Discoloration of gums is a fairly common problem with which patients often seek help from a dentist. The seriousness of this disease lies in the fact that the blue color of the gums can indicate not only some dental disease, but also the presence of severe somatic pathologies. Diagnosing the disease at an early stage and promptly starting treatment is the key to quickly getting rid of the disease without developing any complications.
Gum structure
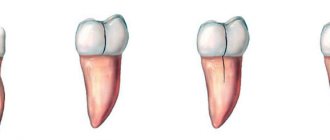
According to physiological and clinical characteristics, the gums are divided into three zones:
- marginal, which covers the cervical area of the tooth and has a smooth surface. The width of this part is 0.8–2.5 mm;
- attached (alveolar). It is fused with the alveolar bone, has a width of 1–9 mm and is lined with stratified keratinizing epithelium;
- free (marginal), located between the teeth and called “interdental papillae,” which normally have a triangular shape. The area adjacent to the tooth is covered with non-keratinizing epithelium.
The basis of the connective tissue of the gums is made up of cells, proteoglycans, fibers and blood vessels. Collagen fibers ensure tight compression of the gums to the tooth, continuity of the dentition and distribution of the load of chewing pressure. The presence of elastic fibers is observed in the perivascular zones.
Histological structure
In accordance with the histological characteristics, two components are distinguished in the structure of the gums. These include stratified epithelium and connective tissue.
In the case of epithelium, the basis of the basal layer are cells in the shape of a cube or cylinder, on top of which are sequentially located spiny cells, protein grains (keratohyalin), as well as the outer stratum corneum. The structure of the latter consists of flat cellular elements that do not contain nuclei and are subject to keratinization, which leads to its periodic renewal - due to deeper layers.
The absence of nerve endings or blood vessels in the epithelium is determined by the functional task of the layer. The goal is to prevent pathogenic bacteria and microbes from entering the periodontal tissue. In this case, there is a natural barrier between the basal layer and the connective tissue base, which forms in the form of a membrane septum.
The gum's own plate is two-layered:
- The upper layer is structurally a connective tissue with a loose structure, forming papillae oriented towards the surface and extending into the epithelium. The sensitivity of the gums is caused by the passage of blood vessels, nerve endings, and the central or trigeminal nerve through them.
- The deeper layer is characterized by a mesh structure and is formed from collagen fibers produced by fibroblasts. Uniting with each other, they move into the periosteum area, due to which the gums remain immobile, and the elements of the dentition are arranged in strict sequence.
The connective substance that unites and strengthens connective tissue cells is the matrix, a product of proteoglycan and glycoprotein molecules. The supply of blood is ensured by the gum branches - the location of the capillaries close to the edge of the tissue causes increased sensitivity of these areas.
Consequences of a recession: what will happen if the problem is not solved
Almost all dental diseases, if ignored for a long time, first result in a loss of aesthetics, food getting into the spaces between the teeth, the development of an inflammatory process, mobility, and then the loss of teeth. And gum recession is no exception. As the thinning and loss of mucous membranes progress, the problems intensify:
- increased sensitivity and acute pain in the teeth in the area of the gingival margin develops,
- exposed areas of the root are more susceptible to caries, which quickly reaches the inside of the tooth and affects the pulp,
- the risk of developing wedge-shaped defects increases,
- gums become swollen and inflamed or, on the contrary, become unnaturally light, whitish,
- Plaque is deposited faster at the roots, which over time expands the periodontal pockets and, among other troubles, gives a putrid odor from the mouth.
If the problem is not solved, you can lose all your teeth - they simply will have nothing to hold on to.
Also, the recession has psycho-emotional consequences. When the gum contour loses its attractiveness, a person's smile begins to appear unhealthy and completely unattractive. In addition, the teeth lengthen because... their roots are now also “included” in the smile zone. Large gaps (tremas) appear because the roots of the teeth are narrower. All this creates serious psychological barriers to communication.
Symptoms
In addition to visual changes in soft tissue, the following symptoms may occur:
- pain when eating and brushing teeth;
- itching;
- swelling of the mucous membrane;
- the appearance of bleeding;
- abundant plaque on the teeth and the appearance of mineralized deposits.
Symptoms depend on the cause of the pathology and on the individual characteristics of the patient’s body. Eliminating cyanosis of soft tissues is the first step in treatment and in making the patient feel better.
When to seek help from a specialist
- The blue color of the gums does not subside for more than four to five days;
- Blue discoloration is accompanied by swelling and bleeding;
- Acute pain appears that is not relieved by painkillers;
- Body temperature can rise to 38 - 39 degrees;
- Loss of strength, general weakness.
Ignoring the disease is fraught with the development of serious complications, including the formation of an intraoral cyst.
Recommendations after tooth extraction
There are recommendations that, if followed, significantly speed up the gum healing process. Not only the speed of wound healing depends on them, but also the absence of possible complications. The doctor’s main recommendations in the postoperative period may be the following:
- you need to avoid foods that are too hot, spicy, or irritating to gum tissue;
- in the first days you need to carefully avoid damaging the clot; It is necessary to be extremely careful in maintaining oral hygiene;
- about 3 hours after the tooth extraction procedure you need to refrain from eating;
- in the next three days you need to eat only soft food, without consuming sweets, alcohol, or hot drinks;
- on the first day after the procedure, it is recommended to sleep on a high pillow;
- During the week, it is recommended to avoid visiting the sauna, solarium, sunbathing on the beach, and reduce physical activity;
- on the first day, it is forbidden to brush your teeth to avoid damaging the blood clot;
- Do not try to pick the clot with your finger, toothpick or tongue;
- a cold compress should be applied to the surgical area for 20 minutes, every 2 hours;
- It is recommended to use oral baths and then rinse with antiseptic agents.
The postoperative period requires careful attention to the patient's health status. A complication resulting from neglect of the rules will require much more time, money and effort to heal the wound.
Pathologies
Factors that can trigger gum disease include mechanical damage, poor hygiene, infection, and the development of ulcers or cancer. Characteristic signs of deviation from the norm are loss of sensitivity, the formation of edema, bleeding and abundant accumulation of plaque on the surface. Common diseases include:
- Gingivitis is an inflammatory process that occurs as a result of chronic pathologies, errors in the selection of prosthetic structures, as well as tartar deposits.
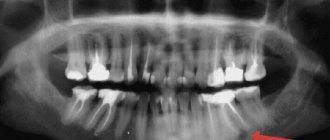
- Periodontitis is an inflammation of bone tissue, often developing from a local to an extended form. It becomes the result of infection or food debris getting into the gum pockets, and, in the absence of proper treatment, leads to a weakening of the structure of the dentition.
At the first signs of abnormalities, it is recommended to undergo diagnostics at a dental clinic. Timely identification of the cause of gum disease allows comprehensive treatment to begin and helps to avoid serious consequences.
Periodontal structure
Author: Joseph P. Fiorellini
There are three zones in the oral mucosa:
1. Gums and hard palate, covered with chewing mucous membrane.
2. The back of the tongue, covered with a specialized mucous membrane.
3. The mucous membrane lining the rest of the oral cavity. The gum is a part of the oral mucosa that covers the alveolar processes of the jaws and surrounds the necks of the teeth.
Clinical features
Normally, in adults, the gingiva covers the alveolar bone and root down to the cemento-enamel junction. The gum is anatomically divided into marginal, attached and interdental. Although each gingival type has significant differences in differentiation, histology, and thickness depending on their functional purpose, all types are designed to prevent mechanical and microbial damage. That is, the specific structure of different types of gums reflects its effectiveness as a barrier to the penetration of microorganisms and toxic substances into deep-lying tissues.
Marginal gingiva
Marginal, or unattached, gingiva is the edge or border of the gum that surrounds the teeth in a collar-like manner (Figures 2-1 and 2-2). In approximately 50% of cases, it is separated from the adjacent attached gum by a shallow linear depression called the free gingival groove. Typically about 1 mm wide, the marginal gingiva forms the wall of the gingival sulcus. It can be separated from the tooth surface with a periodontal probe.
Gingival sulcus
The gingival sulcus is a shallow crevice or space around a tooth, bounded by the surface of the tooth on one side and the epithelium lining the free edge of the gum on the other side. It is V-shaped and barely allows the insertion of a periodontal probe. Clinical determination of the depth of the gingival sulcus is an important diagnostic indicator. Under absolutely normal or ideal conditions, the depth of the gingival sulcus is 0 mm or close to this value. This can be achieved experimentally only in animals completely devoid of microorganisms, or after intensive long-term prevention of plaque formation.
Clinically healthy gums have a groove of some depth. Its depth, determined on histological sections, is 1.8 mm, with a variation from 0 to 6 mm; other studies reported 1.5 mm and 0.69 mm. The clinical assessment used to determine sulcus depth is performed by inserting a metal instrument called a periodontal probe and determining the distance it penetrates. Histologically, the depth of the sulcus does not have to be exactly equal to the depth of penetration of the probe. The so-called probing depth of clinically normal gums in humans ranges from 2 to 3 mm.
Figure 2-1 Normal gingiva in a young adult. Note the demarcation (mucogingival line) (arrows) between the attached gingiva and the darker alveolar mucosa.
Figure 2-2 Diagram of the anatomical formations of the gums.
Attached gum
The attached gingiva is a continuation of the marginal gingiva. It is hard, elastic and tightly connected to the underlying periosteum of the alveolar bone. On the vestibular side, the attached gum extends to relatively loose and mobile alveoli