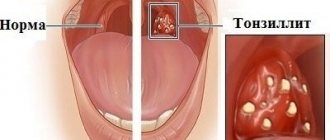
Chronic tonsillitis is a chronic inflammation of the tonsils.
The palatine tonsils (popularly called tonsils) are an important part of the human immune system.
Bacteria, viruses, and microscopic fungi enter us with food and air. They settle on the mucous membranes, where they are picked up by a constant current of mucus, and this “river” flows in the direction of the oropharynx, just where the tonsils are located behind the palatine arches.
The palatine tonsils are like a sponge. They are dotted with gaps. When we swallow a bolus of food soaked in infected mucus, this mucus enters the lacunae of the tonsils. There, foreign microorganisms are attacked by the guard cells of the primary immune response: neutrophils and macrophages. The latter not only kill the infection, but also “cut” it into small molecular fragments, on which young cells of the secondary immune response—lymphocytes—are then “trained.” Prepared and trained lymphocytes emerge from the tonsils and “spread” throughout the mucous membranes of the pharynx and nose, forming a fairly reliable secondary specific defense.
Exacerbation of chronic tonsillitis: symptoms
Often, for a long time, chronic tonsillitis occurs without symptoms or has scanty symptoms (in a simple form). There may be discomfort when swallowing food and liquids, a sensation of a foreign body in the throat, dry mouth, halitosis (bad odor) and tingling. Externally, the tonsils increase in size and there are signs of inflammation. The disease is characterized by exacerbations of sore throats up to three times a year, long periods of recovery, with general symptoms of asthenia and prolonged low-grade fever.
For the toxic-allergic form, more frequent exacerbations are typical, often with complications in the area of neighboring tissues (pharyngitis, peritonsillar abscesses), and the almost constant presence of asthenia and prolonged fever are typical.
The clinical picture of chronic tonsillitis during an exacerbation is as follows:
- sore throat that gets worse when swallowing;
- redness of the throat and tonsils;
- characteristic plaque;
- purulent discharge from the tonsils;
- bad breath;
- swelling of the nasopharynx;
- temperature increase;
- weakness;
- headache;
- fast fatiguability;
- arrhythmia;
- enlarged lymph nodes;
- dyspnea.
Symptoms of the disease
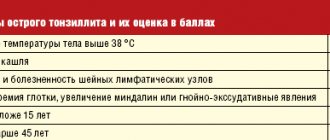
Angina:
- pain in the throat when swallowing;
- increase in body temperature;
- the presence of purulent plugs on the tonsils;
- headaches;
- enlarged lymph nodes and their pain;
- a state of general weakness.
Chronic stage of tonsillitis:
- discomfort and pain when swallowing;
- presence of bad odor from the mouth;
- excessive fatigue;
- slight increase in body temperature;
- sleep disturbance;
- enlargement and tenderness in the cervical lymph nodes.
Causes, main risk factors
Up to 30 different colonies of pathogenic microbes can be sown on the surface of the tonsils of patients suffering from chronic tonsillitis. But in crypts and lacunae staphylo- or streptococcus is usually determined. A key role in the pathogenesis of chronic tonsillitis is played by beta-hemolytic strains of streptococcus (type A). Other flora - gram-negative coccal, fungal, viral - have an impact on local immunity, they support inflammation.
There are a number of factors contributing to the occurrence of the disease:
- hypothermia;
- decreased immunity;
- microtrauma of the tonsils;
- foci of inflammation in the mouth and in the head area (caries, sinusitis, adenoids, etc.);
- smoking;
- poor nutrition;
- allergy.
Viruses and bacteria that cause tonsillitis can come from the external environment.
Causes
Tonsillitis is an infectious disease. It can be caused by various types of viruses:
- adenovirus, enterovirus, influenza and parainfluenza viruses;
- Epstein-Barr virus, cytomegalovirus infection;
- pathogens of measles, herpes simplex and others.
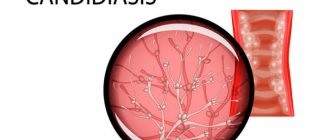
Bacterial tonsillitis is most often caused by streptococci. It can also be caused by staphylococci, gonococci, corynebacterium diphtheria, anaerobic flora, and spirochetes. Candida sore throat sometimes occurs in young children.
The development of the disease also involves factors that reduce the overall resistance of the body - hypothermia, malnutrition, prolonged emotional stress and others.
Treatment for tonsillitis depends on its causes. To determine the causative agent, timely consultation with a doctor is necessary.
Classification
Doctors distinguish various clinical forms of chronic tonsillitis, differing in clinical manifestations, severity of the condition and prognosis, risk of complications, as well as treatment tactics.
The simple form of chronic tonsillitis is characterized by a predominance of local symptoms. If general manifestations and lymphadenitis occur, this is referred to as a toxic-allergic form of tonsillitis. It comes in two versions:
Toxic-allergic chronic tonsillitis 1st degree . Sore throats are typical for him, which can worsen after ARVI, combined with general symptoms.
Toxic-allergic chronic tonsillitis of the 2nd degree - the symptoms are more pronounced, associated with diseases that have common factors of etiology and pathogenesis.
According to the degree of compensation of the process, the disease is divided into two options:
- chronic tonsillitis, compensated form - the source of infection is in a dormant state, there are no reactions from the body, repeated sore throats do not occur; The function of the tonsils and general reactivity are not impaired.
- chronic tonsillitis is a decompensated form - relapses of sore throat occur, complications of the heart, damage to the paranasal sinuses, middle ear, and renal complications are possible.
According to pathomorphological criteria, the process is divided into the following options:
- lacunar tonsillitis with predominant damage to the area of the lacunae;
- parenchymal-lacunar, involving in addition to the lacunae also the area of the lymphoid tissue of the tonsils themselves;
- phlegmonous - inflammation is predominantly localized in the area of lymphoid tissue;
- sclerotic with abundant growth of connective tissue fibers in the area of the tonsils and surrounding tissue.
Development mechanism and reasons
The palatine tonsils, or tonsils, along with the lymphoid structures of the oropharynx, perform the function of protection against pathogenic microorganisms and viruses. When local immunity decreases or the number of pathogen colonies increases, an exacerbation occurs - acute tonsillitis.
Recurrent tonsillitis leads to chronic tonsillitis. It is extremely rare that chronicity of the disease occurs after primary inflammation, and also without previous sore throats.
More than 30 pathogenic microorganisms can provoke tonsillitis, but staphylococcus and streptococcal infections are most often detected. The main role is played by the activity of streptococcus. Other microorganisms contribute more to reducing local immunity and maintaining the inflammatory process.
Provoking factors:
- past infections;
- immunodeficiencies, including those caused by immunosuppressive therapy;
- hypothermia;
- seasonal allergies;
- adenoiditis;
- inflammatory foci in neighboring sections;
- polyps and others.
Chronic angina is promoted by improper or incomplete treatment of the acute form of the disease, self-medication and unjustified symptomatic therapy.
Complications of chronic tonsillitis
Against the background of a chronic inflammatory process in the tonsil area, various complications are possible. Therefore, it is important to know why chronic tonsillitis is dangerous. Thus, the tonsils themselves, losing their function as a barrier to infection, become its breeding ground. Inside them are pathogens with the products of their metabolism. The infection can spread throughout organs and tissues, affecting the renal parenchyma, joint and heart tissue, and liver. In addition, tonsillitis adversely affects the functioning of the immune system and can be a provocateur of collagen diseases - lupus, scleroderma, dermatomyositis, periarteritis. The skin and peripheral nerve fibers may also be affected. With prolonged intoxication against the background of the disease, damage to blood vessels (vasculitis) and platelets (purpura) is possible.
Complications of tonsillitis
Tonsillitis, both acute and chronic, can cause local and general complications.
The first group includes damage to the tissues of the pharynx: paratonsillar abscess, parapharyngitis, laryngitis. Local complications also include acute otitis media and cervical lymphadenitis.
Common complications associated with damage to internal organs:
- diseases of the joints and connective tissue: rheumatism, rheumatoid arthritis, infectious polyarthritis, systemic lupus erythematosus;
- damage to the heart and mediastinum: myocarditis with the development of dilated cardiomyopathy and heart failure, mediastinitis;
- inflammation of the lungs, kidneys, appendix, sepsis and others.
To avoid the development of such complications, if there are symptoms of tonsillitis, it is necessary to carry out its full treatment.
Diagnostics
Diagnosis of chronic tonsillitis occurs on the basis of complaints, examination of the patient, and questioning of the patient. Objective signs, manifestations of chronic tonsillitis, and the general condition of the tonsils are important; the doctor determines the stages of the process and the form.
The following diagnostic procedures are also carried out:
- throat swab for flora;
- general blood and urine tests;
- blood test for antibodies to streptococcus.
This helps determine treatments for chronic tonsillitis.
Systemic therapy for the treatment of chronic tonsillitis at IAKI LLC
Washing the lacunae of the tonsils in combination with physiotherapeutic procedures has a good therapeutic effect and is widely used at the Institute.
First stage (washing the lacunae of the tonsils)
1. Washing of the tonsils can be done using the Belogolov’s method (Fig. 1) and using hardware methods (using the ATMOS ENT combine (Fig. 2) and the Tonsilor-M apparatus, etc.).
The choice of method depends on diagnostic and therapeutic purposes and is determined by an otorhinolaryngologist.
The antiseptic pressure created by the syringe piston effectively removes large purulent plugs. The disadvantage of the method is that it is traumatic when there is a pronounced gag reflex and the inability to qualitatively clean lacunae of small and medium diameter from purulent caseous contents. This method is widely used when it is necessary to obtain material for diagnostics, as well as for certain anatomical features of the structure of the palatine tonsils.
Rice. 1. Washing according to Belogolov’s method
2. Rinsing the lacunae of the palatine tonsils with a vacuum apparatus “ATMOS” (Fig. 2).
During rinsing, vacuum action allows you to effectively and painlessly remove even purulent plugs located deep in the lacunae. The method is non-traumatic and suitable for treatment in all age groups (vacuum attachments are selected taking into account the age and size of the tonsils). During rinsing, the tonsil is treated with an antiseptic solution.
3. Vacuum rinsing of the palatine tonsils with the “Tonsilor-M” apparatus (Fig. 2)
One of the advanced and effective methods of conservative treatment of chronic tonsillitis. The principle of operation of the Tonsilor-M device is based on creating a vacuum at the point of application and emitting low-frequency ultrasound onto the affected tissue of the palatine tonsil. Ultrasonic waves provide cavitation and aspiration of purulent contents from the lacunae of the tonsils, accelerate regeneration processes without causing allergic reactions or addiction, enhancing the therapeutic effect. The device is equipped with special nozzles that allow you to deliver an antiseptic solution directly to the tonsils.
Rice. 2. Washing using an ENT combine “ATMOS”, a device “Tonsilor-M”
Second stage (treatment with an astringent antiseptic solution)
After washing the lacunae of the palatine tonsils and clearing them of purulent contents, the tonsil tissue is soaked with a tampon with an astringent antiseptic agent (Fig. 3).
Rice. 3. Treatment of tonsils with an antiseptic solution
Third stage (laser therapy)
The next stage is a physiotherapeutic effect on the tissue of the palatine tonsil (Fig. 4) using a low-intensity ultraviolet laser beam, aimed at reducing swelling and inflammation of the tissue of the palatine tonsils.
Rice. 4. Laser therapy session after rinsing
Fourth stage (transdermal (percutaneous) exposure to an infrared magnetic laser)
Next, a transdermal (percutaneous) effect of an infrared magnetic laser (Fig. 5) is performed on reflexogenic ENT points: the maxillary region of the projection of the palatine tonsils, the region of the larynx and thyroid cartilage and the projection region of the exit site of the second branch of the trigeminal nerve on the face.
Rice. 5. Transdermal (percutaneous) exposure to an infrared magnetic laser
Fifth stage (vibroacoustic impact)
It is recommended to conduct sessions of vibroacoustic influence; the use of this method is necessary to improve the trophic (nutritional) function and normalize microcirculation in the tissues of the palatine tonsils.
Stage six (therapeutic low-intensity laser exposure)
In some cases, in the treatment of chronic tonsillitis, it is possible to alternate a therapeutic low-intensity laser (Fig. 7, Fig. 8) with other types of physiotherapeutic effects: ultraviolet irradiation (UVR, “quartz tube”) of the mucous membranes of the ENT organs and vibroacoustic effects on the projection area of the palatine tonsils.
This method allows for the sanitation of the microflora located on the surface of the palatine tonsils and the nasal cavity due to ultraviolet irradiation (UVR).
Rice. 7. Sanitation of the microflora of the nasal cavity using ultraviolet irradiation.
Rice. 8. Sanitation of microflora on the surface of the tonsils using ultraviolet irradiation.
Systemic therapy for chronic tonsillitis is carried out in courses (usually spring, autumn). The number of procedures is determined by an otorhinolaryngologist. For a lasting effect to occur, at least five sessions must be performed. If, during the procedure, purulent caseous contents continue to be washed out of the lacunae of the palatine tonsils, the washing procedures must be continued “until clean rinsing waters”. Typically the course duration is 10 procedures.
It is advisable to conduct courses 2 to 4 times a year; between courses it is necessary to carry out medication prescribed by an ENT doctor.
A course of washing the tonsils not only reduces the risk of exacerbation of chronic tonsillitis, but also prevents the occurrence of other ENT pathologies, and also avoids the need to remove the tonsils.
Attention! If, after completing the course, the formation of purulent caseous contents occurs 2-4 weeks later, the doctor may recommend surgical removal of the tonsils.
With systemic therapy, surgical treatment methods are rarely used!
The consequences of chronic tonsillitis most affect the heart and joints! Rheumatism of the joints, inflammation of the myocardium, endocardium can be a consequence of chronic tonsillitis! DO NOT SELF-medicate! CONTACT AN OTOLARINGOLOGIST!
It is not recommended to use antibacterial drugs in the chronic process, however, in the acute period there is a need for their use.
Attention!
The selection of drug therapy should be made individually, taking into account the severity of the disease, the presence of concomitant diseases, the patient’s age and the risk of possible side effects. Strictly follow the instructions of the otorhinolaryngologist! We ask you not to self-medicate based on Internet data!
Branch phone:
+7 (495) 695-56-95
Treatment methods in adults
In most cases, they resort to conservative treatment of chronic tonsillitis. Source: Modern methods of treating chronic tonsillitis. Ryazantsev S.V., Eremina N.V., Shcherban K.Yu. Medical Council, 2022. p. 68-72:
- therapy for inflammation in the head and oral cavity;
- procedures that increase immunity (hardening, taking vitamins, physical education, etc.);
- hyposensitizing drugs (to suppress allergic reactions);
- immunomodulators (normalize the immune system);
- means of reflex action (acupuncture, manual therapy);
- washing the tonsils with antiseptics;
- administration of drugs to the tonsils.
The treatment plan is complemented by physical therapy for chronic tonsillitis.
A radical method of treating chronic tonsillitis is surgical removal of the tonsils (tonsillectomy). The operation is performed in cases where inflammation occurs more than five times a year and does not respond to complex conservative treatment of chronic tonsillitis. Source: Choosing an antibiotic for exacerbation of tonsillitis. Karpishchenko S.A., Kolesnikova O.M. Medical Council, 2015. p. 40-43.
Treatment
There are two main methods of treatment: surgical and conservative.
The treatment method is determined by an otorhinolaryngologist, which depends on:
- forms of chronic inflammation;
- frequency of exacerbations;
- the presence or absence of beta-hemolytic streptococcus in the tonsils;
- effectiveness of previous therapy.
Conservative treatment method:
- Local antibiotic therapy
- Systemic antibiotic therapy (tablet or injection forms).
- Rinsing the lacunae of the tonsils and introducing antibacterial and anti-inflammatory drugs into them.
- Physiotherapeutic procedures:
- phonophoresis of drugs,
- ultraviolet radiation (UV),
- magnetic laser therapy (MILTA),
- vibroacoustic impact.
Prevention of chronic tonsillitis in adults
Preventive measures to prevent chronic tonsillitis include:
- proper hygiene;
- hardening;
- balanced diet;
- maintaining cleanliness in the home and workplace, eliminating dust;
- timely treatment of inflammationSource: Treatment and prevention of chronic tonsillitis. Atagulova G. Zh. Medicine and ecology, 2012.
Chronic tonsillitis is a very common disease that causes a lot of inconvenience to the patient. But is it possible to cure chronic tonsillitis? If your tonsils often become inflamed, then do not self-medicate, but consult a doctor who will select the optimal treatment regimen for you and determine how to get rid of chronic tonsillitis. You can make an appointment with a medical specialist in St. Petersburg by calling the phone number listed on the website.
Article sources:
- Treatment and prevention of chronic tonsillitis. Atagulova G. Zh. Medicine and ecology, 2012
- Chronic tonsillitis in the practice of an otolaryngologist and cardiologist. Yalymova D.L., Kostyuk V.N., Vishnyakov V.V., Yalymov A.A., Shekhyan G.G., Zadionchenko V.S. Cardio Somatics, 2014. p. 60-65
- Choice of antibiotic for exacerbation of tonsillitis. Karpishchenko S.A., Kolesnikova O.M. Medical Council, 2015. p. 40-43
- Modern methods of treating chronic tonsillitis. Ryazantsev S.V., Eremina N.V., Shcherban K.Yu. Medical Council, 2022. p. 68-72
Forms of tonsillitis
There is a large classification of forms of acute tonsillitis :
Catarrhal
The mildest form, in which the mucous membrane of the tonsils is affected. The palatine tonsils are not very enlarged, the mucous membrane of the throat is red, there is no plaque or pus.
Follicular
In this form, the follicles of the tonsils, that is, the deeper structures of the tonsils, are affected. They are visible through the tissue of the tonsils in the form of whitish-yellow round formations.
Lacunarnaya
It leaks more severely. When examined, yellowish-white and purulent plaques can be seen on the tonsils.
Fibrinous
A dense film of grayish fibrin forms on the tonsil, which is difficult to remove with a spatula.
Herpetic
Characterized by the appearance of blisters on the tonsils. When they rupture, painful, difficult-to-heal ulcers form.
Phlegmonous
With this form, after 1-2 days of acute tonsillitis, an abscess (cavity with pus) develops.
Ulcerative-necrotic
Angina of Simanovsky-Plaut-Vincent.
As a rule, one tonsil is involved in the process, on which a grayish-yellowish coating forms with the development of ulcers underneath it.
Mixed forms
In this variant of the disease, infection occurs with several pathogens at once, as a result of the addition of a secondary infection or with a severe decrease in immunity.
Chronic form of tonsillitis
Relevant in the same way as acute.
Understanding the significance and prevalence of bacterial tonsillitis pathogens, especially group A beta-hemolytic streptococcus, has a huge role in preventing the development of chronic tonsillitis. Allergic syndrome is caused by the allergenic effect of streptococcal lipopolysaccharides, which, when absorbed throughout the disease, cause an allergic mood and create the preconditions for the development of local and general complications.
Conservative therapy
Depending on the diagnostic results, the doctor draws up an individual treatment plan. Acute tonsillitis is treated by a therapist on an outpatient basis using conservative methods, using antibacterial drugs in the form of tablets, rinsing, washing, and irrigation of tonsil lacunae.
Therapy of chronic tonsillitis is the responsibility of an otolaryngologist, who acts together with an immunologist.
A good result in the treatment of the disease is achieved by affecting the tonsils themselves. The hospital's otolaryngologists conduct courses of medical manipulations, during which:
- caseous plugs are removed;
- The folds of the tonsils (lacunae), which hide foci of infection, are cleaned.
During the treatment process - washing, lubricating and irrigating the tonsils with medicinal solutions, inflammation is stopped, the compensatory stage of the disease is prolonged, which makes it possible to delay or avoid tonsillectomy. Additionally, complex treatment at home is prescribed.
Reviews
Andrey
For most of my life I was tormented by constant exacerbations of chronic tonsillitis. Every spring and autumn I consistently lost two weeks for treatment. Surgery to remove tonsils has bothered me since childhood. My wife almost forcibly brought me to the clinic. I didn’t even imagine that new techniques can eliminate the problem absolutely painlessly. I have been living without constant exacerbations for a year now, and I am very grateful to the hospital specialists for this.
Natalia
Not long ago I had to bring my child to have his tonsils removed. From my own experience I remember how unpleasant and painful this procedure is. I was more worried than my son. However, the clinic doctors were able to find an approach to the child and calm him down. The operation was performed without pain or blood. Now I know for sure that your clinic employs super specialists and kind, sympathetic people.
Diagnosis of the disease
The first stage of a diagnostic examination is examination of the patient. The condition of the pharynx is assessed using special lighting, as a result of which the doctor notes enlarged lymph nodes, pronounced redness of the tonsils, yellowish purulent plaque and other signs characteristic of tonsillitis.
The next step, which is very important for prescribing competent treatment for tonsillitis, is taking tests. To determine the causative agent of the disease, a smear is taken from the surface of the tonsils and the posterior wall of the nasopharynx. This analysis is sent to the laboratory, where the material will be further examined. The presence of a certain group of microorganisms allows us to understand what specifically provoked damage to the tonsils and led to tonsillitis.
A blood test is also taken for examination. Indicators that confirm the presence of the disease will exceed the normal level:
- The ESR indicator reaches 18–20 mm/h.
- The number of immature neutrophils increases.
- The level of neutrophils in the blood reaches 7-9x109/l.
- The presence of metamyelocytes and myelocytes is detected.
A test to determine sensitivity to antibiotics allows the doctor to select the most effective treatment in the future. During treatment, the doctor will prescribe antibiotics, each of which is capable of suppressing the proliferation of a certain group of pathogenic microorganisms.
We care about your health
Tonsillitis is one of the most common diseases. Infections of a viral or bacterial nature enter the respiratory tract (often one of them is joined by another), causing an inflammatory process. A surge in tonsillitis is most often observed in the spring and winter, when many people have a weakened immune system. Also, this disease can develop against the background of existing foci of infections in the body, for example, with dental caries, periodontal disease, sinusitis and others.
Tonsillitis is transmitted mainly by airborne droplets, pathogens: staphylococci, streptococci, fungi, bacilli.
Tonsillitis can have both acute (called sore throat) and chronic forms. Acute tonsillitis most often occurs as a result of an exacerbation of the chronic form, when a person with reduced immunity could, for example, become hypothermic.
Symptoms of tonsillitis
Compared to chronic tonsillitis, acute tonsillitis occurs in a more severe form: the body temperature can rise to 40 degrees, the patient feels a very strong pain in the throat, and it is difficult for him to swallow. The tonsils are swollen and enlarged, with the presence of purulent plugs. Patients feel headache, weakness, and their lymph nodes are enlarged.
Depending on the type of sore throat, which can be lacunar, herpetic, catarrhal, follicular, etc., ulcers, follicles, and a film called plaque form on the palatine tonsils.
With chronic tonsillitis, the temperature can rise to 38. The patient has a light coating on the palatine tonsils, and the tonsils themselves look enlarged and reddened. A person feels weakness, muscle pain, and aching joints.
Chronic tonsillitis is characterized by stages of remission and exacerbation. During the period of remission, the focus of infection is passive, and the person is not bothered by unpleasant symptoms. But as soon as one becomes hypothermic (especially with reduced immunity), he immediately begins to feel an unpleasant sore throat, pain when swallowing, cough, fatigue, poor general health and lack of appetite. The patient's lymph nodes may become inflamed.
Chronic tonsillitis is a long-term inflammation of the pharynx and palate. Its simple form has only a local symptom: sore throat. But if the picture is complemented by persistent lymphadenitis of the neck, changes in the functioning of the heart and high temperature, then this is already a toxic-allergic form.
Chronic tonsillitis has several stages: compensated, when the source of infection is not active, and decompensated, when exacerbation occurs due to repeated sore throats, inflammation of the ear and nose.
Tonsillitis (tonsillitis) - what inflammation looks like (photo of the disease)
Photograph of the throat with purulent sore throat
Photo - throat with follicular sore throat
Catarrhal sore throat - photo
Photo - lacunar tonsillitis
Possible complications of tonsillitis
Like many other diseases, tonsillitis is dangerous due to its complications . These include, first of all, rheumatism. After suffering from a sore throat, a person may feel severe aching in the joints and an increase in temperature.
In second place, as a rule, are cardiovascular diseases. Interruptions in heart function, shortness of breath, tachycardia are sure signs that a sore throat has caused complications.
Another unpleasant symptom after tonsillitis is swelling and tenderness of the lymph nodes, which have become infected from the tonsils. This is lymphadenitis.
The infection can also spread from the tonsils to the surrounding tissues of the upper respiratory tract, leading to pain when swallowing. And this disease is a complication of tonsillitis and is called paratonsillitis.
It should be noted that more than a hundred diseases are known that arise as a result of complications after acute tonsillitis. These include a variety of kidney, eye, skin and thyroid diseases.
Diagnosis of tonsillitis
It begins, of course, with an examination by a doctor, who determines whether the tonsils and adjacent tissues are swollen and red, and whether the ear and cervical lymph nodes are inflamed. The patient is sent for a general blood test.
Before prescribing treatment to the patient, the ENT doctor determines the nature of the inflammatory process: in what form does tonsillitis occur - chronic or acute, the type of inflammation (purulent, catarrhal), is the sore throat primary or secondary, what is the causative agent (this is determined in the laboratory - a culture is done from the throat ).
Treatment of tonsillitis - specifics of therapy
In the treatment of tonsillitis, both conservative methods and surgical intervention can be used. Treatment methods depend on the specifics of the disease.
For chronic tonsillitis, if necessary, antibiotics are prescribed in tablets, and for sore throat they are often administered intramuscularly. Local treatment is also carried out: purulent plaque on the tonsils is removed, the lacunae are washed with antibacterial solutions, physiotherapy and a course of vitamins with immunomodulators are prescribed.
In case of acute tonsillitis, it is recommended to irrigate the oral cavity with antiseptic solutions, rinse, treat the tonsils with iodine-containing preparations (if there are no allergic reactions to iodine), inhalations, and resorption of antibacterial tablets are useful. You should also drink a lot (weak teas, fruit drinks, juices, rosehip decoctions, etc.), take antipyretic and painkillers.
Acute tonsillitis is not recommended to be treated with antibiotics, because they reduce local immunity. But if the form of the disease is more severe, then the patient requires mandatory bed rest and antibiotic therapy. However, the prescription of antibiotics should be preceded by an analysis of the results of culture in the pharynx area, which will identify the causative agent of the infection. It is recommended to include in the course of treatment drugs that enhance immunity, as well as general strengthening and anti-inflammatory drugs. Physiotherapy will also be useful.
If a person suffers from tonsillitis more than twice a year, has complications from this disease, and conservative treatment does not bring the expected results, then removal of the tonsils may be recommended. There are many modern methods of performing this operation (infrared laser, ultrasound, biopolar, radiofrequency ablation and others), but many consider the cold plasma coblation method to be the most effective and gentle. However, it should be remembered that the tonsils are the first protective barrier that stops and disarms pathogenic bacteria . But in many cases (especially after frequent colds), the tonsils stop performing their functions and themselves become a source of infection, causing serious complications. In this case, it is better to remove them.
Treatment of tonsillitis (tonsillitis) at the Medkvadrat ENT center in Moscow, Kurkino and Khimki.