Symptoms of the disease
This pathology occurs in type I diabetes mellitus, but can also occur in type II diabetes. Therefore, at the first signs of illness, immediately consult a doctor to prescribe treatment.
Symptoms include:
- Abdominal pain.
- Vomit.
- Cardiopalmus.
- Acetone smell on your breath (or other unusual odor).
- Dehydration of the body (dehydration).
- Disorientation in space, confusion.
- Unconsciousness (or coma).
Ketone bodies are found in urine.
The smell of acetone on your breath - does diet matter?
The content of the article
An acetone odor from the breath is felt in people on a low-sugar diet. A decrease in the concentration of carbohydrates leads to the fact that the main source of energy for the body becomes fats, which form ketone bodies. Fats will also be the main source of energy received by the body in case of fasting and a small supply of sugars.
Symptoms of elevated ketone levels due to the ketogenic diet:
- Smell of acetone from the mouth.
An increased concentration of ketones is indicated by a noticeable smell of sour apples from the mouth. - Decreased activity
. Reducing the intake of carbohydrates initially leads to a feeling of constant fatigue, dizziness and nausea. Physical strength also decreases. This state lasts for several days or weeks until the body begins to burn more fat and switches to a new source of energy. - Disruption of the gastrointestinal tract
. The ketogenic diet can also lead to diarrhea and constipation. - Insomnia.
Sleep disturbances are a kind of signal from the body about carbohydrate deficiency. - Decreased appetite.
Patients begin to lose weight and appetite. This is due to the fact that a decrease in the concentration of carbohydrates in the blood leads to a decrease in the concentration of insulin and an increase in glucagon, which stimulates the oxidation of fatty acids. Increased protein degradation when using this diet can lead to negative consequences due to protein deficiency.
A low-carbohydrate, low-fat diet that leads to ketosis has long been used to treat epilepsy, especially in children.
Causes of the pathological condition
Ketoacidosis appears in the following cases:
- When a very low dose of insulin is administered.
- Eating large amounts of carbohydrates.
- Missing a dose of insulin.
- Excessive physical activity.
- Severe stress.
- Excessive alcohol consumption.
- The presence of an infectious disease.
- Using ecstasy or cocaine.
When blood sugar levels are significantly higher than normal, hyperglycemia occurs in the body and the number of ketone bodies increases.
How to prevent diabetes
It is important to understand that the symptoms of the disease clearly manifest themselves during the period when the level of glucose in the blood significantly exceeds the permissible values. At the initial stage of diabetes, symptoms are almost invisible. For this reason, all adult patients over 40 years of age are recommended to have their blood tested annually for sugar in order to timely diagnose the onset of the disease and prevent its further development.
Contact the medical office and you will receive qualified medical assistance from an endocrinologist in the diagnosis and treatment of diabetes mellitus in children and adults.
Mechanism of development of diabetic ketoacidosis
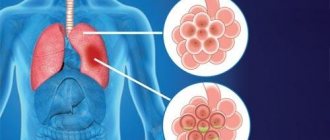
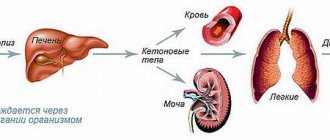
If there is a lack of insulin, the body cannot convert glucose into the energy it needs. Fat consumption begins. When they are used, ketone bodies accumulate in the body, the content of which rapidly increases. Ketone bodies cannot enter the blood due to the lack of insulin. They pass through the kidneys into the urine. A high content of by-products quickly poisons the body and leads to complications.
A patient who knows about the causes, symptoms, methods of prevention and treatment can avoid the occurrence of diabetic ketoacidosis.
Acetone breath and diabetes
Diabetes is a group of metabolic diseases that involve hyperglycemia—high blood sugar levels—associated with impaired insulin function or secretion. The patient's body, which cannot use carbohydrates as a source of energy as a result of impaired insulin secretion or action, begins to use fats for this purpose. As a result, ketone bodies are formed, which is the reason for the smell of acetone in the mouth. Some patients compare this smell to the smell of acid, gas or gasoline.
Chronic hyperglycemia causes damage to various organs, mainly the kidneys, eyes, blood vessels, heart and nerve fibers. There are several types of diabetes:
- type 1 diabetes;
- type 2 diabetes;
- gestational diabetes.
Type 1 diabetes is characterized by an absolute lack of insulin due to the destruction of beta cells in the pancreas. But the most common form of diabetes is type 2, which is characterized by impairment of both insulin secretion and function.
Diabetes
Typical symptoms of diabetes: increased thirst, polyuria, dehydration, drowsiness and weakness.
How to check your ketone levels?
As DKA develops, symptoms appear quickly. If one or more signs are present, blood and urine are tested for ketone bodies. They appear in the blood much faster than in the urine. To prevent poisoning of the body, perform the following measures:
- A blood test is performed to check for the presence of ketone bodies. If your home glucose meter can do this, use it. All you have to do is insert the required test strip.
- Study the result obtained. A value up to 0.6 mmol/l does not require any action. This indicator is considered the norm. An average level of 0.6-1.5 mmol/l indicates the beginning of the formation of ketone bodies in the body. Over the next 1.5-2 hours, you may need the help of a doctor. A high content of ketone bodies (more than 1.5 mmol/l) requires immediate medical attention and behavioral caution.
The attending physician is informed of the diagnosis and adheres to the prescribed recommendations.
Epidemiology of diabetes mellitus:
It should be noted that the incidence of diabetes mellitus is constantly increasing; according to various estimates, from 3 to 6% of the population in Russia suffer from this disease.
The development and progression of diabetes complications have the greatest impact on the life prognosis of patients with diabetes. It should be taken into account that with decompensation of diabetes mellitus, there is a continuous progression of complications of diabetes mellitus; all complications of diabetes mellitus occur in the initial stages (and this is precisely the time when they should be treated most intensively, since it is at this moment that the situation is often reversible) and are often asymptomatic , and the diagnosis can often be made on the basis of laboratory and instrumental research methods. This suggests that examination and treatment of complications of diabetes mellitus should be carried out as planned, regardless of the presence of patient complaints. This greatly creates difficulties in communication between the patient and the doctor, because the doctor often has to treat a patient who “doesn’t hurt anything,” which leads to low adherence to treatment in patients. This attitude of the patient towards the doctor’s recommendations often leads to the fact that the doctor must deal with advanced forms of the disease. It is more difficult to achieve a pronounced positive result in this case.
Diabetic distal polyneuropathy:
Complaints of a patient with diabetic distal polyneuropathy:
The overwhelming majority of patients with diabetes mellitus are characterized by complaints of pain in the lower extremities (pain in the feet of varying intensity at rest, more often at night and in the evening, numbness, goosebumps, episodes of increased sensitivity, chilliness of the feet, cramps in the muscles of the legs and feet, paresthesia, burning in the feet), dry skin, muscle atrophy, less frequent palpitations that occur at rest, unmotivated sweating, changes in blood pressure (for example, hypotension occurring after eating), impaired urination, decreased sexual function in men and women, dyspepsia.
Additional examination:
The diagnosis is made during an examination by an endocrinologist, neurologist, or podiatrist (the so-called “diabetic foot” specialist); specialists assess the degree of compensation for diabetes mellitus, various types of sensitivity, and the severity of changes. Electromyography of peripheral nerves is recommended.
Treatment:
- Normalization of carbohydrate metabolism is a necessary condition for the treatment of diabetic polyneuropathy
- Drug treatment: antiepileptic drugs, antidepressants, opioids, B vitamins (Milgama), alphalipoic acid drugs (Berlition, Thioctacid, Thiogamma)
- Physical methods of treatment: magnetic therapy (peripheral magnetic stimulation, treatment with a multimag apparatus), microwave resonance therapy, hyperbaric oxygen therapy, ozone therapy, etc. It should be noted that demyelination processes occur continuously in diabetic polyneuropathy, therefore treatment should be ongoing or in regular courses.
Microvascular complications of diabetes mellitus:
diabetic nephropathy, diabetic retinopathy.
Diabetic nephropathy
- specific kidney damage in diabetes mellitus, when the main functional unit of the kidneys (the vascular glomerulus) is damaged, the working tissue of the glomerulus is replaced with connective tissue, which does not perform a function. All this leads to a decrease in kidney function, the terminal stage of which is characterized by the development of chronic renal failure.
The prevalence of diabetic nephropathy increases the longer the duration of diabetes and can reach 50% or higher with a duration of 15-25 years.
There are three stages of diabetic nephropathy:
- DN, microalbuminuria stage;
- DN, stage of proteinuria and preserved nitrogen excretion function of the kidneys;
- DN, stage of chronic renal failure.
As a rule, patients with diabetic nephropathy in the proteinuria stage do not worry about anything. In the vast majority of cases, the disease is detected by examining urine for microalbuminuria. This study is recommended for all patients with diabetes mellitus 1-2 times a year, this is all the more important since at this stage the consequences are reversible.
With the development of diabetic nephropathy, the stage of proteinuria begins. This stage is characterized by the appearance of constant protein excretion in the urine, which corresponds to urinary albumin excretion of more than 200 mcg/min or 300 mg/day and protein excretion in a general urinalysis of more than 0.3 g/day. Patients also complain of swelling of the face in the morning, increased blood pressure, and occasional decreases in hemoglobin levels. If left untreated from the onset of proteinuria, renal failure develops on average after 5-7 years.
Diabetic nephropathy in the stage of chronic renal failure: the filtration function of the kidneys continues to steadily decline, leading to an increase in the concentration of nitrogenous waste (urea creatinine) and the appearance of electrolyte disturbances (increased potassium levels). In patients, protein excretion in the urine increases to 1.0-1.5 g/l and higher, swelling is noted on the face and limbs, blood pressure steadily rises to high numbers, and is difficult to treat. In severe cases, patients require renal replacement therapy (hemodialysis).
Treatment of diabetic nephropathy: treatment of diabetic nephropathy is complex and long-term, treatment is aimed at restoring the structural and functional integrity of vascular endothelial cells (achieved by prescribing angioprotective drugs (Sulodexide), treatment with physical methods (laser therapy), antioxidant therapy (including ozone therapy), therapy aimed at normalizing intraglomerular pressure (ACE inhibitors and angiotensin receptor antagonists are best suited for this).
Treatment
DKA requires immediate hospitalization and intensive care. With correct measures taken, the condition resolves within 24 hours. Perform the following actions:
- Blood sugar levels return to normal.
- They flood the body.
- Restores mineral balance.
With timely detection and correct diagnosis, ketoacidosis resolves without complications or with minimal negative consequences. If there is delay, coma or death occurs. Control of nutrition and blood glucose levels is the main prevention of the development of DKA.
Read also
Acromegaly
Somatotropic hormone is a hormone produced in the pituitary gland.
The main function of somatotropic hormone is to stimulate the growth of various body tissues. The biological effects of the hormone are... Read more
Osteoporosis
Osteoporosis is a progressive metabolic disease of the skeletal bones, which results in a decrease in bone density and disruption of its internal structure. The result of osteoporosis is...
More details
Diffuse nodular goiter, autoimmune thyroiditis, hypothyroidism
Chronic autoimmune thyroiditis, hypothyroidism, thyroid nodules. Thyroid diseases are a common problem in iodine-deficient regions (which include Samara...
More details
Pheochromocytoma
Pheochromocytoma is a tumor of the adrenal medulla that produces catecholamines (adrenaline, norepinephrine, dopamine). Pheochromocytoma consists of chromaffin cells. Pheochromocytoma may have...
More details
Metabolic syndrome
Metabolic syndrome is a “pandemic of the 21st century.” The prevalence of metabolic syndrome is 20–40%. In the Russian Federation, 40% of the population have 2 components of metabolic syndrome, 11% –...
More details
Ways to reduce odor
First of all, you need to determine the cause of halitosis. If diabetic halitosis with a characteristic ammonia odor is complemented by putrid, sour, rotten “odors,” you should undergo an examination of the internal organs, including:
- laboratory tests of urine and blood;
- ultrasound of the abdominal cavity (with kidneys).
If necessary, the treating endocrinologist may prescribe additional diagnostic procedures. To eliminate ketoacidosis, it is recommended to adjust the diet. In the daily menu, it is necessary to reduce the amount of protein foods and fats, replacing them with complex carbohydrates (porridges, vegetable dishes, fruits allowed for diabetes).
The following methods can be used to weaken the antipathetic amber:
- mint candies and tablets (for diabetics, the absence of sugar in the composition is important), mint leaves;
- anise seeds, juniper berries;
- sprays for mouth freshening with an antiseptic effect;
- pharmaceutical mouth rinses with eucalyptus, mint, menthol extracts
- decoctions of herbs with antibacterial properties (chamomile, sage, etc.) for rinsing;
- vegetable oil for rinsing the mouth (a five-minute procedure will help freshen your breath for a long time, but the oil should not be swallowed).
Regular oral hygiene is a prerequisite. When choosing a toothpaste, you should consult your dentist.
Halitosis test
When visiting a dentist, testing for halitosis is carried out using a special halitometer. The five-point scale of the device allows you to evaluate the result from “0” - no odor, to “5” - pronounced and sharp. At home, you can test yourself using a sterile pharmaceutical mask. You need to put it on and exhale forcefully.
In case of diseases of the teeth and gums, an environment favorable for the growth of bacteria is created in the oral cavity - the cause of an unpleasant odor
The freshness of your breath will be determined by the intensity of the perceptible “aroma”. Instead of a mask, you can use a cup or plastic bag, which must be pressed tightly to the mouth, take a deep breath and exhale as forcefully as possible. Another option is a wrist test. To do this, you need to lick this area of your hand, wait 20 seconds and smell.
Important! You can carry out independent manipulations to determine halitosis in the absence of rhinitis (runny nose) or other pathologies associated with a difficult sense of smell.