The symptoms of mucosal hypertrophy do not differ significantly from a simple runny nose.
Changes in the condition of the mucous membrane lining the inner surface of the supramillary sinus are caused by various processes and conditions of the ENT organs. Thickening of the mucous membrane of the maxillary sinuses is a precursor to the development of a serious inflammatory process.
Causes of thickening of the membranes
The internal tissues of the maxillary sinuses increase in volume in the following cases:
- improper treatment of rhinitis;
- frequent respiratory diseases;
- long-term allergic reactions;
- hypothermia of the body;
- if a polyp has formed in the sinus area;
- severe infectious diseases;
- acute states of deficiency of any vitamin;
- with congenital structural features of the nasal passages;
- when a foreign body enters the nasal cavity;
- when a patient takes hormonal drugs for various purposes.
Important: the prognosis of the course of the disease directly depends on the degree and area of tissue thickening; the more insignificant it is, the more likely a rapid and complete recovery is.
Changes in the mucosa can occur not only in the maxillary sinuses, but also in the frontal and ethmoid sinuses. In this case, the mucous membrane degenerates into connective tissue.
Thickening of the mucous membrane of the maxillary sinus is one of the components of the following diseases:
- chronic sinusitis (purulent, purulent-polypous, necrotic, parietal hyperplastic forms);
- allergic reactions and rhinitis.
If the acute form of the disease is not treated, it transforms into a chronic course of the disease. In this case, the condition periodically worsens, the symptoms intensify, which each time become more and more difficult to relieve. An inflammatory process that lasts more than two months is considered to be a chronic form of the condition.
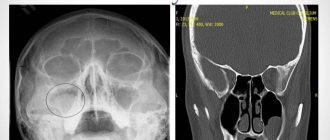
Mycetoma
non-invasive fungal sinusitis of the left maxillary sinus
The hypointense MR signal of a mycetoma may be mistaken for air in the paranasal sinus; Non-invasive fungal sinusitis does not look the same in different sequences.
If they are large, they cause headaches due to the pressure of the cyst shell on the walls of the sinus.
Often combined with allergic rhinitis, hypertrophy of the nasal turbinates and deviated nasal septum
Large cysts located in the lower parts of the maxillary sinus may be asymptomatic, while a small cyst located on the upper wall, in the area of the 2nd branch of the trigeminal nerve, can cause headaches.
Mucocele of the ethmoid labyrinth and frontal sinus on the right
This is a large formation of the paranasal sinus, lined with epithelium and filled with mucus, which is formed as a result of obstruction of the main sinus canal.
The most typical symptom: expansion of the paranasal sinus with smooth, clear contours with thinning and remodeling of the adjacent bone plate.
Symptoms of tissue thickening
Signs of changes in the condition of the maxillary sinus mucosa are not specific only to this case.
Important: the constant inflammatory process changes the mucous membrane, cracks form in it, and polyps grow.
The symptoms are similar to most symptoms of respiratory diseases.
The chronic condition is characterized by the following complaints from patients:
- Breathing is difficult both when inhaling and exhaling.
- Constant nasal discharge, which has a different appearance and consistency.
- Often the discharge smells like pus. It can be felt even when the patient breathes.
- It is difficult for the patient to blow his nose; there is a feeling of mucus, but it is difficult to remove it from the nasal cavity.
- This condition is characterized by a deterioration in the sense of smell, up to its complete loss.
- The patient's voice becomes nasal, the person speaks “into his nose.”
- There may be complaints of congestion, pain and tinnitus.
- If an increase in mucous occurs due to the development of sinusitis, then in the initial stages the mucus will be liquid. At this stage, sinusitis is catarrhal. As the disease progresses, it will become thicker and thicker. The development of a purulent stage of the disease is possible.
- Sometimes, when the mucous membrane of the maxillary sinuses thickens, a person’s eyelids swell and their eyes water. Their soreness may mistakenly suggest conjunctivitis.
- Headaches come in varying intensity, nature and location.
- Allergic reactions are accompanied by a liquid state of mucus discharged from the nose.
- In the cheek area, on the sides of the nose, pain appears, increasing with pressure.
- During an exacerbation, the body temperature rises and the condition worsens sharply.
When the acute stage passes, even if the condition has already become chronic, the patient begins to feel better. The satisfactory condition lasts until the next onset of the acute stage.
The patient gets used to his condition and the alternation of these periods; he does not consult a doctor.
Mechanisms of changes in the structure of the mucosa
Thickening of the internal tissues of the maxillary sinuses occurs according to the following principle:
- When the disease occurs, swelling and thickening occur. The ducts that remove mucus from the sinuses are located on the surface of the mucous membranes, which means that when there is swelling, they are blocked. The mucous membrane performs its function of producing mucus. In case of illness, it is produced more than in a normal situation.
- Excess mucus remains in the sinus, causing pressure. The walls of the sinus begin to stretch.
- With increased pressure, cysts grow. These formations are subject to uncontrolled growth in size.
- If pathogenic organisms penetrate the sinus cavity, the cyst tissue becomes inflamed.
- The cells begin to produce pus, which has no way out of the cavity.
Chronic sinusitis
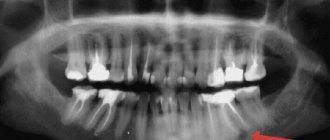
Occurs after untreated or untreated sinusitis; it can also occur in the event of a violation of the outflow of exudate (with a deviated nasal septum) or in the case of contact transmission of infection from the teeth (for example, teeth affected by caries - author's note) to the mucous membrane of the maxillary sinus (odontogenic sinusitis ).
Clinical manifestations
Prolonged runny nose, periodic exacerbations of sinusitis, general malaise, headache, constant sinus discharge, and so on. So outwardly nothing special, but it’s constant.
Diagnostics
It is best to use SCT (especially in cases of odontogenic sinusitis, when it is extremely important to determine the condition of the bone tissue, to exclude the presence of purulent inflammation in the area of the apexes of the roots of the teeth, in general, in those areas where the doctor simply cannot look - author's note). In second place is MRI - most often, it is with the help of magnetic resonance therapy that the diagnosis is made: chronic sinusitis, since it is a “by-product” of an MRI study of the brain, which is one of the most frequently prescribed.
What does long-term lack of treatment lead to?
Important: degeneration of mucous tissue is very dangerous, as malignant formations may occur.
Long-term changes in the shape and volume of the mucous membrane of the maxillary sinuses lead to hypertrophy of the maxillary sinuses. The nasal septums shift, and the patient begins to experience serious breathing problems.
In addition, the displacement of the shells disrupts their symmetrical arrangement. Impaired free nasal breathing will negatively affect the condition of the entire body. On performance, sleep status, mental balance, oral health and much more.
Changes in the condition of the nasal turbinates affect the condition of their mucous tissue.
The following happens:
- the asymmetry of the shells provokes uneven air inhalation, the mucous membrane of the shells becomes inflamed;
- when trying to cope with increased loads, the membrane grows, hypertrophy of the mucous membrane of the nasal concha begins;
- secretion increases.
Important: hypertrophic changes in the nasal mucosa can also be provoked by physical impact, trauma to the nose and face.
The purulent stage of the development of the situation is especially dangerous.
Purulent processes in the sinus will have the following symptoms:
- congestion occurs periodically, can be unilateral or bilateral;
- nasal discharge – cloudy, white;
- the jaw, forehead, and sides of the nose hurt;
- the general condition of the patient is rapidly deteriorating;
- the temperature rises.
Vasomotor sinusitis
It develops in people with disorders of the autonomic nervous system and nasal breathing against a background of negative emotions and stress.
Clinical manifestations
Allergic and vasomotor symptoms are manifested by sneezing, difficulty in nasal breathing, and discharge of large amounts of contents from the nose. Most often this is pansinitis.
Diagnostics
In this case, ACMD-Medox can use both SCT and MRI with equal benefit. With classical radiography, there may be options for under- and over-diagnosis associated with the nature of the visualization of pansinuit in the images.
Establishing diagnosis
With the help of rhinoscopy, a preliminary conclusion can be made
The following methods are used to diagnose the disease:
- X-ray examination;
- MRI;
- Rhinoscopy.
The research method is prescribed by the attending physician. Often you have to resort to more than one method. It is especially important during the examination to determine the exact location of mucosal hypertrophy.
Important: it is not possible to cure this disease at home, since a diagnosis can only be made after a series of procedures and consultation with a specialist.
In case of a serious condition of the patient, surgical intervention will be indicated. The video in this article and photos will explain the features of x-ray diagnostics.
X-ray is the main diagnostic method when there is a suspicion of thickening of the mucous membrane of the maxillary sinuses
Surgical methods for treating hypertrophy
Hyperplasia of the mucous membrane of the maxillary sinuses can be cured by certain surgical methods.
Surgical treatment methods:
| Method name | Main tool | How to do it |
| Galvanocaustics | Electrode | It is performed under local anesthesia. The pathological area is cauterized. After the procedure there is a recovery period, the formed scar resolves. Nasal breathing is completely restored. |
| Conchotomy | Wire loop | The technique involves resection of the enlarged mucosa. |
Upon completion of the procedure, the doctor should give detailed instructions about the features of the postoperative period.
In addition to surgical methods, drug support is prescribed:
- antihistamines;
- drugs to strengthen blood vessels;
- rinsing the sinuses and nasal turbinates with medicinal solutions;
- performing inhalations.
For successful treatment, the main thing is to see a doctor on time
Thickening and swelling of the mucous membrane of the maxillary sinuses causes pathological formation of mucus and pus. Pathogenic microorganisms successfully live in such an environment. This proximity is especially dangerous for the membranes of the human brain, which are located near the maxillary sinuses.
This disease cannot be determined independently, which means that even with a simple runny nose you need to consult a specialist. Self-medication in this case gives false hope, wastes precious time, the cost of which is very high, and is harmful to health.
Frontitis (inflammation of the mucous membrane of the frontal sinus)
is an inflammation of the mucous membrane of the frontal sinus. Inflammation occurs due to infection with pathogenic organisms such as viruses, bacteria, and fungi. As a result of inflammation, swelling and blockage of the frontal-nasal tract occurs with purulent contents, which accumulate in the sinus, burst its walls and put pressure on the nerve receptors, which leads to frontal sinusitis.
Symptoms
There are acute and chronic processes of frontal sinusitis.
An acute process occurs most often against the background of influenza, rhinitis, as well as during trauma due to swelling of the mucous membrane and blockage of the frontonasal canal. The acute process is characterized by:
- increase in body temperature to 38 degrees
- sharp pain in the forehead, eyes, with pressure the pain intensifies
- copious nasal discharge (serous or serous-purulent)
- nasal breathing is difficult.
Have you noticed the following symptoms? Make an appointment
If frontal sinusitis is treated incorrectly, or in its absence, the acute process can turn into chronic frontal sinusitis due to insufficient drainage of the frontal sinus.
The chronic process most often occurs when the nasal septum is deviated. With each cold, the risk of frontal sinusitis increases. Chronic frontal sinusitis is marked by more subtle symptoms than in the acute form:
- aching headache
- pain on the affected side of the sinus, worsens with pressure
- purulent nasal discharge with an unpleasant odor, which flows down the nasopharynx during sleep, and in the morning the patient expectors a large amount of sputum.
Causes of the disease
The reasons for the development of frontal sinusitis may be:
- the presence in the body of a chronic source of infection (caries, tonsillitis), bacterial carriage (staphylococcus, streptococcus)
- runny nose
- previous trauma to the nose and, as a consequence, circulatory disorders and swelling of the mucous membrane
- deviated nasal septum
- congenital anomalies of the nasal cavity
- adenoids and polyps - can block the canal between the nasal passage and the paranasal sinus
- past diseases - influenza, ARVI, scarlet fever, diphtheria, rhinitis, sinusitis, sinusitis
- decreased immunity
- chronic diseases of the upper respiratory tract
Diagnostics
After an examination by an ENT doctor, as a rule, an x-ray of the paranasal sinuses is prescribed; in some cases, an ultrasound examination of the frontal sinuses and computed tomography are indicated.
To determine sensitivity to antibiotics, it is necessary to take a general blood test and bacterial culture of nasal discharge.
We recommend that you consult a doctor! 276-00-15
To determine the source of infection, rhinoscopy (examination of the nasal cavity using an endoscopic method) is indicated, with the help of which a possible curvature of the nasal septum can be identified.
Treatment
Treatment of frontal sinusitis is carried out conservatively, in some cases surgical treatment is indicated (for purulent form).
In general, for the treatment of frontal sinusitis, the doctor prescribes vasoconstrictor drugs in the form of drops or sprays; if the process of frontal sinusitis is purulent, broad-spectrum antibiotics are prescribed. Once a tank culture is obtained, treatment may be adjusted depending on sensitivity to antibiotics.
If frontal sinusitis is caused by a viral infection, antiviral therapy is prescribed; for a fungal infection, antifungal drugs are prescribed. Additionally, immunomodulators are prescribed to support the immune system.
doctor
Depending on the severity of the process, rinsing of the paranasal sinuses by moving the fluid may be prescribed. In this case, the medicinal solution is injected into the nasal cavity, the solution passes through the paranasal and frontal sinuses, and comes out with a stream of liquid, washing out the purulent contents and mucus. But if treatment does not improve and the level of pus increases, surgical treatment of frontal sinusitis is indicated.
A modern and effective method of treating frontal sinusitis is the expansion of the frontonasal anastomosis using an endoscope, during which the pus drains abundantly. This procedure is not traumatic and does not maintain a cosmetic effect. The procedure is performed under local anesthesia.
Another method of treating sinusitis without a puncture is the use of the YAMIK sinus catheter, where, when different levels of pressure are created in the paranasal sinuses, pus flows out.
Which method of treating frontal sinusitis will be effective in a particular case can only be decided by a specialist based on the examination and the patient’s symptoms.
Possible complications
Frontitis can lead to intracranial complications: purulent meningitis, brain abscess, which can even cause death.