoblasts (also called Rashkov's plexus). Unmyelinated nerve fibers depart from this plexus, which are directed to the peripheral areas of the pulp, where they seem to entwine the odontoblasts, forming the so-called “nadodontoblastic plexus” between the odontoblasts and predentin. Some of the nerve fibers end in this plexus, but the rest of them penetrate into the dentinal tubules.