Performing syndrome diagnosis
To properly check for the presence of a disease, it is necessary to perform a full range of various procedures. In particular, diagnosis of stylohyoid syndrome includes a number of actions and manipulations.
First of all, a professional examination of the patient is performed, as a result of which the doctor examines and identifies the compaction of the bone growth in the area of the anterior zone of the cervical spine of the patient. If you press on this part, the person should experience pain, and his health will deteriorate greatly.
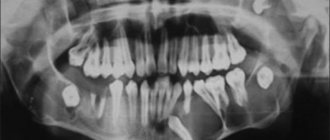
Secondly, an X-ray of the facial skeleton, skull bones, and neck is taken.
At the time of diagnosis, you should carefully approach the procedures, because this disease can easily be confused with other similar pathologies, the symptoms of which are very similar. As an example, suppuration of the tonsils can be cited.
Fracture of the lower jaw
With a unilateral condyle fracture, the lower jaw moves to the affected side when opening the mouth. An open bite only in the anterior region indicates a bilateral fracture of the condylar processes. In case of a fracture of the head and ramus of the lower jaw without displacement of the fragments, valuable information can be obtained by placing a load on the lower jaw. Pressure on the chin from front to back or on the angle of the lower jaw from bottom to top causes pain in the area where the fracture line is located. When the fragments are displaced, by palpation in this place, uneven contours of the bone and bone protrusions can be determined. The single or multiple nature of the fracture of the lower jaw can also be determined using a wooden spatula. On the side of the fracture, the patient cannot hold the spatula between the lateral teeth. If he cannot hold the spatula between the front teeth or between the lateral teeth on both sides, then this indicates a bilateral fracture of the mandible in the area of the body, ramus or condylar process of the mandible. Features of the location of the fracture line and the direction of displacement of fragments are determined on radiographs of the lower jaw. The listed signs are absent in SBD of the temporomandibular joint.
Clinic
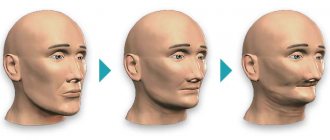
In the presence of an elongated and/or curved styloid process, or a calcified stylohyoid ligament, or a calcified stylohyoid fold, or elongated horns of the hyoid bone, excessive pressure of these structures occurs on the internal and external carotid arteries. Due to this, in the areas fed by the carotid arteries, many seemingly unrelated clinical symptoms appear, such as:
- sensation of a foreign body in the throat;
- chronic inflammation of the pharyngeal mucosa;
- pain in the maxillary joint;
- pain and noise in the ears;
- unilateral and bilateral orbital or headache;
- “shooting” pain when turning the head.
According to the literature, patients with stylohyoid syndrome most often complain of poorly localized pain with unilateral localization in the upper anterior part of the neck and irradiation to the pharynx, root of the tongue, and ear. In this case, pain can spread to the temporomandibular joint, lower jaw, temporal, buccal areas, and submandibular triangle. In some patients, pain occurs in the teeth of the upper and lower jaws. M. Kiely et al. (1995) described the spread of pain to the sternocleidomastoid muscle, and D. Savic (1987) - to the supraclavicular fossa, shoulder girdle and anterior chest wall. Patients usually characterize the pain as dull, constant with periods of intensification and weakening. Its intensity increases towards the end of the day, intensifying when turning or throwing back the head, after a long conversation or singing, or changes in weather conditions.
Patients usually complain of pain in only one organ, most often in the pharynx, ear, temporomandibular joint, and only a detailed survey allows us to clarify its localization and areas of distribution. Some patients develop glossopharyngeal neuralgia with its characteristic painful paroxysms. Dysphagia is a common symptom of the disease, and difficulty swallowing is usually associated with a significant increase in pain in the throat and ear. Some patients are bothered by the sensation of a foreign body in the throat, others are worried about a “constantly sore throat”; they may experience pharyngeal spasm, persistent dry cough without objective signs of inflammation in the upper respiratory tract.
Stylopharyngeal syndrome
As a rule, it is right-sided, since the right styloid process is normally longer than the left by an average of 0.5 cm. Pain occurs as a result of pressure, for example, by an elongated and inwardly curved styloid process, on the tissue in the area of the tonsillar fossa and irritation of the nerve endings of the glossopharyngeal nerve. The intensity of pain varies greatly - from minor pain or the sensation of a foreign body in the throat, especially when swallowing, to sharp, severe constant pain in the throat and tonsils, radiating to the ear. Some patients also note pain on the front surface of the neck, in the area of the hyoid bone. Occasionally, these sore throats are mistakenly associated with pathological changes in the tonsil and it is removed, and ongoing pain is explained by irritation of the nerve endings by a postoperative scar. However, stylopharyngeal syndrome should be differentiated not only from damage to the tonsils, for example by a chronic inflammatory process, but also from neuralgia of the glossopharyngeal nerve. Neuralgia of the latter is characterized by paroxysmal burning or shooting pains in the pharynx, tonsils, root of the tongue, radiating to the ear, which occur during talking, laughing, coughing, yawning and eating.
Styloid-carotid syndrome (“carotid artery syndrome”).
The pathogenesis consists of pressure from the tip of the elongated and outwardly deviated styloid process on the internal or external carotid artery near the bifurcation of the common carotid artery, irritation of the periarterial sympathetic plexus and pain receptors. When the internal carotid artery is irritated, the pain is constant and is felt in the frontal region, orbit, eyes, that is, in the area of branching and blood supply of the internal carotid artery or its branches, in particular the orbital artery. Due to the pressure of the appendage on the external carotid artery, pain radiates along its branches to the temple, crown, face (below the eye).
- Why does the jaw hurt on one side when chewing near the ear: what does pain on the right and left mean, how to treat it?
Radiation diagnosis of stylohyoid syndrome (clinical observation)
Authors: A. G. Lamper, M. V. Vishnyakova, E. A. Stepanova
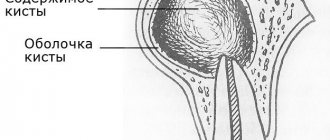
Stylohyoid syndrome (SHS), or Eagle syndrome, is the generally accepted name for a clinical symptom complex associated with abnormalities in the size and position of the styloid process of the temporal bone (STST). Changes, as a rule, concern the structures of the stylohyoid complex (SHC), which is formed by the SHC, stylohyoid ligament and hyoid bone [9].
Patients may present a whole range of nonspecific complaints, with which they turn to specialists of various profiles, without receiving adequate treatment for a long time. Among them:
– pain, more often, in the pharynx, ear and temporomandibular joint, with irradiation to the lower jaw, temporal and buccal areas, submandibular triangle, teeth, root of the tongue [9]; – dysphagia with increased pain in the throat and ear during swallowing (possible sensations of a foreign body in the throat or a “constantly sore throat” [3, 4]; – persistent dry cough without objective signs of inflammation in the upper respiratory tract [1, 2, 5, 7];
– limitation of head movements and a feeling of “stiffness” in the neck muscles [6, 8].
Changes in the stylohyoid complex occur in 20–30% of adults. However, due to the lack of awareness among practitioners about SPS, its timely recognition is significantly delayed.
Clinical observations
Patient K., 30 years old, considered himself sick for two years when he first accidentally discovered a small round painless formation on the left anterolateral surface of the neck. Was consulted by a surgeon. To clarify the nature of the formation, a puncture was performed, the result of which was inconclusive.
Over the subsequent time, the formation slowly increased in size, difficulty swallowing and limitation of lateral movements of the neck. For further examination and treatment he was hospitalized at MONIKI. Objectively: The face is symmetrical. The skin is of normal color and moisture. Opening the mouth is free, fully, painless.
From the oral cavity – no features. Phonation is not impaired. During swallowing, a shift of the larynx to the right is observed. Sensitivity is not impaired. On the left anterolateral surface of the neck, palpation reveals a fixed, painless, hard oblong formation about 5 cm long, not fused to the surrounding tissues.
Regional lymph nodes are not palpable. Thyroid gland without pathology on ultrasound.
When radiography of the cervical spine in direct and oblique projections: on the left, an additional S-shaped formation was identified between the styloid process and the body of the hyoid bone, consisting of intercalary bones connected to each other by joint-like joints (Fig. 1). More complete information was obtained from computed tomography (Fig.
2): the left styloid process of the temporal bone is thickened, connected to the body of the hyoid bone through two intercalary bones that form false joints among themselves. The left greater horn of the hyoid bone is connected by the calcified thyrohyoid ligament to the horn of the calcified thyroid cartilage. The right SHOVK is elongated and thickened.
Conclusion: CT picture of an anomaly in the development of the spinal cord with the formation of synostoses and false joints between the hyoid bone, the styloid process of the left temporal bone and the superior horns of the thyroid cartilage. Based on clinical and radiological studies, the diagnosis of stylohyoid syndrome was confirmed.
During the operation, the left styloid process of the temporal bone, the stylohyoid ligament and the left horn of the hyoid bone were removed. The removed material contained bone fragments of a compact structure with areas of hyaline cartilage and fine calcium deposits. During control radiography, in the area of the surgical intervention, a non-removed fragment of the distal part of the calcified stylohyoid ligament is identified, connecting to the body of the hyoid bone (Fig. 3).
The postoperative period proceeded without complications. The patient was discharged in satisfactory condition for follow-up.
Discussion
Anomalies of the SOVK are associated with disturbances in the development of the branchial arches. In the mesenchyme between the gill pouches, cartilaginous gill arches are formed. Of particular importance are the first two of them – the visceral arches, on the basis of which the visceral skull develops [12, 13].
In the spectrum of changes in the spinal cord, the following types of anomalies may occur: lengthening of the spinal cord, ossification or calcification of the stylohyoid ligament (complete or partial, unilateral or bilateral), possible total damage or the formation of diarthrosis-like joints.
In the pathogenesis of SPS, pathological deviation of the process in the posteromedial direction, often in combination with its elongation and curvature, is important. This leads to pressure on the surrounding muscles, the glossopharyngeal nerve, the sympathetic plexus of the internal carotid artery, and the lateral wall of the pharynx.
Moreover, the value of the angle of deviation at which the apical part of the process comes into contact with these anatomical formations is inversely dependent on its length and the severity of the curvature [11]. Clinical diagnosis is very problematic, primarily due to the lack of characteristic objective symptoms.
During the examination, you can palpate the apex of the process, as well as identify pain in the projection of the styloid process, anterior palatine arch, stylohyoid, masticatory (pterygoid, temporal) and sternocleidomastoid muscles. In addition, there is no consensus on the normal length of the styloid process of the hyoid bone.
Thus, previously a SHOVK of more than 30-33 mm was considered elongated.
However, later data (based on mass orthopantomographies) showed that the average length of the CV joint should be considered 45 mm, and this figure varies in different age and sex groups (42 mm in women under 35 years of age; 49 mm in men over 45 years of age), and fluctuations in the length of the process can vary from its complete absence (on one or both sides) to fusion of its apex with the lesser horn of the hyoid bone [7]. At the same time, modern possibilities for surgical treatment of SPS increase the relevance of accurate diagnosis of the disease, the main role in which is played by radiation research methods - traditional radiography and computed tomography.
Conclusion
The interest of this clinical observation, in our opinion, is due to a fairly typical medical history of a patient with stylohyoid syndrome, the diagnostic problems of which are associated mainly with the lack of awareness of doctors of various specialties, including practical radiologists, about the existence of such a disease.
Mentions of it are found, as a rule, in specialized literature on otorhinolaryngology, maxillofacial surgery and neurology.
In fact, the use of a selected set of complaints, objective signs and a correct diagnostic algorithm, including radiography and CT, facilitates the recognition of SPS, planning and implementation of corrective surgery.
Literature
Akberov R.F., Khabibullin I.R. // Vertebroneurology. – 1992. – No. 2. – pp. 46–47. Grinberg L. M. Neurology of the face / ed. V. A. Karlova. Moscow, 1991. – pp. 57–59. Danilov A. B. Pain syndromes in neurological practice / ed. A. M. Veina. Moscow, 1999. – P. 13–51. Lebedyantsev V.V., Shulga I.A., Ovchinnikova N.K.
XI Scientific and Practical Conference of Otorhinolaryngologists of the Orenburg Region. – 1998. – P. 23–24. Lebedyantsev V.V., Shulga I.A. On the pathogenesis of stylohyoid syndrome // News of otorhinolaryngology and logopathology. – 2001. – No. 2. – pp. 32–36. Carter L. Soft tissue calcification and ossification. In: White SC, Pharoah MJ, editors. Oral radiology, principles and interpretation.
Missouri: Mosby, 2004. – R. 597–614. Gokce C., Sisman Y., Tarim Ertas E., Akgunlu F., Ozturk A. Prevalence of styloid process elongation on panoramic radiography in the Turkish population from Cappodocia region // Eur J Dent. – 2008. – No. 2. – R. 18–22. Gözil R., Yener N., Calgüner E., Araç M., Tunç E., Bahcelio lu M.
Morphological characteristics of styloid process evaluated by computerized axial tomography // Ann Anat. – 2001. – No. 183. – R. 527–535. Krennmair G., Piehslinger E. Variants of ossification in the stylohyoid chain // Cranio. – 2003. – No. 21. – R. 31–37. Baekim CC, Mutlu H, Güngör A, et al. Evaluation of styloid process by three dimensional computed tomography // Eur Radiol. – 2005. – No. 15.
– R. 134–139. Prasad KC, Kamath MP, Reddy KJ, Raju K., Agarwal S. Elongated styloid process (Eagle's syndrome): a clinical study // J Oral Maxillofac Surg. – 2002. – No. 60. – R. 171–175. Ryan D. Murtagh, Jamie T. Caracciolo, and Gaspar Fernandez CT Findings Associated with Eagle Syndrome AJNR Am // J Neuroradiol. – 2001. – No. 22 (August). – R. 1401–1402. Ramadan SU
, Gokharman D., Tuncbilek I., Kacar M., Kosar P., Kosar U. Assessment of the Eagle's syndrome stylohoid chain by 3D-CT // Surg Radiol Anat. – 2007. – No. 29. – R. 583–588.
The materials are copyrighted, reprinting is permitted only with the written consent of the editors.
Source: https://vestnik.medsi.ru/publications/259/
Diagnostics
To make a diagnosis, it is very important to carefully collect complaints and medical history. So, it is necessary to establish when the painful sensations appeared, what nature they are, what provokes an increase in pain, and what causes a weakening. It is necessary to accurately determine the areas where pain occurs and where it radiates. This is important for differential diagnosis with neuralgia of other nerves (occipital, glossopharyngeal, upper laryngeal, trigeminal, auriculotemporal).
It is mandatory to examine the throat to rule out pharyngitis and tonsillitis.
An additional examination method is skull radiography (or targeted radiography of the stylohyoid process).
Causes, symptoms and treatments for stylohyoid Eagle-Sterling syndrome
Under the lower jaw there are numerous anatomical formations, diseases of which can manifest as pain in the neck. Unpleasant sensations occur in the following cases:
- Pathological changes in the lymph nodes with lymphadenitis. Inflammation is accompanied by sharp pain in the neck, radiating to the jaw, and an increase in temperature.
- The appearance of metastases - tumors of the lymph nodes under the lower jaw. The pain becomes chronic, and the body temperature rises and does not fall for a long time. The person experiences general weakness, loses weight and feels unwell.
- Increased sensitivity of the tongue when eating sour, spicy, cold or hot foods.
- Glossitis is an inflammation of the tongue, in which it becomes bright red and swollen.
- Salivary stone disease, accompanied by swelling of the lower jaw, secretion of pus by the glands in the oral cavity, fever and pain in the neck, ear and jaw.
- Pharyngitis, tonsillitis, sore throat.
- Jaw fractures are accompanied by pain in the neck under the jaw, hemorrhages and swelling.
- Neuralgia of the glossopharyngeal nerve. The disease is extremely rare and starts from the root of the tongue or tonsils, moving to the ears and neck.
- With tumors of the larynx, the pain gradually intensifies and moves lower into the neck and chest. Pain in the neck and lower jaw, soreness, cough, and voice changes occur.
Types of neck and jaw pain
The neck and lower jaw can hurt in different ways, depending on the causes and disease that caused the disease. Let's consider the options for how pain can manifest itself.
Intense pain on the sides of the neck under the jaw
The neck under the jaw on the left and right can hurt for various reasons:
- inflammation of the jaw bone;
- injury;
- lymphatic pathologies and oncological diseases;
- dental problems.
It doesn’t matter what symptoms accompany the pain, you need to consult a specialist. When pain does not cause discomfort, this is not a reason to ignore the need to see a doctor.
There are many diseases that do not show noticeable signs at the beginning of their development. Over time, mild discomfort develops into severe, sharp pain that cannot be tolerated.
In this regard, it is necessary to fight the disease not with pain relief or lotions, but with the help of comprehensive medical treatment.
It's a dull pain
Pain in the neck, radiating to the jaw and having an aching character, can be caused by such reasons as:
- Migraine. The pain can be localized on one side, intensifying with bright light or changes in lighting, as well as with loud extraneous sounds. Additional symptoms of migraine include vomiting, nausea, extreme thirst, blurred vision, etc.
- Infectious dental diseases.
- Corotidynia.
Pain under the jaw on the left
- Pain in the navel area: causes and treatment
- How to calculate your ideal weight
Pain in the neck and lower jaw on the left can be caused by a heart attack or angina as a result of impaired blood flow. Problems can be diagnosed by burning, acute pain in the chest. In this case, it is important to quickly consult a doctor who will prescribe the correct treatment and prevent death.
Pain when pressing
Pain in the neck and jaw when pressed may indicate:
- osteogenic sarcoma;
- neuralgia of the ear node;
- sialoliths;
- inflammation of the lymph nodes.
Pain in the neck and jaw when swallowing
The cause of pain in the neck and lower jaw when swallowing is sore throat. The disease is diagnosed by symptoms such as fever, headaches, weakness and malaise. The pain may radiate into the ear.
We have listed only the main types of pain. You can accurately determine the root cause of the disease by visiting the following doctors:
- therapist;
- dentist;
- otolaryngologist;
- neurologist;
- surgeon.
Causes
Along with changes in the size and shape of the styloid process, the cause of Eagle syndrome may be:
- ossification of the stylohyoid ligament;
- spasm of the stylopharyngeus, styloglossus or stylohyoid muscles;
- fusion of the stylohyoid ligament with the hyoid bone or with the styloid process.
Symptoms of stylohyoid syndrome
The main symptom of this disease is the presence of constant pain in the upper anterior part of the neck, which intensifies with swallowing, tongue movements, turning the head, and prolonged conversation.
Often pain radiates to the ear, pharynx, temple, temporomandibular joint, sternocleidomastoid muscle, supraclavicular fossa.
Symptoms associated with compression of the carotid arteries are also characteristic:
- noise in ears;
- headache;
- nausea;
- dizziness;
- sensation of a foreign body in the throat.
Diagnostics
To make a diagnosis, it is very important to carefully collect complaints and medical history. So, it is necessary to establish when the painful sensations appeared, what nature they are, what provokes an increase in pain, and what causes a weakening.
It is necessary to accurately determine the areas where pain occurs and where it radiates.
This is important for differential diagnosis with neuralgia of other nerves (occipital, glossopharyngeal, upper laryngeal, trigeminal, auriculotemporal).
It is mandatory to examine the throat to rule out pharyngitis and tonsillitis.
An additional examination method is skull radiography (or targeted radiography of the stylohyoid process).
Why do the lymph nodes under the jaw become inflamed?
In the vast majority of patients, the cause of inflammation of the lymph nodes is a bacterial infection. Most often it comes from an inflamed upper respiratory tract or ear.
According to doctors, in about a fifth of all patients, the lymph nodes in the neck hurt due to advanced caries or a dental abscess.
This inflammation is called lymphadenitis. In the initial stages, this disease develops gradually. There are practically no symptoms. The patient cannot even feel the lymph nodes under the skin. The mucous membranes of the mouth are not hyperemic. The mouth opens without any problems.
Source: https://zdorovo.live/nevralgiya/prichiny-simptomy-i-sposoby-lecheniya-shilopodyazychnogo-sindroma-igla-sterlinga.html
Diagnosis of stylohyoid syndrome in Pirogov
At the National Medical and Surgical Center named after N. I. Pirogov, the diagnosis is made by studying the anamnesis in conjunction with studies carried out in the clinic.
The disease is most often detected by the following method: palpation of the cervical spine or the fossa of the tonsillar part of the oral cavity occurs, resulting in pain.
Then the patient receives a referral for fluoroscopy, which confirms the diagnosis. There have been cases when an increase in the size of the stylohyoid process did not have a painful effect on patients. Before the pathology was discovered, they felt quite comfortable.
Osteoarthritis of the temporomandibular joint
It develops slowly and is often asymptomatic even with significant joint damage. Early symptoms include pain and some stiffness in the temporomandibular joint. The stiffness may go away temporarily and then return (usually at the end of the day). When the lower jaw moves, a crunch occurs in the temporomandibular joint. Upon palpation, pain is determined only in the area of the temporomandibular joint. The radiograph often shows erosion of the cortical plate of the head, less often a tubercle or compaction of the cortical plate; sometimes spur formation or deformation of the head of the mandible is detected. These symptoms are absent in SBD.
Diseases of the salivary glands
Acute purulent inflammatory processes, exacerbations of chronic inflammatory processes, salivary stone disease and malignant neoplasms of the salivary glands are usually accompanied by facial pain.
Acute purulent or chronic inflammatory process most often affects the parotid gland. The nature of the pain that occurs during the initial period of development of purulent parotitis sometimes resembles the temporomandibular joint. However, acute purulent parotitis is accompanied by swelling of the soft tissues over the parotid gland, increased body temperature, hyperemia, swelling at the mouth of the parotid (Stenon) duct and the release of cloudy or purulent saliva from it. Chronic mumps is characterized by long-term treatment and periodic exacerbation of the process with the appearance of signs of acute mumps. These symptoms are not observed in SBD. With salivary stone disease, pain often appears during eating, along with swelling of the affected gland. Sometimes it spreads to the ear and temple. Some time after eating, the pain stops and the swelling subsides. This pattern can be repeated many times.
X-rays and bimanual palpation reveal foreign bodies of various sizes and shapes (salivary stones) located in the excretory ducts or salivary glands. Often an inflammatory process is associated with salivary stone disease. In these cases, a clinical picture of an acute purulent inflammatory process of the salivary gland appears (submaxillitis or mumps). Exacerbation of chronic, often parenchymal, mumps is accompanied by pain in the affected gland. From the anamnesis it is possible to find out that pain and swelling appeared repeatedly. Upon palpation, an enlarged, painful salivary gland is determined. When massaging the gland, cloudy or purulent saliva is released from the mouth of its duct. With artificial contrast (excretion of iodolipol or other radiopaque substance into the excretory duct), the x-ray reveals many small cavities in the thickness of the gland. These symptoms do not occur in SBD.
When the parotid salivary gland is affected by malignant neoplasms (cystadenoid carcinoma (cylindroma), epidermoid carcinoma, etc.), pain often occurs, which gradually increases as the tumor enlarges. An ever-increasing swelling is found in the thickness of the gland. Paresis or paralysis of facial muscles appears. Sometimes saliva mixed with blood is released from the excretory duct. With artificial contrast and on an x-ray, the pattern of the excretory ducts resembles a picture of a dried tree. The nature of the neoplasm is determined using a puncture or biopsy. The listed symptoms are absent in SBD.
Diseases of the paranasal sinuses
More often than others, inflammatory processes and neoplasms are observed in the maxillary sinus. Inflammatory processes of the maxillary sinus are characterized by pain in the infraorbital region, pain upon percussion of the upper molars and premolars, and sometimes the pain spreads to the temporal region. Often upon palpation there is pain in the area of the tubercle of the upper jaw. Anterior rhinoscopy reveals swelling and hyperemia of the mucous membrane, purulent exudate under the middle concha, and sometimes polyps. The x-ray shows darkening of the maxillary sinus. These signs are not present in SBD of the temporomandibular joint. Neoplasms of the maxillary sinus are characterized by pain in the infraorbital region, numbness of half the upper lip, the wing of the nose, sometimes exophthalmos, diplopia, swelling and anosmia on the affected side, tooth mobility and other symptoms that are absent in SBD of the temporomandibular joint. The radiograph shows darkening of the maxillary sinus and destruction of its bone walls with unclear and uneven contours along the periphery.
Diseases of the temporomandibular joint often have to be differentiated from neoplasms of the floor of the mouth, base of the tongue, branches of the mandible or joint. To exclude these diseases, careful palpation of the affected areas, regional lymph nodes, radiography of the lower jaw and function or biopsy of the altered tissue area should be performed. Detection of tissue compaction, bone destruction, atypical cells and other signs not typical for temporomandibular joint dysplasia will help establish the correct diagnosis.