From this article you will learn:
- why does the socket hurt after tooth extraction,
- what is alveolitis: photos and videos,
- How is alveolitis treated?
The article was written by a dental surgeon with more than 19 years of experience.
Alveolitis is a classic complication that occurs after tooth extraction and consists of the development of inflammation of the socket of the extracted tooth. Often alveolitis is also called “dry socket” (this is due to the fact that the alveolar bone in the depths of the socket is exposed due to the loss of a blood clot).
On average, alveolitis develops after tooth extraction in 3-5% of cases, but this applies to teeth of any location with the exception of wisdom teeth. When the latter are removed, alveolitis occurs in 25-30% of cases, which is associated with the greater complexity and traumatic nature of the removal process.
Dry socket after tooth extraction: photo
You can see what normal healing of a socket should look like (at different times from the moment of extraction) in the photo in the article: → “What a socket should look like after tooth extraction”
Dry tooth socket: features of the disease
A dry socket appears in two cases after tooth extraction. In the first, a blood clot may fall out or dissolve, while in the second, it may not form initially (usually due to severe bleeding). On average, a similar diagnosis is made to two to five percent of people who have undergone a tooth extraction procedure, but dry socket after wisdom tooth removal is much more common. In the absence of timely treatment, the disease can progress to the stage of alveolitis, which in turn threatens the appearance of phlegmon or an abscess. What does a dry socket look like? Visually, a dry tooth socket is easy to identify: in the absence of a blood clot, part of the bone is exposed.
Symptoms of dry socket
- After 2 - 3 days, the gums begin to become inflamed and pain appears.
- As the inflammatory process develops, pain increases and manifests itself not only in the oral cavity, but also in the cervical region, as well as in the ear area.
- The appearance of an unpleasant odor and specific taste in the mouth is another characteristic symptom.
- Partial hearing loss may occur.
Indications
In addition to the above cases, curettage of the tooth socket is also prescribed in case of detection of an infectious lesion of the tissue structure, diagnosing alveolitis or the effect of a dry cavity. Typical symptoms that necessitate medical intervention include:
- Pain syndrome that persists for more than 3-4 days after surgery.
- Increased temperature, inflammation of the gums in the area of removal, acute reaction to chewing load.
Negative symptoms are typical only for the first 48 hours, and are caused by the body’s natural reaction to the changes that have occurred. If severe discomfort persists, it is recommended to immediately consult your doctor and undergo a re-examination.
Causes of dry socket after tooth extraction
- Smoking (especially immediately after tooth extraction).
- Poor oral hygiene over a long period of time.
- Poor blood clotting or taking blood thinners.
- Frequent rinsing of the mouth.
- Mechanical impact on the socket and soft tissue in its area.
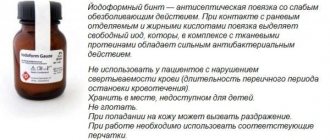
In addition to the factors mentioned above, much depends on the extraction procedure itself: improperly performed tooth extraction contributes to a number of complications, including dry socket and alveolitis. To prevent this unpleasant phenomenon, dentists recommend limiting physical activity for a few days after tooth extraction, and also not chewing on this side of the jaw (especially hard foods). Under no circumstances should you touch the hole and the area around it with your hands or foreign objects. Bad habits (drinking alcohol and smoking) should be eliminated during healing. The doctor usually prescribes anti-inflammatory drugs for rinsing the mouth (miramistin, chlorhexidine or furatsilin), but this procedure should be carried out no more than 2 - 3 times a day.
What can you do at home -
After the acute symptoms of inflammation have subsided, there is no need for antiseptic turundas inside the socket, because they do not help the wound to heal (epithelialize) faster. At this stage, the best treatment method will be to fill the hole with a special Dental adhesive paste (Solcoseryl). This drug has an excellent analgesic effect (after 2-3 hours the pain will practically stop, and after 1-2 days it will go away completely), and also speeds up healing many times over.
Scheme of use - this paste is added to a hole that has been washed with an antiseptic and slightly dried with a dry gauze swab (completely filling the hole). The paste is perfectly fixed in the hole and does not fall out of it. There is no need to remove the paste from the hole, because... it slowly dissolves on its own, giving way to growing gum tissue. The only thing that may be required is to periodically add it to the hole.
How to rinse the hole from food debris -
In some situations (when the turunda has fallen out of the hole, and there is no way to see a doctor right away), it may be necessary to wash the hole. After all, after each meal, the hole will become clogged with food debris, which will cause new inflammation. Rinsing will not help here, but you can easily rinse the hole with a syringe.
Important : from the very beginning you must bite off the sharp edge of the needle from the syringe! Next, bend the needle a little and fill a 5.0 ml syringe with a solution of Chlorhexidine 0.12-0.2% (it is sold ready-made in every pharmacy for 20-30 rubles). Screw the needle tightly so that it does not fly off when pressing the syringe plunger! Place the blunt end of a bent needle into the upper part of the socket (do not insert too deeply to avoid injuring the tissue), and rinse the socket under pressure. If necessary, do this after every meal.
In principle, after this the hole can be dried with a gauze swab and treated with Solcoseryl. We hope that our article on the topic: Alveolitis after tooth extraction, symptoms, treatment - turned out to be useful to you!
Sources:
1. Higher prof. the author’s education in surgical dentistry, 2. Based on personal experience as a dental surgeon, 3. National Library of Medicine (USA), 4. “Outpatient surgical dentistry” (Bezrukov V.), 5. “Propaedeutics of surgical dentistry” (Soloviev M. .).
Treatment methods for dry tooth socket
If you discover symptoms of a dry socket, immediately contact your dentist: in this case, you should not self-medicate, although on the Internet you can find a lot of advice on how to treat a dry socket at home. Can a dry socket heal on its own? Without therapeutic and preventive measures, the healing process is not always successful and takes longer. What kind of dry socket treatment will be carried out after tooth extraction depends on the degree of development of the inflammatory process.
| Degree of complication | Treatment method |
| Lightweight | Antiseptic and anti-inflammatory drugs available without a prescription. |
| Average | Antibacterial therapy, cleaning the hole and filling it with anti-inflammatory gel. |
| Heavy | In severe stages of the disease (cellulitis, abscess), the patient is sometimes hospitalized, and a number of measures are taken for his rehabilitation, including physical therapy and ultraviolet irradiation. |
Treatment of a dry socket after the removal of a wisdom tooth is carried out in the same way as in the case of other teeth, however, access to the area of inflammation can be complicated due to the distance of the “eight” location.
General overview
From a technical point of view, socket curettage is a procedure for mechanical cleaning of the inner surface of the alveolar bed. The use of special instruments allows you to prevent the development of a pathological condition, remove foreign objects and deep deposits characteristic of periodontitis. During the planned removal of elements of the dentition characterized by the presence of cystic formations, as well as with diagnosed periodontitis, the procedure is included in the general protocol and is carried out immediately after extraction, eliminating the possibility of side effects.
How long does it take for a dry socket to heal?
Many people are interested in the question of how long it takes for a dry socket to heal. In the absence of complications, the wound heals in 5 - 7 days, and within a month the hole is filled with epithelial tissue. If you have dry socket, the healing process may take longer than two weeks (with proper treatment, of course). As already mentioned, extensive inflammation may occur and even require surgical hospitalization of the patient: in this case, the healing of the dry socket may be very delayed.
Stages of socket healing by day
- The bleeding that occurs after tooth extraction stops after a few minutes , and a blood clot is formed that protects the wound from the penetration of microbes. Under the clot, damaged tissue is being restored, so it is so important to maintain its integrity until the hole heals completely.
- Day 1 – the processes of epithelization (healing) of the wound surface begin.
- Day 3 - signs of epithelization become noticeable, healing begins from the edges of the wound and moves towards the center.
- Day 4 - granulation tissue begins to form - a type of connective tissue that is formed in the body only during wound healing by secondary intention, when there is a strong defect in the skin.
- Day 7 - granulation tissue replaces part of the blood clot, it remains only in the center of the hole. Osteoid (bone) beams begin to appear, indicating bone formation. At the same time, epithelial tissue grows significantly from the edges of the gums.
- 14th -18th day - epithelization of the wound is completely completed, its surface is tightened and heals completely. By this time, the hole is completely filled with granulation tissue, and osteoid tissue is actively developing.
- After a month, a significant part of the hole is filled with new bone tissue. By the end of the second, sometimes third month, this process is completely completed.
- 4th month - bone beams in the newly formed osteoid tissue calcify, it matures: it becomes spongy and does not differ from the rest of the bone. At the same time, the edges of the socket dissolve, the alveolar edge in the area of the extracted tooth becomes thinner and lower than it was before surgery.
Causes
After a tooth has been removed, alveolitis of the socket often occurs. Certain factors may contribute to this:
- the blood clot, which prevents infection from entering the wound, has been destroyed;
- bone fragments, stone, plaque got into the hole during the removal procedure;
- the specialist did not clean the hole very well from granulations and granules;
- sterility was compromised;
- the removal was very traumatic;
- the patient did not follow all the doctor’s instructions;
- The patient's body is exhausted, immunity is quite low.
When a regular tooth or wisdom tooth has been removed, you should not rinse your mouth too vigorously, as there is a risk that the blood clot located in the socket will be washed out. The result is that microbes get inside and provoke an inflammatory process.
Diagnostics
Such a diagnosis is made only by a doctor when he examines the oral cavity. You can't diagnose yourself. After all, alveolitis of the socket is a serious disease.
If it is not treated promptly, serious complications are possible, including blood poisoning. If there is no blood clot at the place where the tooth was pulled out, then this indicates alveolitis.
Blackening of the gums
A change in gum color does not always indicate the onset of inflammatory processes. If the gums at the site of the incision become whitish, this is considered one of the normal variants. This is how fibrin manifests itself, which tightens the wound and protects it from bacteria getting inside.
However, if the bed and adjacent fabrics have turned dark blue or black, this is a cause for concern. Blueness indicates the transition of inflammation to the third stage, which can lead to complete atrophy of the gum tissue.
The gums begin to turn black already when the irreversible process of decay has begun. This is usually accompanied by purulent discharge, a strong and very unpleasant odor from the mouth, and severe pain that cannot be controlled with conventional painkillers.