Normally, a person grows 52 teeth over a lifetime: 20 milk teeth and 32 permanent teeth. Supernumerary teeth are “extra” dental units that appear in addition to some incisors, canines, premolars or molars. In various medical sources, the phenomenon is called hyperdontia, supradontia or polyodontia. A superset can include 1–2 teeth or reach several hundred dystopic structures, be true or false.
Supernumerary teeth: causes of anomaly
The main cause of polyodontia is a violation of the formation or development of tooth germs. Doctors are considering several theories for this phenomenon:
- Heredity – hyperdontia develops as a result of genetic abnormalities that can be transmitted from parents to children. In this case, the pathology should manifest itself in the patient’s closest blood relatives.
- Splitting of the root germ of the tooth in the embryonic period of development. Usually observed after the mother becomes ill during pregnancy. Characteristic of single supernumerary teeth (1–2 pcs.).
- Failure during the embryonic period of tooth formation with the formation of multiple dental buds (up to several hundred). It is observed when the mother lives in unfavorable environmental conditions, during treatment with dangerous drugs, taking drugs, or alcohol abuse.
In more rare cases, polyodontia develops as a result of odontoma, a benign tumor in the area of the jaw arches. The disease is typical for children and young people during the period of active growth of tooth germs. Such a tumor structure may contain several tens or even hundreds of highly deformed dentin-enamel formations.
Provoking factors in the prenatal period:
- malfunction of genes - primarily the Msx1 gene (responsible for the formation of tooth germs);
- viral infections;
- taking teratogenic and potentially dangerous drugs;
- smoking, drug use, alcohol use;
- poor environmental conditions;
- exposure to radiation - not only direct exposure, but also increased general background radiation in the place of residence/work.
Reference! Some scientists consider the presence of supernumerary teeth as an atavism. Thus, it has been scientifically proven that various species of the genus Homo could boast a set of teeth of 36–44 pieces. However, this theory does not explain in any way the appearance of multiple rudiments covering all spaces of the sky (a typical example is an Indian boy who had to remove 230 supernumerary units).
Symptoms of pathology
The main symptom is the presence of teeth beyond the natural set. They can have different positions, shapes and numbers. The process of teething of abnormal teeth is often accompanied by pain, fever, and inflammation of areas of the oral cavity. If measures are not taken in a timely manner, complications may develop:
- redness and swelling at the site of the impacted tooth;
- problems with chewing food and digestion;
- injuries to the mucous tissues of the oral cavity;
- violation of the position of the main teeth (dystopia) and the formation of malocclusion;
- various speech defects - mainly problems with the pronunciation of hissing sounds;
- loosening of adjacent normal teeth;
- deformation of the jaw bones.
In young children and adults, the pathology has its own nuances. They are associated with age-related characteristics of the body and affect the subsequent development of maxillofacial structures. Statistics on the spread of pathology in children and adults:
- 60% of cases are children and adolescents during the period of replacement of milk teeth with permanent ones;
- 35% of cases are adults;
- 5% of cases are small children during the period of growth of baby teeth.
Reference! Supernumerary teeth, as a rule, have a standard structure, sometimes with a smaller crown size. Less common are deformed formations of a teardrop-shaped, lumpy, chisel-shaped form.
Introduction
The eruption of primary teeth in children is a natural and physiological process. However, in some cases it may be accompanied by numerous unpleasant symptoms, such as fever, loss of appetite, child anxiety, sleep disturbances and indigestion.
Anatomical and physiological features of the maxillofacial region of children
Considering the anatomical and physiological features of the maxillofacial region of children in the process of teething, it should be noted that the nature of the changes will depend on the age of the child. A newborn has no teeth in the oral cavity.
During this period, the mucous membrane covering the edge of the alveolar process forms a dense cushion over it. The oral mucosa in newborns has a similar structure in all parts. Subsequently, differences appear in the structure of various parts of the oral mucosa.
The gums of infants also differ in structure from the gums of adults: the connective tissue is more delicate, there is less elastic tissue, and a greater number of cellular elements. At the end of the child's first year of life, there is a noticeable increase in elastic tissue in the gums. In the soft tissues surrounding the tooth before eruption, slight hyperemia is noted [1].
Mechanism of teething
The eruption of a tooth is one of the links in the chain of processes of its development, which begins in the prenatal (in utero) period and continues for several years after eruption. This process is associated with the growth and development of the child’s entire body.
Teeth are considered erupted when they reach the occlusal surface, i.e. contact with the teeth of the opposite jaw. In this case, part of the enamel in the cervical area remains under the gum.
The mechanism of eruption is quite complex. By the time the tooth erupts, atrophy and resorption of the area of bone covering the crown of the tooth occurs. Similar processes occur in the gums. When a tooth erupts, simultaneously with the resorption of bone tissue in some areas, its formation occurs in others. During root growth, processes of bone restructuring also take place, and a gradual deepening of the dental alveoli occurs.
During teething, morphological changes occur in the teeth and surrounding tissues. There is an increase in blood supply, a change in vascular permeability, an increase in the production of the basic substance of the pulp and periodontium, and atrophic changes in the gums over developing teeth occur [2].
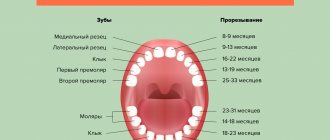
Physiological teething
Physiological teething is characterized by three main features: certain timing, pairing and sequence of eruption [3]. Temporary teeth begin to erupt in a child at an average of 6–7 months. The generally accepted timing of teething, presented by Kronfeld (see table) [4].
However, when analyzing the literature data, it can be stated that the timing of tooth formation, eruption, formation and resorption of roots is individual for each child, therefore different authors indicate different timing in their studies.
In addition, the data vary depending on the region of residence of the child: for example, in the northern regions of Russia there is a more frequent deviation from the average timing of teething towards later teething [6].
The eruption of primary teeth is influenced by many factors, and sometimes even a combination of them. Studies have shown that the eruption of primary teeth in young children is most strongly influenced by the mother’s chronic diseases, the presence of bad habits, diseases during pregnancy, gestosis and diseases of the child in the first year of life [5].
Pathology of eruption of primary teeth
The pathology of the eruption of primary teeth can include early, late and difficult eruption. Violation of the pairing and sequence of eruption of primary teeth also refers to the pathology of eruption.
Earlier eruption of baby teeth may adversely affect the resistance of their tissues to the action of negative factors. When teething in a child at the age of 3 months after birth, due to imperfect structure and insufficient mineralization of hard tissues, lack of hygienic care, earlier damage to temporary teeth by caries is possible.
Particular attention should be paid to pre-erupted primary teeth. Most often these are the lower central incisors, very rarely - the upper ones. The structure of teeth that erupted in utero is defective; their roots have not yet finished forming. Such temporary teeth can lead to complications for both the mother and the child. When sucking, the teeth injure the mother's nipple, which often causes mastitis. Such teeth should be removed soon after eruption. There is currently no generally accepted explanation for the reasons for such premature eruption [7].
A significant delay in the onset of teething may indicate a violation of the child’s physical development, some kind of metabolic disorder or a general somatic disease.
Violation of the timing, pairing and sequence of eruption of primary teeth can serve as a marker of various diseases, for example, rickets, endocrine disorders, hypothyroidism. Research has shown that the eruption of primary teeth in the group of children with rickets begins on average 3.5 months later when compared with healthy children; a violation of the sequence of eruption of temporary teeth is observed in 52.31% of children with rickets; a violation of paired eruption is observed in 35 .38% [5].
Teething in children with different constitutional types has its own distinctive characteristics. For example, in infants with a lymphatic-hypoplastic type of constitution, which is characterized by lymphadenopathy, excess body weight, delayed static-motor development, more often than in children with other types of constitution, late eruption of primary teeth, severe anxiety, crying, and disturbances are observed. character of the stool, more pronounced swelling and soreness of the gums, profuse salivation. In children with a neuro-arthritic type of constitution, which is based on an increase in the synthesis of uric acid, accompanied by manifestations of sympathicotonia, teething is timely, but occurs with severe pain in the gum area, high fever, the smell of acetone from the mouth, increased regurgitation up to fountain vomiting, increased excitability. In infants with exudative-catarrhal (allergic) type of constitution, teething also occurs within the prescribed time frame, but is more often accompanied by the addition of a respiratory viral infection and exacerbation of atopic dermatitis [8].
The eruption of primary teeth is a natural physiological process that usually does not cause any significant changes in the health of children. However, a number of children develop a symptom complex that, according to the International Classification of Diseases (ICD), is classified as teething syndrome (ICD code - K00.7).
Often, respiratory viral, intestinal infections, dysbiosis, and urinary tract infections can be hidden under the guise of teething. Thus, teething syndrome is more of a diagnosis of exclusion and is made only after other pathological conditions have been excluded.
Symptoms of difficult teething in a child are divided into two groups: general and local. General symptoms - anxiety, moodiness, decreased appetite or even refusal to eat, excessive salivation, low-grade fever - are non-specific and may indicate not only teething, but also another disease. The appearance of cough against the background of teething is caused by hypersalivation and saliva entering the upper respiratory tract. Loose stools are also associated with increased salivation and increased bowel movements. Local symptoms - swelling and redness of the gums at the site of the future tooth, pain on palpation of the eruption site - accurately indicate teething [9, 10].
The most common undesirable manifestations of teething include increased salivation, swelling and soreness of the gums, behavioral disturbances in the child, an increase in body temperature to subfebrile levels with the possible addition of rhinitis, and decreased appetite [11].
Therapy methods
Today, there are pharmacological and non-pharmacological methods of therapy for the eruption of primary teeth [12].
To reduce the severity of pathological symptoms of teething in infants, various medications are used. They can be of general and local action.
In cases of severe pain and fever, non-steroidal anti-inflammatory drugs (NSAIDs) are used, which reduce body temperature and have a systemic analgesic effect.
In order to relieve the main symptoms of teething - agitation, anxiety, increased temperature due to teething, as well as relieving pain and swelling of the mucous membrane, the drug Dantinorm-Baby is used, which includes chamomile (reduces irritability, temperature), laccone (used for pain and inflammation of the gums) and rhubarb (digestion is stabilized).
Dantinorm-Baby has an innovative dosage form - the only sterile solution for oral administration in individual dosage containers.
Dantinorm-Baby is produced in France using the most modern blow-fill-seal technology (“Blow-Fill-Seal” - BFS). It is a single process in which a single machine forms a container and aseptically fills it with a single dose of sterile solution in a very short time. Speed and extremely high safety standards are two advantages of this process: sealed, ready-to-use monodoses of the drug in just 12 seconds. Each dose of Dantinorm-Baby is ideal for children, as it ensures sterility, dosing accuracy and hygiene for non-contact use. Unlike dental gels, the duration of action of 1 dose of this drug is ~ 8 hours. Thus, just 3 doses per day of the dosed solution provide continuous protection against teething symptoms 24 hours a day [13].
The drug contains only natural ingredients, so it can be used in children from birth.
To relieve local symptoms of the eruption of primary teeth in children, various gels are used. Any teething gel usually has a local effect and cannot provide long-term pain relief. It is recommended to use such gels no more than 5–6 times a day to avoid the development of side effects, incl. allergic. The main goal when prescribing a gel for teething is to reduce the intensity of pain and prevent the inflammatory process on the gum mucosa.
Gels with an anesthetic effect containing lidocaine or benzocaine increase the risk of allergic reactions. Studies have shown that the gels contact the gums for a short time, then the child swallows it. This time is not enough for pain relief, however, with frequent use, the child swallows too much gel, which can lead to seizures, severe brain damage, and heart problems. Gels containing choline salicylate exhibit effects associated with aspirin and may cause Reye's syndrome in susceptible children [14].
Non-pharmacological methods of treating symptoms of eruption of primary teeth include a simple and accessible method - massage of the gingival ridges. When pressing on them, the pain syndrome decreases. For massage you can use special silicone brushes. Cool gel or silicone teethers reduce swelling, also reducing pain.
Conclusion
Thus, teething in many children is accompanied by a number of nonspecific syndromes and is a diagnosis excluding other pathological conditions. It is necessary to familiarize parents with this problem and introduce the safest, preferably natural, drugs that help alleviate the pain of this condition in children.
Features of polyodontia in children
Possible symptoms of hyperdontia in childhood:
- intrauterine formation of teeth (a child is born with several teeth);
- the appearance of teeth in the first months, weeks and even days of life;
- delayed eruption of baby teeth.
This has unpleasant consequences:
- problems with feeding the baby - he does not latch onto the nipple well and sucks weakly;
- swelling of the mucous tissues can spread to the nasal area and cause breathing problems;
- poor closure of the dental arches causes severe salivation;
- a prolonged increase in temperature to 38C is possible.
Hyperdontia is especially harmful during the period of speech formation. Teeth located outside the general row prevent the tongue from taking the correct position when pronouncing most consonant sounds. Without eliminating the pathology, any speech therapist will be powerless.
In addition to true hyperdontia, children (less often adults) can develop the so-called false form of the disease. It is characteristic of the period of tooth change and develops during the eruption of molars next to the milk teeth that have not yet fallen out. This is a fairly common phenomenon that usually goes away on its own as the dentition finally forms. In some cases, orthodontic treatment may be required.
Features of polyodontia in adults and adolescents
In adults, after complete replacement of complete teeth, the presence of additional units can lead to additional pathologies:
- chronic rhinitis, sinusitis when the wall of the maxillary sinuses is perforated by the roots of supernumerary impacted structures;
- interdental caries - due to teeth fitting too closely to each other.
Retention and dystopia
Adults are characterized by 2 main types of supernumerary teeth:
- Dystopic teeth are the name given to teeth with deviations in the direction of growth. The peculiarities of the formation of supernumerary units very often lead to dystopia. This is due to the fact that the space on the dental arch line is limited, and the roots of normal teeth simply push the “intruder” towards the cheek or palate.
- Impacted teeth – impaction occurs when a tooth loses its growth impulse and remains embedded in the jawbone. Impacted teeth can cause the adjacent normal teeth to become loose and cause them to shift and change the bite. Often cause pain.
On a note! According to statistics, hyperdontia accounts for up to 2% of cases of dental problems. Of these, 70% are associated with the appearance of single supernumerary teeth, 25% with a couple of such formations, and only in 5% complex multiple complexes of 3–4 or more teeth can be found.
Diagnostic methods
The main indication for diagnosis is the presence of an “extra” tooth in the patient’s oral cavity or obvious signs of its eruption (painful tubercle or swelling in the gum or palate). All of these signs can be identified through a routine visual examination, during which the dentist evaluates the condition of the oral cavity. To confirm the diagnosis and carry out differential diagnosis, an X-ray examination is performed - an orthopantomogram. If it is necessary to examine the dentition in several planes, computed tomography (CT) is additionally prescribed.
On a note! The patient may not be aware of the presence of impacted supernumerary teeth. In this case, hyperdontia is detected only by the results of an X-ray or CT scan of the maxillofacial region.
Dystopic wisdom tooth: what is it?
A dystopic wisdom tooth is a third molar, also known as a “figure eight”, which is positioned incorrectly relative to the rest of the dentition. Such a tooth almost always needs to be removed.
A special case of a dystopic wisdom tooth is an unerupted, but fully formed figure eight, which turns out to be turned parallel to the gum. In this case, the tooth is there, although it is not visible, and it is in an incorrect position, so we can talk about dystopia.
Two examples of dental dystopia
Do supernumerary teeth need to be removed?
There is no clear answer to the question of what to do with “extra” teeth. Much depends on the shape, position and quantity. The following are subject to mandatory removal:
- baby teeth that interfere with normal growth and formation of permanent teeth;
- strongly dystopic structures - located on the palate or at a large angle to the lateral side of the gums;
- impacted formations that put pressure on the adjacent roots of normal teeth and provoke periodic inflammatory processes of soft tissues.
If the additional tooth does not cause discomfort and does not disrupt the development of the dentition, removal may not be necessary. Moreover, such a superset can play the role of a strategic reserve in case of damage to nearby normal teeth.
How does the removal work?
The removal procedure can be simple or complex. In the first case, the doctor is dealing with a fully erupted tooth, the root of which is not intertwined with the surrounding structures. Simple removal steps:
- The oral cavity is prepared - treated with antiseptics, anesthesia is given.
- Grasp the crown with forceps (in some cases, an additional incision of the mucous tissue is required to facilitate access).
- The elevator destroys the retaining ligaments.
- The root is freed and the tooth is removed.
- Clean the hole from tooth fragments and bones.
- Apply stitches (if necessary) and a healing bandage.
Complex extraction is prescribed in the case of impacted, semi-impacted or dystopic teeth with complex root shapes. The procedure is carried out with a deep incision of soft tissues, in especially severe cases - with opening of the jaw bone to gain access to the roots. The latter option is relevant for deep bone occurrence, position in close proximity to the cranial sinuses and orbits, as well as for irregularly shaped roots and a high risk of damage to complete teeth. A complex removal operation is performed by a dental surgeon.
Classification of injuries to children's teeth
The nature and severity of the damage is determined based on a comprehensive examination of the patient using radiological, clinical and other methods. To make a diagnosis, dentists today use different systems for diagnosing trauma to children’s teeth.
Standard ELLIS classification
This system of dividing acute injuries into separate types, developed by Ellis, is the very first and most used in practice. It includes 9 categories of dental damage:
- I – slight fracture of the crown within the tooth enamel;
- II – moderate crown fracture extending into enamel and dentin;
- III – severe fracture of the crown with exposure of the pulp;
- IV – loss of pulp viability in the presence/absence of a crown fracture;
- V – complete dislocation of the injured tooth;
- VI – damage with root fracture;
- VII – slight subluxation of an injured tooth;
- VIII – fracture of the crown in the cervical area;
- IX – trauma to baby teeth.
Types of Traumatic Injuries WHO
Actively used in modern dentistry along with ELLIS. This classification was developed based on the Andresen system and includes, in addition to dental injuries, damage to other tissues (oral mucosa, gums, periodontal tissue, bones).
I. Damage to pulp and hard tissue:
- cracks in tooth enamel (A);
- fracture of the crown without opening the pulp (enamel affected - B, enamel and dentin affected - C);
- fracture of the dental crown exposing the pulp (D);
- combined root and crown fracture with pulp exposure (E);
- trauma with root fracture (F).
II. Periodontal damage:
- shock of the tooth with a weak response of periodontal tissue to percussion without increasing its mobility and displacement (A);
- subluxation with change in mobility without displacement (B);
- penetration of the injured tooth deep into the tissues (C);
- exit of the tooth from the anatomical socket (D);
- displacement in a direction other than axial (E);
- complete dislocation of the injured tooth (F).
III. Bone injury:
- tight connection of the tooth with the socket with penetration deep into the tissue (A);
- fracture of the wall of the anatomical recess (B);
- fracture of the alveolar bone tissue (C, D);
- fracture of the jaw bone (upper – E, lower – F).
IV. Injury to the gums and oral mucosa:
- acute soft tissue injury (A);
- bruise of the mucous membrane or gums (B);
- soft tissue detachment (C).
Classification of injuries to children's teeth according to ICD-C
This is an international system for defining acute injuries, based on ICD-10 (1997). Used in pediatric dentistry to classify various injuries, including fractures of primary and permanent teeth (S02.5):
- fracture (chip) within the thickness of the enamel (S02.50);
- fracture of the dental crown without injury to the pulp (S02.51);
- crown fracture with injury extending to the pulp (S02.52);
- fracture of the root part of a permanent tooth (S02.53);
- double fracture in the area of the dental crown and root (S02.54);
- multiple fractures of different locations (S02.57);
- unspecified fracture of primary or permanent tooth (S02.59).
Orthodontic treatment
Depending on the situation, it is used after tooth extraction or instead of it. In children, it is used to stimulate the loss of baby teeth and eliminate false hyperdontia, as well as to facilitate and accelerate the eruption of a normal set. In addition, orthodontic treatment with the installation of braces, mouth guards, dental plates or other auxiliary structures can straighten crooked teeth and return them to their proper place.
Before prescribing treatment, the dentist carefully evaluates the condition of the complete and supernumerary structures and, depending on the overall picture and prognosis for the future, can use both formations or leave the strongest and most durable tooth (not necessarily complete).
Procedure for providing assistance to children with dental damage
Immediately after receiving an injury, the patient is provided with primary medical care, which includes a general assessment of the child’s condition, pain relief, prescription of antibiotics, anesthetics and other medications, as well as a preliminary diagnosis. After this, the patient’s parents are given a recommendation to make an appointment with a pediatric dentist (therapist), who will carry out full dental treatment. The doctor providing specialized care carries out:
- registration of a medical history (including legal and social aspects of the case);
- collecting anamnesis (origin of injury, presence of concussion, local symptoms);
- clinical examination of the injury (visual examination, percussion, palpation, temperature tests of the pulp, instrumental methods);
- additional diagnostics (electroodontodiagnostics (EDD), transillumination, targeted radiography, occlusal radiography, computed tomography);
- making a diagnosis based on examination, clinical and other studies;
- choice of treatment tactics taking into account the nature of the damage, possible risks, benefits and costs.
The period of rehabilitation of a child after an injury, starting from the moment of emergency assistance, can take 1-3 or more days. Given the complexity of treatment, the period of complete restoration of the integrity and functions of damaged teeth often takes a longer period - several months or even years.