There are many clinical conditions whose nature and distribution can be clarified by MRI.
To begin with, it is worth saying a few words about the development options, of which the most common are hypoplasia and aplasia of the sinuses.
Hypoplasia of the frontal sinus
Particularly noteworthy is such a development option as excessive pneumatization of the sphenoid sinus and posterior ethmoid cells in the form of developed upper lateral recesses, in the presence of which the internal carotid arteries and optic nerve canals can protrude into their lumen. As a result, during inflammatory processes in the mucous membranes of these sections (including subacute and chronic), a clinical picture of progressive atrophy of the optic nerves may develop. In addition, when performing surgical interventions in this anatomical area, the risk of damage to the carotid arteries and optic nerves increases many times.
Developed superolateral recesses, against which the optic nerves are identified
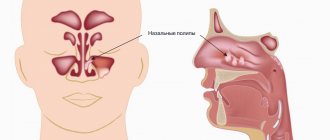
Inflammatory changes in the paranasal sinuses are the most common diseases of the upper respiratory tract. From 5 to 15% of the world's population suffers from various types of sinusitis. In addition, there is a trend towards an increase in chronic forms.
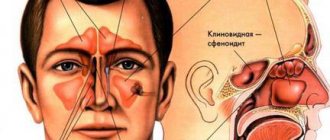
Facial pain with sinusitis is localized in the projection of the affected sinus. With frontal sinusitis and sinusitis, in addition to pain, there is pain on palpation. Ethmoiditis and sphenoiditis are characterized by constant pain in the eye and nose and nasal congestion. Diagnosis of chronic sinusitis is especially difficult. With mucoceles and tumors, swelling and displacement of the eyeball are observed: upward - with damage to the maxillary sinus, outward - with damage to the ethmoidal labyrinth, and downward - with damage to the frontal sinus.
Let's look at examples of pathology of the paranasal sinuses detected during an MRI examination.
Swelling of the mucous membrane of the right maxillary sinus with fluid level
MR picture of polysinusitis with a total disturbance of pneumatization of the cells of the ethmoid bone, moderate, sometimes uneven, local disturbance of pneumatization of the right half of the main sinus and the upper parts of the left maxillary sinus, without an exudative component.
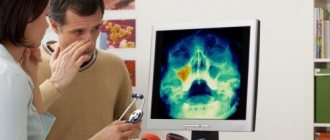
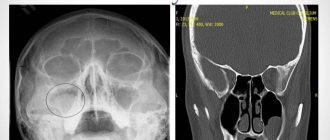
What does a sinus x-ray show?
An x-ray shows the human skull with bone structures, cavities and septa. The method is used at the preparatory stage in surgery.
What can be seen on a sinus x-ray:
- Foreign object in the nasal passages.
- Inflammatory process, thickening of the mucous membrane of the infected area.
- Consequences of injuries to the face and head.
- The presence of exudate (mucous, blood, purulent) in the paranasal and frontal cavities.
- "Airiness" of the sinuses.
- Neoplasms: polyps, tumors, cysts.
- Anomalies in the structure of the facial skeleton.
X-rays help to correct the diagnosis in case of fever or headache of unknown etiology.
Ultrasound in gray scale mode: diagnosis and evaluation of the effectiveness of treatment of maxillary sinusitis
Ultrasound scanner RS80
A benchmark for new standards!
Unparalleled clarity, resolution, ultra-fast data processing, and a comprehensive suite of advanced ultrasound technologies to solve the most challenging diagnostic problems.
Introduction
The incidence of acute bacterial rhinosinusitis in our country tends to increase. Thus, according to the Moscow Department of Health, in the period 2012–2017. the number of patients has increased 1.9 times compared to the previous 15 years, while the number of patients with severe forms of this suffering has increased [1]. Acute rhinosinusitis is one of the most common diseases encountered in outpatient practice. In different countries, its incidence ranges from 15 to 40 episodes per 1000 patients per year, women suffer approximately twice as often as men, and the highest incidence occurs in working age from 25 to 44 years [2].
The presence of facial pain, difficulty in nasal breathing, purulent nasal discharge, impaired sense of smell, and unpleasant odor in the nose are the most common symptoms of sinusitis. The close proximity of the optic, trochlear, oculomotor and abducens nerves can lead to flashing spots before the eyes, impaired convergence, decreased vision, dizziness, nausea and even vomiting. Inadequate or insufficient and untimely therapy often contributes to the transition of acute sinusitis to a chronic form; it becomes recurrent and leads to the development of chronic bronchitis, pneumonia or bronchial asthma. The changing range of pathogens and the development of their resistance to previously used drugs complicate the choice of antibiotic therapy. It is believed that if there is no effect of initial therapy on the 7th day, a repeat diagnostic search should be performed [3].
The existing range of techniques most commonly used for this purpose includes anterior rhinoscopy, endoscopy, ultrasound scanning in A- and B-mode, diagnostic puncture, plain radiography and computed tomography of the paranasal sinuses (SNS). Anterior rhinoscopy, when mucopurulent secretion is detected in the middle nasal meatus, indicates the presence of sinusitis, but the absence of discharge does not exclude a pathological process in the sinuses.
Endoscopy of the nasal cavity allows you to visualize the discharge in the area of the anastomosis of the paranasal sinuses, however, a full endoscopic examination of the nasal cavity can be difficult if there is gross deformation of the nasal septum. Ultrasound scanning in A-mode, due to the difficulty of interpreting the data obtained, often does not allow differentiating a cyst or polyp from mucosal edema and a liquid component.
A diagnostic puncture does not give an idea of the condition of the walls and mucous membrane, the presence of polyps and other formations, although it allows one to obtain the contents of the sinus or prove its absence.
Plain radiography is the main method for diagnosing the paranasal sinuses. The agreement rate between radiography and computed tomography for maxillary sinusitis is 77% [4].
Computed tomography of PPN is the “gold standard” in the diagnosis of sinusitis; it serves as a reliable basis for planning surgical treatment. However, its use for monitoring during conservative treatment is limited due to high cost and radiation exposure.
Ultrasound scanning of the maxillary sinuses in gray scale mode (B-mode) has been used for more than 15 years and not only in cases where it is necessary to exclude exudative sinusitis in a group of people who have contraindications to x-ray examination, but also for monitoring during treatment [5] , however, the frequency of its use is small and does not exceed 4%, while the frequency of use of radiation methods is 87% [2].
To illustrate the capabilities of ultrasound examination of the maxillary sinuses in gray scale mode, we present the following clinical observations in which the study was performed on a modern expert-class ultrasound device. Ultrasound was performed with the patient sitting and facing the examiner using a linear sensor with a frequency of 7.5 MHz in sagittal and horizontal sections; the lower wall of the orbit, which is the upper wall of the maxillary sinus, served as a guide for finding the maxillary (maxillary) sinus.
Clinical observation 1
Patient N., 25 years old, consulted an otolaryngologist with complaints of congestion in the left half of the nose. Ultrasound of the left paranasal sinus in A-mode reveals an expansion of the initial complex (Fig. 1a), in B-mode the posterior wall is not visualized, since the pneumatization of the sinus is preserved, thickening of the mucous membrane up to 15 mm is noted - a picture of left-sided maxillary catarrhal sinusitis (Fig. 1b).
Rice. 1.
Catarrhal maxillary sinusitis.
A)
Echogram of the left maxillary sinus in A-mode.
b)
Echogram of the left maxillary sinus in B-mode.
As is known, catarrhal sinusitis is characterized by swelling of the mucous membrane, cellular infiltration of all its layers with leukocytes, due to which in B-mode a weakly echogenic zone with a clear distal contour appears directly behind the bone base of the anterior wall of the sinus, which, when examined in A-mode, corresponds to an expansion of the initial complex. In this observation, there are no reflections from the posterior wall either during ultrasound in gray scale mode or in A-mode, that is, pneumatization of the sinuses is preserved.
Visualization of the posterior wall is possible only if pneumatization is impaired and depends on the amount of secretion or other contents: the more secretion, the more complete the view of the walls will be. The line of separation of media, which would correspond to the X-ray concept of “liquid level,” is not visible with ultrasound, since the ultrasound beam passes parallel to this line [6]. Consequently, the amount of exudate must be judged by the extent of visualization of the posterior wall in the sagittal section.
Clinical observation 2
Patient V., 40 years old, complained of nasal congestion and pain in the projection of the left maxillary sinus. Ultrasound of the paranasal sinuses on the right shows uniform thickening of the mucous membrane (Fig. 2a), on the left - a violation of pneumatization: the posterior wall is visible to the level of the infraorbital foramen (Fig. 2b). An additional hyperechoic arc is the cyst wall. An X-ray taken on the same day shows a total darkening of the left maxillary sinus; MSCT on the left confirmed the presence of a cyst.
Rice. 2.
Right-sided exudative maxillary sinusitis. Cyst of the right maxillary sinus.
A)
Echogram of the right maxillary sinus in B-mode. Thickened mucous membrane is marked with calipers.
b)
Echogram of the left maxillary sinus in B-mode. Arrows mark the wall of the cyst.
Clinical observation 3
Patient E., 49 years old, complained of nasal congestion, mucous discharge, and discomfort in the zygomatic region. Ultrasound in A-mode in both maxillary sinuses shows a significant expansion of the initial complex and on the right - an additional peak from the posterior wall (Fig. 3a), on the radiograph on the right - subtotal darkening, on the left - parietal thickening of the mucosa (Fig. 3b). Ultrasound in B-mode shows exudate on the right, filling almost the entire volume of the sinus (Fig. 3c), and on the left – parietal thickening of the mucous membrane up to 14 mm (Fig. 3d). There is complete agreement between the results of ultrasound and radiography. After 7 days of conservative treatment, complete restoration of pneumatization on the right was noted (Fig. 3e) and a significant decrease in the thickness of the mucosa on the left (Fig. 3f).
Rice. 3.
Right-sided exudative maxillary sinusitis dynamics before and after treatment.
A)
A-mode echogram of the maxillary sinuses before treatment.
b)
X-ray of the paranasal sinuses before treatment.
V)
Echogram of the right maxillary sinus in B-mode before treatment.
G)
Echogram of the left maxillary sinus in B-mode before treatment.
d)
Echogram of the right maxillary sinus in B-mode after treatment.
e)
Echogram of the left maxillary sinus in B-mode after treatment.
Clinical observation 4
Patient Yu., 36 years old, complained of a feeling of pressure in the area of the right maxillary sinus. Ultrasound (Fig. 4a) shows pneumatization of the right maxillary sinus is preserved, the posterior wall is not visualized, the mucosa is thickened, and the thickening is heterogeneous, with point hyperechoic inclusions. MSCT (Fig. 4b, c) also reveals uneven thickening of the mucosa, with an area of heterogeneous compaction – a fungal body (mycetoma). Dense inclusions represent deposits of phosphate and calcium sulfate in areas of necrosis of mycetoma - a picture of non-invasive fungal sinusitis. The patient was operated on and the diagnosis was confirmed.
Rice. 4.
Non-invasive fungal maxillary sinusitis.
A)
Echogram of the right maxillary sinus in B-mode.
b)
MSCT of the paranasal sinuses. Axial projection.
V)
MSCT of the paranasal sinuses. Frontal projection.
Clinical observation 5
Patient N., 43 years old, complained of difficulty in nasal breathing, mucus running down the back of the throat, discomfort in the left zygomatic region, and headaches. On ultrasound, pneumatization of the right maxillary sinus is preserved; a cyst measuring 11 x 9 mm is visualized in the lower part near the anterior wall (Fig. 5a), the left maxillary sinus is airless (Fig. 5b), the picture resembles exudative sinusitis, but the posterior wall has a double contour, and this sign indicates that this is not a free exudate, but a large cyst, which is confirmed by the results of MSCT (Fig. 5c, d).
Rice. 5.
Maxillary sinus cysts.
A)
Echogram of the right maxillary sinus in B-mode. Arrows mark the wall of the cyst.
b)
Echogram of the left maxillary sinus in B-mode. Arrows mark the wall of the cyst.
V)
MSCT of the paranasal sinuses. Frontal projection.
G)
MSCT of the paranasal sinuses. Axial projection.
Clinical observation 6
Patient K., 38 years old, complained of difficulty in nasal breathing, mucopurulent discharge from the nasal cavity, headache, and low-grade fever. On ultrasound, the pneumatization of the right maxillary sinus is disrupted, the posterior wall is visible, which has a single contour in contrast to the previous observation, and near the anterior wall there is an additional arch, which is the wall of the cyst (Fig. 6a). The presence of exudative sinusitis was confirmed x-ray: the right maxillary sinus is completely darkened (Fig. 6b). Despite the treatment, after 4 days, no dynamics were noted on ultrasound, which served as the basis for a puncture, during which purulent discharge was obtained, the sinus was washed with a dioxidine solution. As a result, during control ultrasound 2 days later, pneumatization of the sinus was restored, the posterior wall was not visible, and a small cyst remained near the anterior wall (Fig. 6c).
Rice. 6.
Right-sided exudative maxillary sinusitis. Treatment control.
A)
Echogram of the right maxillary sinus in B-mode before treatment. Sagittal projection.
b)
X-ray of the paranasal sinuses before treatment.
V)
Echogram of the right maxillary sinus in B-mode after treatment. Axial projection.
Clinical observation 7
Patient B., 28 years old, complained of difficulty in nasal breathing, mucopurulent discharge from the nose, headache, and was treated with vasoconstrictor drugs for a week and a half. It is known that he suffers from chronic sinusitis with exacerbations 1-2 times a year. On the radiograph (Fig. 7a) in the right maxillary sinus there is a pronounced thickening of the mucosa, in the left - against the background of parietal thickening of the mucosa, the level of fluid is determined up to 1/3 of the volume of the sinus; the same words can be used to describe the ultrasound picture (Fig. 7b, c). Antibiotics and topical corticosteroids were prescribed. After 4 days, the ultrasound picture was without the slightest dynamics (Fig. 7d), and therefore the sinus was punctured, washed and filled with dioxidine (Fig. 7d): it is transparent to ultrasound and makes it possible to examine in detail the thickened mucosa - uniform along the anterior wall and in the form several polyps along the posterior wall.
Rice. 7.
Polypous polysinusitis. Treatment control.
A)
X-ray of the paranasal sinuses before treatment.
b)
Echogram of the left maxillary sinus in B-mode before treatment. Sagittal projection.
V)
Echogram of the left maxillary sinus in B-mode before treatment. Axial projection.
G)
B-mode echogram of the left maxillary sinus 4 days after the start of treatment. Axial projection.
d)
Echogram of the left maxillary sinus filled with dioxidine solution in B-mode 4 days from the start of treatment. Sagittal projection.
e)
B-mode echogram of the left maxillary sinus 8 days after the start of treatment. Sagittal projection.
and)
Echogram of the left maxillary sinus in B-mode 15 days from the start of treatment. Sagittal projection.
h)
B-mode echogram of the left maxillary sinus 36 days after the start of treatment. Sagittal projection.
And)
MSCT of the paranasal sinuses. Axial projection.
To)
Echogram of the right maxillary sinus in B-mode after 2 years. Sagittal projection.
l)
B-mode echogram of the left maxillary sinus after 2 years. Sagittal projection.
After another 4 days (8th day from the start of treatment), against the background of ongoing therapy, the ultrasound picture is completely restored: the sinus is again filled with heterogeneous contents (Fig. 7f), and only after another week the amount of content decreases, pneumatization is partially restored (Fig. 7g) . However, after 3 weeks the original picture completely returned (Fig. 7h), MSCT confirmed the presence of polyposis polysinusitis (Fig. 7i), the patient underwent surgical treatment and has been feeling well for two years. After 2 years, during pregnancy, nasal congestion reappeared; an ultrasound scan on the 2nd day of illness revealed bilateral exudative maxillary sinusitis (Fig. 7j, l); the sinuses were washed through the anastomosis formed during surgical treatment; a large amount of thick viscous mucus was obtained; treatment: Aqua-Maris, Nasonex, irrigation therapy, intranasal glucocorticosteroids (mometazole). Thanks to timely actions, stable remission was quickly achieved.
Conclusion
The sensitivity of ultrasound for impaired pneumatization is 100%. In determining its cause, be it swelling of the mucous membrane, the presence of exudate, cysts or polyps, ultrasound naturally cannot compete with computed tomography. For swelling of the mucous membrane, the sensitivity of ultrasound is 82.3%, the specificity is 66.7%, for cysts - 66.7 and 33.0%, for polyps - 90.9 and 62.5%, respectively [7]. But a comparative analysis of the information content of plain radiography and ultrasound diagnostics showed the absence of statistically significant differences between them [8], that is, the otolaryngologist has the right to expect from ultrasound the same information as from plain radiography, with the only difference being that ultrasound also provides multiple, quick, harmless, visual and objective assessment of the effectiveness of treatment. The desire to comply with the principles of evidence-based medicine dictates the need for more widespread use of ultrasound of the paranasal sinuses in outpatient practice.
Literature
- Kozlov V.S., Gorbunov S.A., Kudryashov S.E. Analysis of experience in the use of nasal catheters in acute bacterial rhinosinusitis // Bulletin of Otorhinolaryngology. 2020; 85 (6): 46–51.
- Savlevich E.L., Kozlov V.S., Farikov S.E. Analysis of modern schemes for the diagnosis and treatment of acute rhinosinusitis according to the outpatient service of polyclinics of the Administration of the President of the Russian Federation // Bulletin of Otorhinolaryngology. 2020; 85 (4): 51–57.
- Gurov A.V., Zakarieva A.N. Possibilities of modern macrolides in the treatment of acute purulent sinusitis // Consilium medicum. 2010: 12 (3): 31–35.
- Ryazantsev S.V., Karneeva O.V., Garashchenko T.I., Gurov A.V., Svistushkin V.M., Sapova K.I., Kazanova A.V., Maksimova E.A. Acute sinusitis. Clinical guidelines of the National Medical Association of Otolaryngologists. M., 2016. 30 p.
- Shilenkova V.V., Kozlov V.S., Byrikhina V.V. Two-dimensional ultrasound diagnostics of the paranasal sinuses: A manual. Yaroslavl, 2006. 54 p.
- Vasilchenko S.A., Sergeeva T.A., Valitova L.N., Khabarova E.G., Burkov S.G. Ultrasound visualization of the maxillary sinuses: experience of use for sinusitis in an outpatient setting // Kremlin Medicine. 2012; 1:65–68.
- Byrikhina V.V. Two-dimensional ultrasound diagnosis of diseases of the paranasal sinuses: Abstract of thesis. dis. ...cand. honey. Sci. M., 2007.
- Shilenkova V.V., Byrikhina V.V., Karpov V.A., Shargin V.V., Korsun A.A. Comparative analysis of the information content of two-dimensional ultrasonography in the diagnosis of paranasal sinuses in adults and children // Russian Otorhinolaryngology. 2005; 1 (14): 129–132.
Ultrasound scanner RS80
A benchmark for new standards!
Unparalleled clarity, resolution, ultra-fast data processing, and a comprehensive suite of advanced ultrasound technologies to solve the most challenging diagnostic problems.
How is a sinus x-ray performed?
The procedure is not painful and does not require preparation. Receive a referral at an appointment with an otolaryngologist, infectious disease specialist or surgeon.
How to do a sinus x-ray:
- The patient removes metal jewelry, glasses, and dentures.
- To protect against radiation, he wears a lead apron or vest with a collar.
- The laboratory assistant indicates how to position yourself correctly relative to the apparatus. Depending on the required projections, the position is changed at the command of a specialist.
- While taking the photo, you should not move and hold your breath.
- After development and decoding, the film with the description is given to the patient.
The conclusion is not considered a final diagnosis, but provides clarifying information for the treating specialist.
Darkening of the sinuses on x-ray
The method is based on the different permeability of hard and soft tissues by electromagnetic waves. Bones block radiation and appear white in the picture. Specialists are interested in blackouts, which determine the nature of the disorder.
Darkening of the sinuses on an x-ray indicates fluid accumulation. This is a sign of inflammation with the release of mucous or purulent secretion. Sometimes, the picture shows thickening of the walls of the mucous membrane lining the sinuses.
New growths stand out as clear dark spots with shadows. Polyps look like peas on a “pedicle”, and cysts have a cavity filled with fluid inside.
conclusions
1. High-tech methods of radiological diagnostics (MSCT or CBCT) are a necessary component of the complex diagnosis of HFRS.
2. The use of computed tomography (MSCT or CBCT) makes it possible to determine the cause of AHF and, thus, choose the correct tactics for patient management.
3. MSCT or CBCT should be recommended to patients before and after endodontic treatment of teeth and dental implantation, as well as during surgical interventions on the upper jaw in order to timely identify possible pathological changes in the maxillary sinuses (including asymptomatic ones).
Conflict of interest: The authors of the article have confirmed that they have no financial support/conflict of interest to report.
X-ray of the sinuses during pregnancy
The radiation dose during the study is 20 μSv and is considered safe even when performed repeatedly for an adult. The fetus is susceptible to ionizing radiation, which causes intrauterine developmental defects. Carrying a child is a contraindication to the procedure.
X-rays of the nasal sinuses during pregnancy and breastfeeding are done exclusively for health reasons. The potential benefit of the research must outweigh the harm to the child. After the procedure, a pregnant woman needs an ultrasound of the fetus, and a nursing woman needs to transfer the baby to artificial nutrition for a day.
The harm of self-medication
The most obvious harm of self-medication is the lack of positive results. People often take medications until they feel better. However, this approach is wrong. Antibacterial drugs should be taken only as prescribed by a doctor. Strictly in the volumes and within the time frame that he announced at the reception. Otherwise, the symptoms will go away, but the source of infection will remain. Inflammation in the maxillary sinus will become chronic.
Or, if the drugs were chosen incorrectly, there may be no improvement at all. The disease will become advanced, the pain due to overcrowded sinuses will become unbearable, and inflammation will have a chance to spread to the organs and tissues closest to the sinuses, causing all sorts of complications.
Another risk of self-medication is the medications that must be taken for sinusitis. If the dosage is incorrect, taken too often, or if there are problems with internal organs, antibacterial drugs can do more harm than good. Cases of drug-induced liver damage from uncontrolled use of antibiotics are not so rare. What can we say about gastrointestinal tract disorders, dysbacteriosis, and so on.
X-ray of the sinuses for children
Pediatricians try to protect preschool children from the harm caused by X-ray radiation to the fragile skeletal system. The procedure is allowed to be performed on patients over 7 years of age.
Before this period, a clear justification for the importance of intervention is necessary - for example, severe facial trauma or severe sinusitis with a risk of inflammation of the meninges.
It is difficult for a young child to sit or stand still during an x-ray. To distract him, they use toys, sedatives, and in emergency cases, anesthesia. At an older age, you can captivate your child with a game in which you should freeze for a short time.
Sign up for the study
Treatment
In the process of treating chronic maxillary sinusitis, it is necessary to restore the drainage and ventilation function, remove pathogenic discharge and stimulate recovery processes. To achieve success, broad-spectrum antibiotics (amoxicillin, augmentin, panclave, etc.), anti-inflammatory drugs, vasoconstrictor nasal drops, antihistamines, puncture of the maxillary sinuses to clean rinsing water, or rinsing the paranasal sinuses by moving fluid (vacuum) are prescribed. drainage). If the effect of the prescribed treatment does not occur within a week, treatment should be continued up to surgery in the ENT department of the hospital.
If the rinsing water during puncture of the maxillary sinus is white, dark brown or black, a fungal infection can be suspected. In this case, it is necessary to discontinue antibiotics and carry out antifungal treatment. If you suspect the anaerobic nature of the process, which is characterized by an unpleasant odor of the discharge, a negative result in bacteriological examination of the contents, oxygenation (a high-pressure oxygen treatment method) of the sinus lumen should be carried out.
If long-term drainage is necessary, you need to install a drainage in the sinus and rinse it through it daily (up to 3 times a day). In case of severe local pain, which is confirmed by X-ray examination, and the ineffectiveness of conservative treatment within 3 days, as well as if signs of complications appear, immediate referral to an ENT hospital is indicated to carry out surgical debridement.