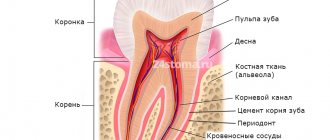
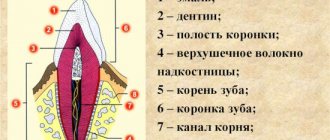
We always pay a lot of attention to tooth enamel; this is what we clean, treat it with care and try not to destroy it under any circumstances. But what is hidden under this shell, which protects the inner body of the tooth from bacteria and all sorts of negative factors? This is dentin - the inner shell, which is located both in the crown and in the root, and protects the pulp and nerve fibers. Dentin is essential to the functioning of each tooth and affects its appearance and health.
Let's try to highlight a few interesting facts to understand what dentin is and exactly what function it performs.
Tooth dentin: what is it, composition and structure
Dentin is a hard tissue located under the cement and enamel of teeth, respectively, in the roots and crown. It has a special structure and is second only to enamel in strength. Such properties are provided by a unique biochemical composition, which is represented by organic (20% by weight) and inorganic (70%) compounds, water (10%). The thickness of the dentin layer ranges from 2 to 6 mm. In the cervical region it is smallest. Its structure is presented in the following table:
| Types of fabric | Layer Features | Functionality |
| Dentinal tubules and tubules | Permeate the entire structure | The fibers that fill these elements are responsible for nutrition and metabolic processes in all dental tissues. Thanks to the tubules, dentin has high permeability |
| Peritubular dentin | Covers the surface of tubules and tubules | Minerals contained in this layer in large quantities nourish all dental tissues. |
| Interglobular dentin | Located between the dentinal tubules. There are two types: peripulpal, or predentin (surrounds the pulp), mantle (in contact with the enamel) | The processes of pear-shaped odontoblast cells, which make up predentin, deliver nutrients to the dental epithelium |
Text of the book “Fundamentals of clinical dental morphology: a textbook”
Chapter 5 Histology of teeth and surrounding tissues
5.1. Hard tooth tissues
5.1.1. Dentin Dentin (dentinum) is
the tissue that forms the bulk of the tooth and determines its shape. In humans, dentin in the crown area is covered with enamel, and in the root area - with cement. Thus, in a healthy tooth, dentin does not come into contact anywhere with the external environment and tissues surrounding the tooth. Like enamel, mature dentin is another ossified tissue of the tooth. In terms of its formation, structure and physiological characteristics, dentin is most likely closer to compact coarse-fibrous bone tissue, but differs from it in greater hardness and the absence of cells. Dentin and bone share some similar properties:
– growth by accession (apposition);
– the presence of a canalicular system containing cell processes, as well as specialized extracellular fluid and mineralizing matrix vesicles;
– structure of an organic matrix of collagens. However, between these two tissues there are obvious differences
differences.
Main features of dentin:
– dentin comes from ectomesenchyme (cells of the cranial part of the neural crest);
– dentin is restored and modified throughout the life of the individual;
– dentin is an acellular tissue (contains only processes of odontoblasts) that does not have blood vessels;
– odontoblasts participate in both the formation and mineralization of the organic basis of dentin.
Physical properties and chemical composition.
Dentin has a light yellow color, has some elasticity, it is stronger than bone and cement, but 4–5 times softer than enamel. The high hardness of dentin is explained by the presence in it of a large amount of mineral salts, the content of which reaches 70-80%, while the remaining 20-30% consists of organic substances (12-18%) and water (8-12%). In this regard, organic and inorganic components (matrices) are distinguished in mature dentin.
Organic matrix
Dentin is made up of collagen. Under an electron microscope, rather large fibers with an axial periodicity of 600–700 nm, characteristic of type 1 collagen, are visible. this is a genetically specific form of collagen found in the most ossified tissues (dentin, bone, cement).
In dentin, collagen fibers are oriented randomly, as in dense, unformed connective tissue. Only at the dentinoenamel border - in mantle dentin - are the fibers characterized by regularity, precise organization and orientation.
The collagen fibers of the dentin matrix are embedded in a basic amorphous substance consisting of glycosaminoglycans such as chondroitin sulfates. The latter can combine with non-collagen proteins, resulting in the formation of proteoglycans - the main components of the dentin matrix.
About 20% of the organic dentin matrix consists of non-collagen proteins, which play a role in the mineralization of dentin:
– proteins rich in gamma-carboxyglutamic acid;
– proteins that bind calcium;
– bone morphogenetic proteins;
– glycoproteins: fibronectin, osteonectin and, possibly, dentinonectin;
– proteins associated with membranes: calcium ATPase and alkaline phosphatase;
– collagenases, as well as collagen-digesting enzymes, necessary for the restructuring and change of the organic matrix.
In the organic basis of dentin, lipids (glycolipids and phospholipids) have also been identified, probably participating in the mineralization of the matrix.
Inorganic matrix
Dentin, like bone, cement and enamel, consists mainly of calcium phosphate in the form of hydroxyapatite crystals, which in dentin are small, thin, needle-shaped.
Transmission electron microscopy data made it possible to establish that these crystals are located both inside collagen fibers and between them. The inorganic dentin matrix contains small amounts of calcium fluoride (fluorapatite), calcium carbonate, magnesium and sodium.
5.1.1.1. Structure of dentin
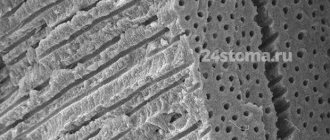
Dentin consists of a ground substance and many thin dentinal tubules (canaliculi dentales) that penetrate the ground substance (Fig. 89).
Rice. 89. Scheme of the structure of dentin and periodontium (according to R. Krstic).
1 – Toms fibers; 2 – odontoblasts; 3 – predentin; 4 – dentin; 5 – cellular cement; 6 – acellular cement; 7 – fibers of the periodontal ligament; 8 – periodontal blood vessels; 9 – bone alveolus; 10—Thoms granular layer (interglobular dentin); 11 – alveologingival ligaments; 12 – gums; 13 – enamel; 14 – gingival epithelium.
Dentinal tubules provide trophism to dentin and are thin cone-shaped tubes with a diameter of 1 to 3–4 μm, running in the radial direction from the dental pulp to the enamel or cement. They are wider in the inner parts of the dentin and gradually narrow outward.
The number of dentinal tubules varies in different parts of dentin. Due to the radial direction in relation to the tooth cavity, the tubules in the internal parts of the dentin (near the pulp) lie more closely: there are 50,000-75,000 dentinal tubules per 1 mm2 of dentin, and from 15,000 to 30,000 tubules closer to the periphery. There are more of them in the crown of the tooth than in the root. In molars there are 1.5 times less of them per 1 mm2 of dentin surface than in incisors.
The dentinal tubules in the crown are S-shaped curved, and in the area of the tooth root they are almost straight and run perpendicular to the axis of the tooth.
In the thickness of the dentin, the tubules branch and give off lateral processes that anastomose with each other (Fig. 90).
Rice. 90. Topography of dentinal tubules in peripulpar dentin (scanogram)
1 – dentinal tubules; 2 – Toms fibers; 3 – collagen fibers of the organic dentin matrix; 4 – boundary plate (Neumann’s shell).
The branching of the tubules is especially clearly visible at the dentinoenamel and dentinocement border, where each of them is divided into several terminal branches. In some cases, the tubules can cross the dentinoenamel border, penetrating into the thickness of the enamel and forming enamel spindles.
Due to the presence of a huge number of tubes penetrating dentin, the latter has high permeability. This circumstance is of clinical significance, causing a rapid response of the pulp to damage to dentin.
The ground substance surrounding the tubules is more compacted (hypermineralized) and homogeneous than the substance in the spaces between them. In this regard, peritubular (around the tubular) and intertubular (intertubular) dentin are distinguished.
Peritubular dentin is the layer of dentin that immediately surrounds each dentinal tubule, forming its wall (Fig. 91).
Rice. 91. Electronic scanogram of a dentin area.
1 – openings of dentinal tubules; 2 – peritubular dentin; 3 – intertubular dentin.
The thickness of the layer of peritubular dentin at the pulp end of the tube is about 40–50 nm, and at the dentinoenamel border – 500–700 nm. This dentin has a higher (35–40%) mineral content than intertubular dentin. The amount of organic matter in peritubular dentin is minimal, since it almost completely disappears during decalcification. Therefore, during caries during dentin demineralization, peritubular dentin undergoes intense destruction, which leads to the expansion of the tubes and an increase in its permeability.
During tooth development, intertubular dentin is formed first in both mantle and peripulpal dentin. It consists mainly of calcified collagen fibrils with a diameter of 100–200 nm, with hydroxyapatite crystals located along the axis of the fibrils.
The contents of dentinal tubules are varied:
– processes of odontoblasts (Toms fibers);
– unmyelinated nerve fibers;
– tissue dentinal fluid;
– non-calcified collagen fibrils (intertubular fibrils);
– hydroxyapatite crystals.
Some of these substances are involved in the sensory function of dentin, others are involved in the restructuring of its organic matrix. From the inside, the wall of the dentinal tubule is lined with a thin film of organic matter - the boundary plate (Neumann's membrane, or membrane), running along the entire length of the dentinal tubule and containing high concentrations of glycosaminoglycans. The tubes can serve as conductors for various substances necessary for dentin restoration, cellular debris from degenerated odontoblasts, microorganisms and their metabolic products. The latter can reach the pulp, causing some damage to it.
The processes of odontoblasts, being a direct continuation of the apical sections of their cell bodies, as a rule, stretch along the entire length of the dentinal tubules, ending at the dentinoenamel border. They contain few organelles, but a significant number of cytoskeletal elements, as well as vesicles, lysosomes and polymorphic vacuoles. The lateral branches of the processes are numerous in the predentin and internal parts of the dentin (100–200 µm from the border with the pulp), there are few of them in its middle parts and again many at the periphery. The branches form contacts with branches of neighboring odontoblasts, which can play a significant role in the transfer of nutrients and ions, as well as contribute to the spread of microorganisms and acids during caries.
Nerve fibers directed into dentin from the peripheral parts of the pulp usually penetrate into it to a depth of several micrometers, individual fibers - to 100–200 microns. Some of the fibers already in the predentin are divided into numerous branches; others pass inside the dentinal tubules along the process of the odontoblast or have a spiral course, entwining it and occasionally forming branches running at right angles to the tubules. Nerve fibers are usually thinner than the processes of odontoblasts and in some places form connections with them such as tight junctions and gap junctions. Most researchers believe that nerve fibers in the dentinal tubules influence the efficiency of odontoblast activity, that is, they are efferent, and do not perceive changes in their environment.
The main substance of dentin, located between the dentinal tubules, has a fibrillar structure and consists of collagen fibers and a homogeneous cementing substance (Fig. 9 2).
Rice. 92. Electronic scanogram of a demineralized area of peripulpar dentin.
1 – collagen fibers of the organic matrix; 2 – openings of dentinal tubules.
The location of collagen fibers and their structure change in different parts of dentin. In this regard, two layers of dentin are distinguished: outer, or mantle (mantle) dentin and inner, or peripulpal dentin. In mantle dentin, the predominant fibers are those running in the radial direction (Korff fibers), parallel to the course of the tubules. this arrangement remains closer to the occlusal surface of the tooth crown, and on the lateral surfaces of the crown and in the root area the radial fibers acquire an increasingly oblique direction.
Mantle dentin smoothly transitions into peripulpal dentin, in which, along with radial fibers, there are a large number of fibers located parallel to the surface of the pulp. The mantle dentin matrix is less mineralized than the peripulpal dentin matrix and contains relatively fewer collagen fibers.
In peripulpar dentin, the fibers are located tangentially (Ebner fibers) and almost at right angles to the dentinal tubules.
The location of Ebner fibers in the peripulpal dentin coincides with the location of the dentinal plates - layers of dentin deposited from the inside, from the pulp side, during the development of the tooth. The expression of rhythmic growth and layered dentin deposition are Owen's contour lines and Ebner's growth lines.
Owen's lines usually run at right angles to the dentinal tubules and correspond to periods of rest in the activity of odontoblasts. During this period, less intense calcification of the dentin substance and the formation of very small interglobular spaces occurs (Fig. 93).
In baby teeth and first permanent molars, a contour (neonatal) line is often visible, separating the layer of dentin that formed during the prenatal period of life from the dentin that formed after birth. According to B. Orban [72, 73], this line corresponds to incompletely calcified dentin that arose in the first 2 weeks after birth due to metabolic disorders during the period of adaptation of the newborn to sudden changes in environment and nutrition.
The number of Owen lines can increase in pathological conditions of the body (long-term illnesses accompanied by increased body temperature, unstable nutrition, etc.).
Rice. 93. Microphotograph of a longitudinal section of a tooth (from L.I. Falin).
1 – Owen lines; 2 – dentinal tubules.
The thinner Ebner lines, directed almost perpendicular to the dentinal tubules, are located closer together than the Owen lines, with a periodicity in the crown of about 18–20 μm. Between Ebner's lines there are lines, the distance between which is usually constant (about 4–5 µm) depending on the location - at the apex or at the root of the tooth. It is assumed that the latter reflect the daily rhythm in the formation of dentin, and the Ebner lines correspond to the 5-day cycle of the formation of the organic dentin matrix, i.e., periods of less mineralization of the main substance of dentin.
Secondary and tertiary dentin.
Dentin deposited in the teeth of an adult during his life is called secondary (regular, or physiological) reparative dentin (Fig. 94).
In addition to the slower rate of formation, it differs from primary dentin (which arose during the embryonic development of the tooth) in having a less regular structure. This is expressed in a change in the course and number of dentinal tubules and collagen fibers with a lower degree of mineralization. The most active deposition of secondary dentin occurs in the side walls and in the roof of the pulp chamber, and in multi-rooted teeth - in its bottom. In this regard, with age, the shape of the pulp chamber changes: the pulp horns become less protruding, and its volume decreases. The intensity of secondary dentin deposition in men is higher than in women; it decreases with age. The thickness of the secondary dentin layer can be used as one of the indicators to estimate the dental age of an individual.
Rice. 94. Microphotograph of a vertical section of a mandibular molar.
1 – secondary (reparative) dentin; 2 – vestibular horn of the pulp; 3 – lingual horn of the pulp; 4 – dentin; 5 – enamel; 6 – tooth cavity.
The production of secondary dentin sharply increases with the destruction or abrasion of enamel and exposure of dentin (caries, increased tooth abrasion, exposure to chemicals, etc.). At the same time, in areas of the pulp corresponding to the area of tooth damage, there is a deposition of more or less significant masses of replacement dentin, which can protrude into the tooth cavity and change its configuration. Such dentin is called tertiary (irregular). Unlike secondary dentin, which completely lines the surface of the pulp facing the dentin, the formation of tertiary dentin occurs more or less locally, that is, only in places of the strongest influence of an unfavorable factor (Fig. 95).
The main function of tertiary dentin is to protect the dental pulp from the spread of bacteria, toxins, etc. It can form in any part of the wall of the tooth cavity, but most often appears in the area of the pulp horns. According to its structure (presence of osteoblasts, irregular course of dentinal tubules or even their absence, weak mineralization), it is closer to the bone and is therefore called osteodentin by some authors. In the dental cavity of elderly people, foci of osteodentin are also normally found, which can significantly change the configuration of the cavity, up to its complete obliteration.
Rice. 95. Topographical features of tertiary dentin (scheme).
1 – enamel; 2 – dentin; 3 – tooth cavity; 4 – defect in the area of the tooth neck; 5 – tertiary dentin; 6 – enamel defect (caries).
Denticles.
In the dental pulp, round or irregularly shaped bodies are sometimes observed, consisting of dentin or dentin-like tissue, which are called denticles, or pulp stones. According to their position in the pulp, they are divided into free, that is, lying directly in the pulp; parietal, maintaining connection with the tooth wall; interstitial, which arise when free or parietal denticles are overgrown with new layers of secondary dentin (Fig. 96).
As a result, the denticle becomes immured in the wall of the tooth (this process is more often observed at the root of the tooth, closer to its apex). Depending on the structure, it is customary to distinguish between highly organized (canalized) and low-organized (devoid of canaliculi) denticles. The sources of their formation are odontoblasts. As noted, denticles have the structure of dentin or dentin-like tissue, therefore they are called true denticles, in contrast to false denticles, which are foci of limited calcification in the pulp tissue.
The sizes of denticles are very variable - from barely noticeable grains to 2–3 mm in diameter. As a result of their growth, denticles can merge with each other, filling the entire tooth cavity or root canals, preventing endodontic manipulation. By squeezing the nerve fibers of the pulp, denticles can cause pain of a pulpitic nature. The reasons for their formation are not clear enough. Denticles are found both in the teeth of elderly people and in the teeth of young people, and even in tooth germs before their eruption [42, 61].
Rice. 96. Topography of denticles in the dental pulp (diagram).
1 – enamel; 2 – dentin; 3 – interstitial denticles; 4 – free denticles; 5 – parietal denticles; 6 – dental pulp.
5.1.1.2. Age-related changes in dentin
Dentin is a living tissue that is produced continuously throughout life. The formation of secondary and then tertiary dentin leads with age to a decrease in the size and volume of the tooth cavity - a process called pulp recession by clinicians. In addition, in the teeth of elderly people there are areas of dentin in which lime salts are deposited not only in the main substance, but also in the dentinal tubules and processes of degenerating odontoblasts. As a result, obliteration (“physiological” sclerosis) occurs, i.e., complete closure of the lumen of some groups of dentinal tubules, while the refractive indices of the tubules and the main substance are aligned and such areas look transparent. These areas are called sclerotic (transparent) dentin. Such dentin is also formed during caries or increased wear of teeth (“pathological” sclerosis), which can be considered as a protective reaction of the tooth to the action of destabilizing factors, which protects the pulp from irritation and infection (Fig. 97).
Rice. 97. Microphotograph of a vertical section of a mandibular incisor.
1 – enamel; 2 – dentin; 3 – dead paths in dentin; 4 – sclerotic dentin; 5 – reparative dentin; 6 – tooth cavity.
The formation of transparent dentin most often begins in the apical part of the root and progresses slowly towards the crown.
Typically, mineralization occurs first in the periodontoblastic space, and then captures the odontoblast process, less often vice versa.
Due to the fact that dentin sclerosis reduces its permeability, it can prolong the period of pulp viability. Obliteration of the dentinal tubules also leads to a decrease in tooth sensitivity.
With age, especially with increased tooth abrasion, the death of part of the odontoblasts and their processes and blockage of the inner ends of the corresponding dentinal tubules with tertiary dentin are also often observed. The contents of such tubules disintegrate, and the cavities of the tubules are filled with air or other gaseous substances. As a result, on thin sections of a tooth, groups of such tubules appear black in transmitted light (Fig. 98).
E. Fish [51] called groups of such tubules “dead paths”. The sensitivity of dentin in these areas is reduced.
In most cases, the dead spaces on the pulp side are, as noted, closed by the formation of irregular tertiary dentin.
Rice. 98. Microphotograph of a section of dentin.
1 – peripulpar dentin; 2 – pulp; 3 – tertiary dentin; 4 – “dead paths” of dentin.
5.1.1.3. Morphology of dentin in a clinical aspect
The “instant” reaction of the pulp to damage to dentin is due to the presence of a system of dentinal tubules, which can become pathways for the invasion of microorganisms, contributing to the rapid spread of the carious process. It has been shown that in cases where 1 mm2 of the dentin surface remains unprotected by enamel, about 30,000 odontoblasts are destroyed. Toxins, drugs and chemical reagents can penetrate through unprotected dentin, and the receptor apparatus of the pulp is also vulnerable to thermal influences. Dentin is most sensitive in the area of the dentinoenamel junction.
With demineralization of dentin, destruction of the dentinal processes of odontoblasts is observed. Under the action of enzymes secreted by microorganisms, the organic matter of demineralized dentin is dissolved. Along the periphery of the carious cavity towards the dental pulp, the dentinal tubules expand and become deformed. Closer to the tooth cavity there is a layer of compacted transparent dentin with significantly narrowed dentinal tubules.
The morphology of dentin must be taken into account when determining the treatment tactics for defects of hard dental tissues of both carious and non-carious origin.
One of the important clinical stages in the treatment of caries is the removal of softened and discolored (pigmented) dentin using various dental instruments (excavators, burs, etc.). An exception is the treatment of deep caries. In these cases, pigmented dentin is left at the bottom of the crown cavity and therapeutic pads containing calcium hydroxide (calmicin), zinc-eugenol paste and other materials are placed on it for several weeks or months. During this period, pulp cells become odontoblasts through cytodifferentiation, and the latter form reparative dentin, after which the dentist can remove pigmented dentin without fear of opening the tooth cavity.
Types of dentin
Dentin is constantly changing. The following types are distinguished:
- Primary. It is formed during intrauterine development of the fetus. It is preserved until the tooth erupts.
- Secondary (replacement). Its formation begins when a tooth appears above the gum. Lasts for life. It differs from the primary one in its slower pace of development and in a large amount of organic matter. Has high permeability.
- Tertiary (irregular). Appears in case of injury, disease and tooth preparation. Its occurrence is a response to an inflammatory process or external irritants. Tertiary dentin performs a protective function. During its formation, the structure of the tissue changes: the tubules have a chaotic arrangement or are absent altogether (usually due to severe inflammation). But the process of formation of tertiary tissue is not endless.
There is also sclerosed (transparent) dentin, which appears as a result of the deposition of the peritubular layer in the tubules. This leads to their gradual narrowing. Similar changes can occur with age. As lime salts are deposited on the walls of the tubules, permeability is reduced, thereby prolonging the viability of the pulp.
Types, location areas
From an anatomical point of view, the mantle and peripulpar layers of dentin are distinguished. The first is located immediately under the enamel, the second - above the pulp. Histologically, dance and radial layers are distinguished, the differences of which relate to the location of collagen fibers.
The following types of fabrics are distinguished:
- primary, beginning to develop before the unit erupts;
- secondary, the development of which begins after the tooth has erupted;
- tertiary, also called reparative, irregular or replacement, appearing as a response to injuries and other damage.
The predentin zone is also distinguished, where secondary and tertiary species begin to form. This region belongs to the germinal region, where the process of formation of new layers begins.
Diseases
Dentin, like other tissues, is subject to age-related changes. The volume of minerals decreases, and degenerative processes begin. The tubules become narrower, sclerosis occurs, and the trophic function practically stops. Metabolic and other processes slow down, which negatively affects the strength and condition of tissues. Resistance to the development of caries decreases, teeth become thinned by various negative factors.
Caries is the main disease diagnosed most often. This is due to various nuances, for example, a local decrease in acidity, demineralization, an increase in the value of carbohydrates and others. With the death of odontoblasts and narrowing of the tubules, tissue nutrition deteriorates, which also makes the layer vulnerable to pathogenic bacteria.
Recovery methods
For treatment, it is recommended to remove the affected tissues followed by filling. After cleaning, the cavity is treated with antiseptics, which protects it from further problems. Composite fillings restore the shape and size of the tooth and allow for proper load distribution. The color is selected in accordance with the shade of the surrounding fabrics.
To prevent the development of diseases, it is recommended to regularly visit the dentist. During a routine examination, problems will be identified in a timely manner, which will allow treatment to begin while preserving tissue.
Functionality and regenerative qualities of dentin
Dentin consists of several layers. They, as already mentioned, protect the pulp from bacterial infections. In addition, this elastic fabric acts as a shock absorber for the enamel. It is also responsible for tooth sensitivity. Thanks to dentin, the pulp responds in a timely manner to infection, injury, and thermal irritants.
Many people believe that the color of teeth is determined by the enamel. In fact, it is translucent, and the snow-whiteness of a smile depends on dentin, which comes in different shades - from white to gray and yellowish. Often yellowness indicates high mineralization of tissues, and therefore the health of the teeth.
Dentin has the ability to regenerate thanks to monoblast cells. Recovery is possible only if the innervation of the dental tissues is preserved. After depulpation, regeneration processes stop.
Basic diagnostic methods
Independent determination of dentin caries is possible based on pain and other unpleasant symptoms. However, only a doctor can make an accurate diagnosis after conducting a full dental diagnosis. It includes basic and additional research methods.
The main diagnostic methods for dentin caries include the following:
- Probing - using a sharp probe, the doctor determines the presence and depth of carious cavities. If the bottom of the cavity has a soft structure and a light brown color, this may indicate an acute course of caries. Dense pigmented dentin in the bottom area indicates a chronic form of the disease. Also, with the help of probing, you can detect hanging edges of tooth enamel, chips on it, and by the localization of pain during probing, determine the depth of the carious lesion.
- Percussion is tapping on the teeth with tweezers or the back of a dental probe.
- Palpation - feeling.
These methods are used to determine the viability of the pulp, which is especially important in differential diagnosis.
Additional research methods include:
- Thermometry - measuring the temperature of dental tissues.
- Electroodontometry is the study of pulp using electric current.
And the following methods are used to assess the condition of the pulp:
- X-ray - an X-ray of the tooth helps determine the exact location of the carious cavity and its depth.
- Transillumination - the transillumination method is widely used in the diagnosis of hidden dentin caries, for example, with an isolated, atypical form of progression. When transilluminated, healthy tissues appear transparent, while those affected by caries create a shadow effect.
When the doctor has made a preliminary diagnosis based on the above methods, differential diagnosis of dentin caries with other types of dental diseases - enamel caries, pulpitis, periodontitis may be required.
Caries: causes of development, diagnosis, therapy
Caries is the most common disease of dentin. Develops with insufficient oral care, low levels of acidity in the mouth, abuse of sweets, and genetic predisposition. The onset of caries development is the stage of a white or pigmented spot. At this stage, dentin is not yet affected. The internal tissues of the tooth are involved in the painful process if left untreated. Depending on the degree of their damage, they distinguish between medium caries, when the middle layers of tooth tissue are affected, and deep caries, in which the pathogenic process almost reaches the pulp.
With caries, the degree of mineralization of tissues decreases and their structure changes. The processes of some odontoblasts are destroyed. The inflammatory process begins. If it is not eliminated in time, it affects the pulp. Diagnosis of the disease is not a problem for the dentist. Upon examination, a carious cavity filled with soft dentin is noticeable. Therefore, it is important to consult a doctor in time. When caries is diagnosed, treatment involves the following:
- administration of anesthesia (if necessary);
- removal of infected tissue;
- cavity disinfection;
- installation of a seal.
In case of deep caries, when a pathological process has developed in the root canals, treatment is mainly carried out in several stages. First, a temporary filling is installed. Various materials can be used for it, including artificial dentin - powder made from kaolin and zinc sulfate. It is diluted with water. Oil dentin is also used in dental practice. The powder is similar in composition to aqueous powder, but is mixed with a mixture of clove and peach oils.
Such components will protect the tooth cavity from bacteria and food debris getting inside. With the help of a sealing material, the medicine will remain in the canal for the required time. Among the properties of artificial dentin, it is worth highlighting its low strength. Therefore, the final stage of treatment should be replacing the material with a permanent filling.
To strengthen the enamel and dentin, remineralization is carried out. To do this, fluoride-containing varnish is applied to the teeth and special toothpastes are used. After the procedure, the enamel becomes less permeable. Carious cement has a layered structure. It is little permeable or impenetrable. Beneficial substances actively penetrate into demineralized dentin to a great depth and react with its inorganic component.
How does a tooth hurt with dentin caries?
Different types of pain are characteristic of different stages of caries. When dentin is damaged, the stages of medium and deep caries are distinguished. In the first case, the carious cavity is located closer to the enamel; in the deep stage, it is as close as possible to the area of the dental nerves.
The middle stage of dentin caries is characterized by a painful reaction in response to temperature or taste stimuli, the pain quickly passes, and the intervals without pain are quite long.
If caries is in the stage of deep damage to dentin, it is characterized by intense long-term pain with short intervals without pain.
Deep caries is the most dangerous, because at any moment it can be complicated by pulpitis, periodontitis, purulent inflammation, and the spread of infection beyond the dental tissues. But even the moderate one can turn into the deep stage at any moment, so if you have a toothache of any nature, you should consult a dentist as soon as possible.
Pathological abrasion of teeth
Abrasion occurs when the bite is incorrect, when the chewing load is distributed unevenly, in the absence of some teeth, constant exposure of the enamel to aggressive substances, and vitamin deficiency. Among the main causes, it is also worth mentioning bruxism - involuntary grinding of teeth during sleep. In these cases, the enamel is erased first, followed by the dentin.
The choice of treatment methods depends on the provoking factor. They may include wearing mouthguards, inlays, and temporary dentures. This allows you to adjust the height of the teeth. When the patient gets used to it, prosthetics are performed (usually with non-removable structures).
Isolated dentin caries: what are its features
Sometimes lesions and extensive carious cavities form in the dentin of a permanent tooth while maintaining the integrity of the enamel. This is how isolated, atypical caries develops. Its difference from the classical form is that the carious lesion does not affect the enamel, but immediately passes to the dentin.
This happens, for example, in cases where a person uses fluoride preparations for a long time for preventive purposes. This leads to strengthening of the enamel located on top of the affected dentin, and, as it were, “seals” the pathological process inside the tooth.
Cost of services
If treatment is started on the day of treatment, consultation and treatment plan are free
| Treatment of superficial caries with the installation of a light-curing filling | RUB 3,800 |
| Treatment of medium caries with light filling | 4,200 rub. |
| Treatment of deep caries with light filling | RUB 5,900 |
| Complex treatment of 1 tooth canal | 1,300 rub. |
| Filling 1 tooth canal | 1,400 rub. |
| Consultation | 550 rub. |
| Titanium anchor pin | 1,300 rub. |
| Anchor pin (carbohydrate, fiberglass) | RUB 1,850 |
Hypophosphatasia
The peculiarity of this pathology is a reduced level of alkaline phosphadase in the blood, as well as impaired bone mineralization. The disease is inherited in an autosomal recessive manner. It is characterized by skeletal deformities and changes in the structure of the lower extremities.
Due to pathological root resorption, temporary incisors fall out prematurely. Abnormalities of calcification are observed in primary teeth, while the crowns retain their normal size and shape. Uneven calcification is observed only in permanent molars and incisors. Signs of hypoplasia are obvious on the enamel.
X-ray shows:
- osteoporosis of bone and underdevelopment of the alveolar process;
- root resorption too early;
- resorption of the root tips of intact teeth;
- W-shaped roots;
- sometimes - taurodontism.