Symptoms of periodontitis (photo), treatment and prevention
Periodontitis is a dental disease, inflammation of the gums. The term periodontium is used to collectively refer to the tissues that surround a tooth and hold it in the jaw. These are ligamentous fibers, connections between the mucosal surface and the crown, gingival cement and gingival bone.
The causes of periodontitis lie in infection of the gums through dental tissue (caries, plaque), dental pockets (gingivitis) or from internal sources of infection (internal inflammatory diseases). Let's look at the symptoms and signs of periodontitis, methods of its treatment and prevention.
Periodontitis and periodontal disease - what is the difference?
Often patients consider these two concepts to be the same dental disease, but this is not entirely true. With periodontitis, there is always an active inflammatory reaction, bleeding and swelling of the gums, periodontal pockets of varying depths and tooth mobility. With periodontal disease, the gums are dense, anemic, there are no pockets or tooth mobility, but the necks and roots are significantly exposed, as a result of which wedge-shaped defects often appear in these areas.
Splinting procedure for periodontitis
The need for splinting in the treatment of periodontitis arises when there is mobility of more than 2-3 dental units in a row. Splinting helps strengthen teeth and also helps to quickly eliminate inflammatory processes in soft tissues.
Splinting can be carried out in different ways. A specialist can use fiberglass tapes in manipulations, install welded dental crowns or a clasp denture. The method of splinting is selected based on the clinical picture of a particular case.
Why does periodontitis develop?
Chronic localized periodontitis can appear for several reasons:
- The presence of carious cavities on the proximal side of the tooth.
- Inadequate prosthetics, after which wide crowns, incorrectly manufactured removable or bridge dentures injure the gums.
- Trauma to the gums as a result of physical impact (bruise) or malocclusion (creation of so-called supraocclusion). If the teeth do not close evenly and there is an area where biting occurs first (super contact), due to the increased load, periodontal inflammation develops in this area. The cause of supercontact may be a filling that overestimates the bite or the absence of part of the teeth.
- Unprofessional dental treatment, as a result of which fillings were installed that do not correspond to the anatomical shape of the tooth, as a result of which overhanging edges injure the edge of the gums and cause food retention in the spaces between the teeth, which leads to the development of the inflammatory process.
The causes and factors that provoke the development of a generalized inflammatory process in the periodontium are as follows:
- Impaired functioning of the immune system, leading to a decrease in the general and local protective response of the body;
- Poor oral hygiene, leading to the accumulation and activation of pathogenic microorganisms;
- Violation of the rate of metabolic processes in the periodontium;
- Reduced load on the dentogingival apparatus due to eating predominantly soft foods;
- Abnormal bite or incorrect location of individual teeth in a row (shifts and rotations along the axis);
- The presence of certain diseases (atherosclerosis, diabetes, gastrointestinal diseases);
- Exposure to occupational (chemicals) or environmental (increased background radiation) harmful effects, constant stress;
- Bad habits, unbalanced diet, excessive use of certain drugs;
- Pregnancy period (the first place at this time is the change in hormonal levels);
- Hereditary predisposition.
Acute periodontitis develops mainly after injuries - chemical (the effect of various substances on periodontal tissue), physical (thermal burns), extensive mechanical damage. This form of the disease can also develop as a complication of acute necrotizing ulcerative gingivitis.
What are the causes of periodontitis?
Understanding the causes of the disease is a very important point, which helps the doctor correctly determine how to treat gum periodontitis. The disease can be triggered by both general and local factors. Common causes include diseases of the gastrointestinal tract, diseases associated with pathology of the endocrine system, some gynecological and urological diseases, sexually transmitted infections, and a weakened immune system. Local, or local, factors are missing teeth, malocclusion, incorrectly installed fillings or crowns, which mechanically irritate the gums and create conditions for the accumulation of bacterial plaque. A significant role is played by the specific microbial flora of the oral cavity, which occurs in some patients and causes periodontitis. But the main factor in the development of periodontitis is poor oral hygiene.
Symptoms
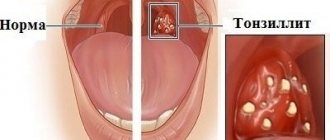
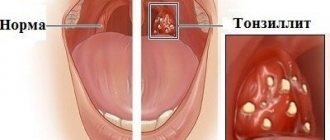
Periodontitis (see photo) is manifested by the progressive destruction of the alveolar processes (namely, the dental cells of these processes). The symptoms of the initial stages are scanty - bleeding gums, loose teeth, sometimes viscous saliva, plaque on the teeth. When the disease is active, due to the rapid destruction of the alveolar processes, the teeth gradually fall out.
The clinical manifestations of exacerbation of periodontitis are more varied: inflammation of the gums, purulent discharge from the periodontal pockets, bad breath, pathological mobility of teeth, and their displacement. Abscesses and fistulas on the gums, enlargement and soreness of the submandibular lymph nodes are common. A chronic course with frequent exacerbations of periodontitis may be accompanied by microbial allergies.
First you need to understand what “periodontal” is and what part of the oral cavity we are talking about.
In fact, the teeth are not permanently attached to the jaw, i.e. they are attached to the bone using various soft tissues and ligaments. These include: the gums, the jaw bone itself (the bony alveolus or “socket”) and the periodontal ligament of the tooth.
If you depict it in the figure, it will look like this (in this question, the elements highlighted in red are important to us):
Now let's move on to the issue of defining periodontal disease itself.
Periodontal disease is a disease in which intensive loss of bone tissue, gums and tooth ligaments occurs.
It is very important to distinguish “Periodontal disease” from “Periodontitis”; what is the difference?
Periodontitis is an inflammatory disease of the tissues surrounding the tooth. It most often occurs as a result of poor oral hygiene. Symptoms of this disease include bleeding, swelling and pain in the gums, and tooth mobility.
Periodontal disease is a non-inflammatory disease, which means there will be no redness, bleeding or pain in the gums.
The occurrence of periodontal disease is interpreted in different ways. They are divided into systemic (i.e., arising indirectly from diseases) and local (arising due to factors acting directly on the periodontium).
The most common common causes of periodontal disease:
- Atherosclerosis (narrowing of the lumen of blood vessels due to deposition of lipid granules in the walls)
- Disruption of the endocrine glands (such as thyroid, pancreas, hypothyroidism)
- Gastrointestinal dysfunction (eg, gastritis, ulcers)
- Changes in the body's reactivity, i.e. appearance of allergies
The cause of periodontal disease and its development
Periodontal disease is a complex disease and has many causes.
The most basic reason is sclerosis (narrowing of the lumen) of blood vessels. Next, tissue trophism begins to be disrupted, i.e. there is insufficient blood supply, delivery of oxygen, nutrients and then a decrease in the number of tissues.
As a result, due to insufficient tissue nutrition, gradual resorption of bone tissue occurs, a decrease in the amount of gums, and exposure of the roots.
Factors that can lead to the development of periodontal disease include:
- Elderly age
- Cardiovascular diseases
- Diabetes
- Nervous system diseases
How to carry out early diagnosis of periodontal disease. Observation of which specialists is important for this disease. Who is at risk?
Periodontal disease is a rather difficult disease to diagnose.
But, as a rule, people experience the following symptoms:
- Reduced gums and decreased bone tissue (the most important symptom!)
- Increased sensitivity of the necks of the teeth
- No gum inflammation
- No periodontal pockets
- Stable position of the tooth in the socket, even with severe gum recession
- Diseases of various body systems that indirectly indicate periodontal disease
Observation by a dentist, i.e. preventive examination once every 6 months. Then you will be referred to a highly specialized doctor - a periodontist. Also, in a regular city clinic, observation by a regular local physician is necessary so as not to miss the onset of any systemic disease.
The main risk group for development is older people. Also people exposed to constant stress, overwork, smokers, etc.
How to identify the cause and what examination methods exist.
There are quite a lot of examination methods.
- Methods for assessing the condition of bone tissue
- The X-ray method of examining teeth with periodontal disease is the most common and simplest. This method makes it possible to assess the degree of bone tissue loss and its quantity. The most common and accessible methods are: intraoral contact radiography, orthopantomogram (OPTG). The disadvantage of this method is the limited field of study.
- An orthopantomogram (OPTG) allows you to assess the condition of the alveolar processes of both jaws in one image. The disadvantage of this method is distortion in the area of the front teeth.
- Computed tomography (CT) is the most preferred research method. Thanks to it, you can build a 3D model of the human dental system. When using CT, there is practically no distortion, unlike OPTG.
- Method for assessing tooth mobility
- Palpation (without the help of special instruments)
- Periodontogram (done using a special apparatus, and then a table is filled in where the periodontal strength of various teeth is determined)
This symptom is important in periodontal disease, but can also occur in other periodontal diseases. The essence of this method is thermal diagnostics (using hot or cold water, i.e. irrigating the tooth from a syringe or by applying a cotton ball to it).
In clinical practice, there are three degrees of hyperesthesia:
- The first is that tooth tissues react to temperature stimuli (a person feels hot or cold water, but does not experience discomfort)
- Second - a person feels pain from the irritant
- Third – pain from any irritants or even without them
Removal of supra- and subgingival dental plaque. Oral hygiene
Removing supra- and subgingival plaque is essential to maintaining both periodontal and overall oral health. This is the main goal of professional oral hygiene. Tartar does not play a significant role directly in the development of periodontal disease, but indirectly it can aggravate the situation with periodontitis (see above the differences between periodontal disease and periodontitis).
There are two ways to remove hard plaque: manual and hardware.
The manual method involves the use of various hand tools to remove tartar.
These tools are different and perform different functions, respectively: scalers, curettes, excavators, smoothers, chisels, rasps.
The hardware method is more common and involves the use of a special device. These piezoelectric devices have a frequency from 25 to 45 kHz. Using these frequencies, the tip attachment breaks the contacts between the molecules of the tartar and allows you to simply wash it off with water or clean it with a special brush and paste.
Main representatives: scalers from EMS (Switzerland), Amdent Boitrol (Sweden), Satelec (France), Siroson L (SIRONA).
After treating the teeth with an ultrasonic scaler, sandblasting is carried out (if there is dark plaque) if necessary, and mechanical cleaning of the teeth with a brush and paste to remove remaining dental deposits, for example, Detartrine. Further, after such an aggressive effect on its structure, it is necessary to restore the mineral composition. To achieve this, fluoridation is carried out in various ways: varnishes, gels, etc.
After professional oral hygiene, it is necessary to replace the old toothbrush with a new one. This is necessary because an old toothbrush contains many microorganisms that can lead to an exacerbation of the same diseases that existed.
During and after treatment, oral hygiene is required 2 times a day and replacing the toothbrush once every two months.
The optimal set of dental products for periodontal disease:
- EZSH (electric prophylactic toothbrush) – if a person has the opportunity to use an EZShch, then this is better than having a manual one. An electric toothbrush should be characterized by: a round head, two-level bristles, indicating bristles (degree of wear), a timer.
- Manual protective shield (if it is impossible to purchase an electrical protection shield) – medium degree of hardness, multi-level bristles, rounded bristle tips, microtextured polymer coating, indication of the degree of wear of the bristles, rubber-plastic in the handle, comfortable grip, non-traumatic. If hyperesthesia occurs, it is possible to replace the brush from medium-hard bristles to soft ones.
- Therapeutic and prophylactic toothpaste - should contain anti-inflammatory oils and plant herbs, it is possible to introduce fluoride compounds to prevent carious lesions, should not contain strong antiseptics, and should contain a moderate abrasive. Also, if hyperesthesia occurs, it is recommended to switch to a “Sensitive” type paste.
- Therapeutic and prophylactic mouth rinses - an anti-inflammatory component in the form of extracts of herbs and plants, without strong antiseptics, with sweeteners is also possible. Regular use is required.
- Flosses (dental floss) are two-component, regular use after each meal is mandatory.
- Irrigator – if you have the opportunity to use an irrigator, then this is very good. There are 2 modes: shower and jet.
Irrigator
Treatment algorithm for periodontal disease
First, it’s worth making a reservation: is it possible to cure periodontal disease? In the early stages of the process - yes, later we are talking about stabilizing the process and stopping further bone resorption. This is done to preserve the teeth for as long as possible.
Treatment for periodontal disease includes several stages:
- Consultation with a periodontist - this doctor specializes in such problems, so he will review images and other research methods and then come up with a plan for further treatment.
- Professional oral hygiene with removal of supra- and subgingival dental plaque. I wrote above about the need for this procedure.
- Anti-inflammatory therapy - includes local and general.
- With local anti-inflammatory therapy, drugs are applied directly to the gum and have a local effect through the capillaries of the gum. Typically this treatment includes the following drugs:
- Rinse with Chlorhexidine 0.05% immediately after brushing your teeth (in the first minute)
- Applications with “Cholisal” or “Solcoseryl” gels. It is carried out after applying chlorhexidine and drying the gums.
- Closed curettage: the purpose of this method is to completely clean out periodontal pockets of possible microorganisms that cause infection. This method is used for mild periodontal disease. It is carried out using special curettes, which, under infiltration anesthesia, are introduced into the periodontal pocket and all dental plaque is removed there manually. The regime after surgery is important: do not eat for the first 2 hours after surgery, then for several days use only crushed, non-hot food and perform hygiene only with liquid products. It is better not to use a toothbrush for the first 2–3 days.
- Open curettage: performed for moderate to severe periodontal disease (depth of periodontal pockets more than 5 mm). Methodology: under infiltration anesthesia, the gum is dissected and detached. This access allows you to completely open the periodontal pocket and clean the tooth root from dental deposits. Then treatment with antiseptic drugs and application of drugs that stimulate osteogenesis (bone growth) are carried out.
- Transplantation of the soft tissue component. This operation is used when the tooth root is exposed. A patch taken from the palate is sutured onto the affected area.
- Gingivectomy is the removal of affected, inflamed, hardened gums by excision.
- Tooth extraction is a radical method, but it is necessary in cases of severe mobility, bleeding and the impossibility of restoring tooth function.
Non-traditional methods of treating periodontal disease
As an independent treatment, this type of treatment will be ineffective, because... Doctors' intervention is necessary to adequately assess the condition of the oral cavity.
And only with the permission of a doctor can unconventional methods be approved.
For example, herbal poisons that have a local anti-inflammatory effect.
Is implantation possible for periodontal disease?
Yes, this method of treatment is possible, but do not forget that no one will give you implants right away.
First, you need to undergo long-term treatment with bone restoration and only then should you talk about implantation.
{jlcommentspro}
Stages of the disease
In dentistry, there are three stages of periodontitis:
- Grade 1 is a small depth of periodontal pockets (up to 3 mm), the appearance of periodic bleeding of the gums after cleaning. At this stage there is no pain or tooth mobility.
- 2nd degree - the pockets deepen up to 5 mm, the neck of the tooth is partially exposed, and a feeling of discomfort appears when in contact with cold and hot.
- Stage 3 is formed 4-5 years after the onset of inflammation (with the usual non-aggressive course of the disease). With severe gum damage, the pockets deepen beyond 6 mm, usually accompanied by the accumulation of food debris and the formation of pus. Pus comes out from under the tooth when you press on the gum. The teeth themselves become very loose and exposed.
Classification of the degree of tooth mobility:
- 1st degree. It is characterized by the possibility of tooth displacement by no more than one millimeter in the vestibulo-oral, bucco-lingual directions and to the adjacent tooth;
- 2nd degree – pathological mobility in the same directions by more than a millimeter, and the appearance of mobility in the palatal-distal direction;
- 3rd degree – teeth are mobile in all directions, including vertical. If some neighboring teeth are missing, then tilting is possible;
- 4th degree – the tooth is mobile in all directions, easily makes any forced movements, including around its axis.
In addition, there are several more varieties of the course of the disease. If gum inflammation develops very quickly, deep pockets up to 8-10 mm deep are formed in one to two months, then this is aggressive periodontitis. If the disease affects several teeth, then it is local periodontitis.
Prosthetics for periodontitis
Prosthetics for periodontitis are necessary in cases where a person has no dental units in his rows. Carrying out prosthetics allows you to prevent the displacement of teeth in rows and completely restore the correct chewing load in the oral cavity. Prosthetics is the final stage in the conservative treatment of periodontitis and must be carried out before surgery (if the operation is planned in the general treatment plan).
For prosthetics in the treatment of periodontitis, it is extremely important to choose the right prosthesis. It must be of high quality and modern, otherwise it will not be possible to stop the process of bone atrophy.
Diagnostics
If any symptoms of periodontitis are detected, it is important to promptly consult a dentist and undergo a thorough examination, during which a specialist will be able to make the correct diagnosis or prescribe additional tests to differentiate the disease.
During the examination, the dentist will perform probing, which will help determine the depth of the gap between the gum and tooth. Based on the results of the examination, it will be possible to determine the degree of periodontitis.
Additional studies are prescribed:
- benzidine test (helps determine the presence of pus in the periodontal pocket);
- Schiller-Pisarev test (helps to see the inflammatory process in the gums at an early stage due to staining);
- radiography (to visualize the degree of bone tissue destruction);
- a smear from a periodontal pocket (determines causative bacteria);
- panoramic tomography (a full view of the affected jaw, mainly prescribed for suspected generalized periodontitis).
In cases where periodontitis is accompanied by general diseases, other tests may be prescribed to help determine the diagnosis and prescribe appropriate treatment.
Periodontal diseases. What gum diseases are there?
Notice
: Undefined variable: post_id in
/home/c/ch75405/public_html/wp-content/themes/UltraSmile/single-item.php
on line
45 Notice
: Undefined variable: full in
/home/c/ch75405/public_html/wp-content /themes/UltraSmile/single-item.php
on line
46
Rate this article:
( 2 ratings, average: 3.00 out of 5)
gum disease
1 Beloklitskaya G.F. Clinical forms of generalized periodontitis and their significance for its differentiated therapy.
How to treat periodontitis?
Effective treatment of this disease will largely depend on how far the inflammatory process has progressed. The more significant the level of bone loss around the teeth, the degree of tooth mobility, the more teeth were lost - the more difficult, longer and more expensive the treatment will be.
The first thing to do is make a treatment plan. This is not as easy to do as it might seem in reality. If the disease is mild, you may only need to consult a periodontist. In cases where the disease is severe, there are malocclusions, there are missing teeth or teeth that need to be removed during treatment, a joint consultation with a periodontist, an orthopedist (prosthetist) and a general dentist is necessary. Remember that it is necessary to plan prosthetics and dental treatment before the actual periodontal treatment begins.
The next stage is direct work with the gums, or rather deposits on the gums. As is known, a significant percentage of periodontitis depends on non-compliance with oral hygiene, namely incomplete cleaning of the area where the gums adhere to the tooth. As a result of this, dental plaque and subsequently tartar are formed, which contribute to the separation of the gums from the tooth itself.
Until dental plaque is removed, no treatment method will bring the expected result, and time will be wasted. Therefore, at the second stage, dentists begin to cleanse the oral cavity of plaque and tartar. This procedure is best carried out using the ultrasound method.
Periodontitis: what is this disease?
Before moving on to considering treatment methods for periodontitis, it is worth finding out what kind of dental disease it is and why it appears. In dentistry, periodontal tissue is the tissue that tightly surrounds the roots of the teeth and holds the tooth itself in its socket. When an infection penetrates into the periodontium, an inflammatory process begins in the tissue, which leads to the occurrence of periodontitis. Treatment of periodontitis should be started immediately, however, the disease cannot always be recognized in a timely manner and independently, since it can develop completely asymptomatically. It is for this reason that it is recommended to undergo regular examinations by a dentist: a specialist will determine the signs of periodontitis and treatment of the disease will be as effective as possible.
Calculate the cost of treatment by taking a short test in 20 seconds!
Do not delay your treatment, because in this matter time plays against us.
The main cause of periodontitis is pathogenic microorganisms that penetrate into the deep layers of the periodontium, however, there are factors that contribute to the appearance of the disease and accelerate the process of its development. These factors include:
- Untreated or advanced gingivitis;
- Autoimmune diseases (diabetes mellitus, HIV);
- Bite defects;
- Increased tone of the jaw muscles;
- Injuries to soft tissues of the oral cavity;
- Poorly performed dental procedures: prosthetics, fillings;
- Stressful and depressive conditions, the presence of bad habits;
- Poor or irregular oral and dental hygiene;
- Some gastrointestinal pathologies.
The listed factors will complicate the treatment of periodontitis, and therefore it is recommended to eliminate them before starting a course of therapy, which means that for effective treatment of periodontitis you will need to visit not only the dentist, but also specialists in other areas of medicine.
Drug treatment
Drug treatment of periodontitis can be divided into local and general:
- General therapy. A combination of antibiotics is prescribed. Moreover, depending on the severity of inflammation and the presence of concomitant diseases, antibiotics can be prescribed both in tablets and intramuscular injections (which, by the way, is preferable). Treatment of periodontitis with antibiotics is also carried out for 10 days, no less.
- Local therapy (in the oral cavity). It includes antiseptic mouth rinses, rinsing periodontal pockets from a syringe with antiseptic solutions, and applications of antimicrobial anti-inflammatory gels. The duration of local anti-inflammatory therapy is 10 days, treatment is carried out twice a day (morning and evening). Moreover, depending on the severity of the disease, the periodontist may prescribe rinses and applications for home use, or you will need to come to the dental clinic at least once a day. In this case, the doctor will rinse the periodontal pockets with antiseptic solutions from a syringe and also treat the gums with gel. The patient will have to do the second treatment independently at home.
- Physiotherapy. Local therapy may also include physical therapy. For example, laser treatment of periodontitis has recently been advertised. But you need to understand that treatment of periodontitis with laser or electrophoresis is only an auxiliary physiotherapeutic method that allows you to relieve the symptoms of inflammation only a little faster.
- Toothpastes. Special anti-inflammatory toothpastes can be an additional tool in complex treatment. There are very good pastes that will help quickly relieve inflammation and strengthen the gums.
In parallel with the removal of dental plaque and anti-inflammatory therapy, it is necessary to begin treatment of carious teeth and removal of non-viable teeth. If at the stage of drawing up a treatment plan the need for prosthetics with bridges or removable dentures was determined, then at this stage the teeth can be prepared for prosthetics, for example, tooth depulpation.
How is periodontitis treated?
Successful treatment of periodontitis can only be achieved in a well-coordinated team of “doctor plus patient”. Much depends on the doctor, but even more depends on the patient himself. The doctor is responsible for the treatment, and the patient is responsible for maintaining the result, because periodontitis is a chronic disease.
Treatment methods for periodontitis are divided into medicinal and surgical. In case of minor inflammation caused by dental plaque, the doctor thoroughly cleans the teeth, eliminates conditions that contribute to the retention of microbial plaque, polishes the surfaces of the teeth and applies a therapeutic bandage with medication to the inflamed area. If a deep periodontal pocket forms and severe pain occurs, the patient may be prescribed antibiotics. When treating severe periodontitis, it is necessary to resort to more serious (surgical) procedures, such as curettage and flap operations. But in any case, periodontitis requires complex treatment, including professional hygiene, drugs for local and internal use, and, if necessary, surgical procedures.
There is also a hardware method for treating periodontitis - Vector. The method involves using ultrasound in combination with medications aimed at fighting microbes and stimulating healing. The Vector device is used both as an independent technique and in combination with surgical treatment.
Treatment of periodontitis with folk remedies
In some cases, drug treatment is replaced with alternative medicine recipes.
The following recipes can be used at home:
- Fresh plantain juice. It rubs into the gums.
- Oak bark (two tbsp) and linden flowers (one tbsp). Mix, pour a large spoonful of the composition into a glass of boiling water. Cool, after straining, use as a mouth rinse 4-5 times a day.
- Sea buckthorn and fir oils. Equal parts of oils are mixed, a piece of bandage is soaked in the mixture, and the sore spot on the gum is massaged with it for ten minutes twice a day.
- Comfrey roots. One tablespoon of roots (crushed, dry) is poured into a glass of water and boiled over medium heat for 20 minutes. Use the decoction as a rinse twice a day.
- Juices of agave (aloe) or Kalanchoe. Make lotions with juices every 10 days, applying to the sore gum for 35 minutes.
Only after consultation with a doctor is it possible to use “grandmother’s recipes”, since the main principle of treating periodontitis remains the principle of not doing harm and not getting a complicated course of the disease.
Treatment of periodontal disease in the early stages
When periodontal disease has not yet destroyed bone tissue, it is easier to cure teeth and gums. To begin with, ultrasonic cleaning of the oral cavity is carried out, which removes plaque, tartar and deposits.
Afterwards, drug treatment of periodontal disease is prescribed:
- General therapy includes taking hormonal and immunomodulating drugs and antibiotics. The exact selection of medications for periodontal disease is made by a dentist; the treatment method depends on the cause of the disease. This is why doctors do not recommend self-medicating without consultation and resorting to traditional medicine - these ineffective remedies create the illusion of treating teeth and gums while the disease progresses.
- Strengthening the immune system. Drugs that boost immunity actually help the body cope with the destruction of gums, tooth roots and bone tissue faster, but only a doctor can prescribe them, and only after conducting a series of tests that will show what substances the body lacks. Contrary to popular belief, special diets do not help get rid of periodontal disease, but dentists recommend excluding spicy, fatty and fried foods - such foods irritate damaged gum tissue and negatively affect the microflora of the oral cavity. It is recommended to eat more fruits and vegetables, because they strengthen the immune system.
- Local therapy. Injections into the gums for periodontitis, gels, painkillers and disinfectants. The main goal of such treatment is to prevent the return of plaque or inflammation.
Surgery
As soon as the teeth become mobile, the dentist resorts to a treatment method such as splinting. With its help, the load is distributed from mobile teeth to stable ones.
There are three splinting methods:
- In the first case, when splinting, a horizontal bar and fiberglass tape are placed on several teeth, after which everything is filled with a light composite. This bar strengthens mobile teeth, stabilizing the row.
- Crowns are considered a more effective method. To do this, the upper part of the tooth is ground down and the root is filled. Crowns soldered together are placed on top. The material for crowns can be chosen depending on preferences and financial capabilities.
- The most expensive and most effective is the use of a clasp prosthesis. It is placed on the jaw and is additionally secured with a metal crossbar for greater stability.
Gingivectomy:
- Gingivectomy is usually used in the early stages of the disease. The essence of the operation is to clean the pockets and remove the inflamed areas of the gums by making an incision. The wound is treated with a special solution and filled with iodine. As a rule, gingivectomy is prescribed for complex surgery in the area of several teeth. The procedure is often confused with patch surgery.
Gingivoplasty:
- For periodontitis, gingivoplasty may be prescribed. It is necessary not only for aesthetic reasons, but also for cleaning pockets and restoring them. The operation is performed under local anesthesia after pre-treatment with an antiseptic. The dentist cleans the contents of the pockets, removes caries and tartar from the roots, and covers the cement of the tooth with a protective film. The gingival tissue is renewed with epithelium taken from the palatal part. Often, during gingivoplasty, bone tissue is restored or transplanted.
Flap operation:
- It can be carried out in several ways, but its main goal is to cleanse the roots of dangerous plaque and secure the gums in such a way as to hide the roots as much as possible. The surgical intervention takes place under local anesthesia, the dentist makes an incision into the tissue, performs root sanitation and puts the flaps back. Often, areas of the gum damaged by inflammation are removed. The pieces of epithelium are connected with sutures.
Prosthetics are performed for patients with missing teeth in the dentition. This is the final stage of treatment, before which the oral cavity was sanitized and gum inflammation, caries, etc. were eliminated. The purpose of this stage is to restore chewing function and correctly distribute the load on the patient’s healthy teeth, prevent their displacement, and restore the aesthetics of the oral cavity. In order to relieve the burden on the teeth before surgery, it is necessary to resolve the issue of prosthetics - install at least a temporary prosthesis for this period, which is subsequently replaced with a better one. Otherwise, after surgery, tooth mobility will only increase.
Is it true that periodontitis can be cured with implantation?
Implantation is a method of combating not periodontitis itself, but its consequences. At a later stage of the disease, teeth become loose and fall out, so they have to be replaced with implants. It should be understood that dental implantation for periodontitis has its own difficulties and limitations, since bone tissue is absorbed in this disease. Its sufficient volume is the main condition for successful installation of implants. If periodontitis is in an advanced stage, implantation can be very difficult or even impossible due to a lack of bone volume. That is why patients should begin treatment as early as possible in order to do everything possible to preserve their teeth, and if they are lost, do not miss the opportunity to restore them with implants.
In any case, before installing implants, it is necessary to transfer periodontitis to the stage of remission (stabilization) or, if possible, eliminate the cause of its occurrence.
Prevention
To prevent such serious problems with soft tissues, it is best to stick to simple and accessible methods of prevention. Dentists recommend:
- avoid stressful situations;
- eat well and strengthen the immune system;
- do not cause general diseases;
- if even one unit falls out, install prostheses;
- lead a healthy lifestyle and give up bad habits;
- try not to damage soft tissues with sharp objects, avoid traumatic situations;
- treat any diseases in a timely manner and eliminate the first symptoms;
- Brush your teeth daily with a medium-hard brush, in circular motions, for at least five minutes;
- If a malocclusion is detected in childhood, it is better to correct it.
- do not forget about the importance of solid products that stimulate metabolic processes in the gums and naturally cleanse the surface of plaque;
- visit the dental office every six months for a thorough examination and detection of the first signs of any abnormalities, as well as for professional cleaning of plaque and tartar.
In addition to these general tips for maintaining health and maintaining good oral hygiene, you can also periodically massage your gums. To do this, apply light pressure on both sides with clean fingers. It is not difficult, and the whole procedure lasts no longer than 5-10 minutes. As a result, metabolic processes in periodontal tissues will resist the proliferation of bacteria.
How to avoid further exacerbation of the disease?
This is where the patient becomes the main member of a well-coordinated doctor-patient team. To maintain the results obtained after treatment of periodontitis, you should brush your teeth correctly and regularly, following all the recommendations of the treating dentist, since with periodontitis, individual oral hygiene differs from usual. In particular, along with a regular brush and paste, there is a need to connect additional hygiene products: dental floss, various brushes for teeth, an irrigator, etc.
In addition, it is necessary to come to the dentist for professional cleaning at least once every six months, and for people with chronic periodontitis even more often - once every three months. Good hygiene is an excellent prevention of periodontitis and the only way to maintain the results of treatment.