Author of the article:
Soldatova Lyudmila Nikolaevna
Candidate of Medical Sciences, Professor of the Department of Clinical Dentistry of the St. Petersburg Medical and Social Institute, Chief Physician of the Alfa-Dent Dental Clinic, St. Petersburg
Gum disease is one of the most common phenomena in dentistry. The leading places among them are occupied by periodontitis, inflammation of the gum pocket, and loose gums.
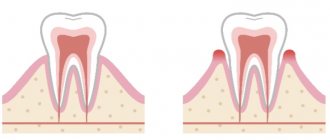
In a healthy state, the gum fits tightly to the tooth. The permissible peeling depth is about three millimeters. This condition is not critical and is even normal; in this case, the pocket easily cleans itself of bacteria and small food particles. It is enough to brush your teeth in a timely manner. However, if the situation develops unfavorably, the pocket expands and becomes deeper. Plaque and food debris accumulate inside, and it becomes impossible to get rid of them with a toothbrush.
Sediments become a breeding ground for bacteria, which provoke further development of the disease.
You should be wary if you notice the following symptoms:
- Bleeding gums;
- Tissue swelling;
- Redness around the teeth;
- Painful sensations when brushing teeth;
- Bad breath;
- Tartar deposits and the appearance of soft plaque.
Formation of a pocket in the gum can lead to serious problems. In later stages, exposure of the necks of the teeth develops. Pathogenic organisms penetrate deep into the tissues, affecting bone tissue and roots, which leads to tooth loss.
Causes of gum pockets
The main reason for gum detachment from a tooth is poor oral hygiene. Incompletely cleaned plaque lingers on the enamel, hardens and forms a stone. This, as well as uncleaned food debris, contributes to the active proliferation of bacteria. They penetrate into the formed hood and gradually lead to an inflammatory process.
Some other factors may also influence the development of the disease:
- Inappropriate hygiene products (too hard toothbrush, aggressive toothpaste);
- Smoking;
- Lack of vitamins;
- Excessive consumption of sweets;
- The presence of certain chronic diseases.
Treatment of gum pocket inflammation
In the early stages and with timely treatment, the disease is easily treatable. You should not try to cure yourself with the help of widely advertised toothpastes or mouth rinses. Only a specialist can prescribe adequate therapy after conducting the necessary research. As a rule, they include:
- Initial examination;
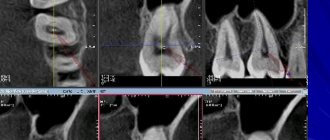
- Taking panoramic x-rays that show all the teeth at once, as well as the depth of tissue damage. This will allow you to choose the right treatment method.
- If necessary, a comprehensive examination for the presence of chronic diseases;
- Making a diagnosis and developing a plan for further action.
As a rule, gum inflammation is treated in several stages. This is a process that requires not only the professionalism of a dental specialist, but also the active participation of the patient himself.
Stage 1. Removing dental plaque
It is plaque and tartar that are sources of bacteria. Therefore, they need to be removed first. This may require several procedures, depending on the extent of the damage to the teeth.
At this stage, special attention is paid to cleaning the gum pockets. It is very important to remove stone and plaque from this area as it is the most difficult to reach at home. In addition, gum pockets “open” the way for bacteria to reach the deep tissues of the tooth.
Stage 2. Anti-inflammatory therapy
This stage is started only when dental plaque is completely removed. The dentist rinses the gum pockets with special antiseptic solutions and applies a gel that relieves inflammation.
In addition, home therapy is prescribed: rinsing with antiseptics and special gels. The patient performs this treatment independently twice a day for the time specified by the doctor.
Stage 3. Recommendations for oral hygiene
Without the patient's compliance with this point, a successfully treated disease may develop again. At this stage, the dentist should tell you which toothbrush and what teeth cleaning products you can use, as well as explain the rules for caring for your teeth.
Brushing your teeth is done with short and gentle rotational movements. Try to reach even hard-to-reach areas. It is convenient to carry out the procedure in the following sequence:
- Cleaning the outside of teeth, both front and back. The top and bottom rows are cleaned separately.
- Cleaning the inside of teeth. Pay special attention to the outermost chewing teeth in the upper and lower rows.
- Cleaning chewing surfaces.
- Cleansing the tongue, including at the root. This is where a huge number of bacteria accumulate, which can easily migrate to the gums and teeth. Plus, cleaning your tongue keeps your breath fresh.
Prevention of gum pocket inflammation
Following simple recommendations will prevent the development of periodontitis and relapses.
Use of specialized therapeutic and prophylactic toothpastes. Due to their special composition, they ensure hygienic cleanliness of teeth and protection of gums from inflammation. Asepta Sensitive toothpaste has this effect. It contains calendula extract and protects teeth well from bacteria. In combination with it, it is recommended to use Asepta gum gel. It contains propolis, known for its healing properties.
Carefully monitor oral hygiene. It's not enough to just brush your teeth. You should also use mouthwash regularly. The Asepta mouthwash has a good effect. It freshens breath, relieves inflammation and pain, and has an antibacterial effect. In addition, it is necessary to use dental floss after each meal to thoroughly clean the interdental space.
Eat more raw apples, carrots, and cucumbers. This food promotes gum massage and natural teeth cleaning.
Regularly undergo preventive examinations at the dentist, at least twice a year.
What parents need to do
- Parents must demonstrate that teeth should be brushed on all sides;
- Move the brush from the gum to the edge of the tooth. For the first teeth, you need to choose a special children's toothpaste and a brush with soft bristles. Teeth cleaning gel is best.
- There is no need to choose toothpaste with excessive fluoride content. While brushing teeth, the child involuntarily swallows the toothpaste, and fluoride can cause irreparable harm to the child’s body.
By the age of 3, children have already mastered the technique of brushing their teeth well, but parents should always be present when brushing their baby’s teeth.
Between the ages of 5 and 12 years, a child's molars begin to erupt. At this time, the enamel on the teeth begins to mature, so you can already use toothpaste containing fluoride.
Parents have the opinion that damaged baby teeth do not need to be treated, because they will fall out anyway. This is an erroneous opinion and caries that appears on baby teeth must be cured.
Life cycle of teeth
Almost all the organs of our body are formed in the womb. Teeth are no exception. Already at the age of 6 weeks, the rudiments of the first teeth appear in the fetus: 10 pieces each. on the upper and lower jaw. Total - 20 small “buds”. This is the future milk bite.
See an interesting infographic about what kind of life our teeth live, and immediately after - in more detail about each stage and useful tips on how to preserve your teeth until old age.
Life cycle of teeth
| Birth | A child is born with fully formed tooth buds - they are located just under the surface of the gums. It is also interesting that some babies are already born with one or more teeth |
| 2-3 months | The baby begins to cut his first teeth. This is a rather unpleasant process, which is accompanied by excessive salivation, pain, deterioration of the child’s mood, and refusal to eat. In addition, during teething, local immunity is significantly reduced, which increases the risk of developing a viral infection. This explains the frequent increase in temperature during this period. |
| 6-14 months | Teeth begin to appear. The lower incisors grow first, then the upper ones. In total, the child should grow 20 pieces, including 2 multi-root chewing ones on each side - this will be the milk bite |
| 6-7 years | At this time, “baby” teeth begin to fall out. There is a change from a milk bite to a permanent one |
| 12-13 years old | The period of complete completion of the formation of a permanent dentition. By this age, the milky ones should fall out completely, and permanent ones should grow in their place. Helping teeth fall out in most situations is not required - this is a natural and physiological process that does not require third-party intervention. But it’s still worth seeing a doctor: it’s important to monitor both the wound and the process as a whole |
| 17-21 years old | During this period, “wisdom teeth” – the furthest ones in the row – may grow. There are 4 of them in total. There were no dairy predecessors in their place, so they have to pave the way on their own. In addition, they grow at a time when the bone tissue is fully formed and very hard. That is why their growth is associated with such problems as pain, acute inflammation of the mucous membrane, incorrect position in the row and even retention (the tooth does not erupt, forms and remains completely in the bone tissue) |
| 20 years and older | Starting at this age (and if there are problems with the body or when playing dangerous sports, even earlier), we begin to lose teeth. In the absence or poor hygiene, with poor nutrition, and the appearance of diseases of many organs and systems of the body, the enamel becomes weaker and is subject to attack by bacteria. With age, the amount of saliva decreases - and it is this that is a natural means of cleansing plaque. This is largely why teeth and gums become more susceptible to decay. It is also worth remembering that not only dental diseases, but also problems with gums lead to loss. |
Clinical picture
The main symptom for all types of flux is severe toothache at the site of infection, sometimes diffuse (with extensive bone damage). Swelling gradually begins to increase: first it is localized above the site of inflammation, and then along the surrounding tissues, sometimes affecting the neck, temple and eye.
Important! Sometimes flux occurs painlessly or with a mild pain effect, which, as a rule, indicates the development of a chronic form with sluggish inflammation and periodic relapses.
Inflammation is accompanied by the following symptoms:
- pulsation at the site of the lesion;
- increase in body temperature to subfebrile and febrile levels;
- headache;
- enlarged lymph nodes on the affected side;
- weakness, lethargy, lack of appetite;
- pain when swallowing, talking, opening the mouth;
- pain when pressing on the gum;
- redness of the oral mucosa at the site of the lesion.
What happens if you don't treat a dental cyst?
The formation does not manifest itself clinically for a long time. The progression of the disease leads to discomfort in the pathological area (especially when chewing food). Over time, a tubercle forms on the surface of the gum near the root area, which gradually increases. The mucous membrane changes color and swelling appears.
When the process suppurates, a person experiences symptoms of inflammation and intoxication: hyperthermia, headache, toothache, chills, tachycardia. A fistula may form in the middle of the protrusion, from which the contents of the cavity are released.
If you do not start treating cystic formation in a timely manner, serious complications may develop:
- phlegmon;
- lymphadenitis of nearby lymph nodes;
- inflammation of the maxillary sinuses;
- periostitis (spread of infection to the periosteum);
- osteomyelitis;
- abscess;
- deformation of the dentition;
- blood poisoning.
Why are the first teeth called baby teeth?
There are several opinions on this matter. Doctors attribute the authorship of the term to Hippocrates, who believed that these teeth are formed from mother's milk. Philologist N.N. Vashkevich states that “the term is a tracing from the Latin lactose “milk”. But the tracing paper is false, it is a misunderstood Arabic liwaqt - “for a while,” “temporary.”
One way or another, the first teeth actually actively “feed” on breast milk, since it is from it that the child absorbs the main building material of teeth and bones – calcium. And although baby teeth erupt, as a rule, at 6-7 months, their formation in the child’s jaws occurs long before that.
It is worth noting that for the health and strength of the first teeth, it is mother’s milk (not cow’s) that is necessary, since the nutrients from it are maximally absorbed by the baby’s body. Therefore, the universal recipe “breastfeed your baby” will help in this matter.
Eruption pathologies
What parents should be wary of when primary or permanent dental elements appear:
- delay in the eruption of the first teeth by 2 - 3 months. This may be a sign of the absence of primordia or a genetic predisposition;
- abnormally early dates. Possible disruptions in the functioning of the endocrine system;
- excessively dark enamel color. May be a consequence of chronic diseases or high iron levels in the blood;
- pathology of the bite or incorrect vector of tooth growth (rotation, tilt, displacement to the side). These signs indicate deformations of the dental system.
Interesting Facts
Enamel color
The natural color of enamel can be absolutely anything and it is extremely rare that it is snow-white. As a rule, the enamel is slightly yellowish or grayish. In children, teeth may even have a bluish tint, which indicates the presence of a large pulp and its close location to the enamel
About a child's first teeth
Some babies may be born with one or even more teeth, which form in the womb. It also doesn’t matter the age when the baby’s first teeth appear – at three or ten months. The main thing is that, in general, the milk bite is formed completely and correctly.
About the important role of baby teeth
Milk teeth serve primarily as the basis for permanent ones - they literally pave the way for them. If the first teeth grow straight, it is not at all necessary that the subsequent ones will grow as well. However, the opposite situation is also possible, so the formation and growth of all teeth should be monitored under the supervision of the attending physician.
About wisdom teeth
Wisdom teeth may not erupt – this is a completely normal and fairly common occurrence. Whether to remove or leave grown ones depends on their condition: if they only bring discomfort, in the presence of caries or pulpitis it is extremely difficult to cure them, it is quite possible to sacrifice such teeth, since they do not bear any functional load
About oral hygiene
According to statistics, only 57% of women and 46% of men cleanse twice a day. The rest periodically skip such an important procedure, which allows you to effectively cope with plaque and thereby protect the enamel and gums from attack by harmful bacteria.
About using dental floss
According to research, today only 50% of the population flosses daily. Meanwhile, this is an excellent way to prevent many dental diseases: it is the floss that effectively cleans the interdental spaces from food debris and plaque. Today, the only alternative to thread can be an irrigator - a brush cannot cope with such narrow spaces
How to treat a dental cyst
If a cyst appears in a tooth, what should you do? At the first signs of pathology, you should seek help from a doctor. The specialist will listen to complaints, conduct an examination of the oral cavity, and refer you for an X-ray examination. Treatment tactics depend on the extent of the inflammatory process.
Conservative methods
Therapeutic treatment of the disease is permissible in the initial stages, when the size of the cavity does not exceed 5 - 8 mm. Another prerequisite is good patency of the root canal, under which the cyst is located. General scheme of therapeutic treatment:
- Hard tooth tissues are prepared.
- Expand the entrances to the canal.
- The pulp is removed.
- Expand the lumen of the canal.
- Antiseptic and medicinal treatment of cavities is carried out.
- Temporary filling with dental paste, which accelerates the restoration of damaged tissue.
Treatment is long-term, taking from several months to 1 - 2 years. The patient periodically visits the doctor for follow-up examinations and repeated medicinal treatments. To suppress the growth of bacterial flora, a course of antibiotic therapy is usually prescribed. If control X-rays confirm the success of treatment, then a permanent filling is installed.
Surgical intervention
The operation is performed if the tooth formation is large, located in a hard-to-reach place, therapeutic treatment has not given a positive result, etc. Invasive intervention can be carried out according to different protocols
Cystectomy
Operation cystectomy - removal of the tumor along with the damaged root segment. This is a tooth-saving procedure. It is performed in the presence of a small tumor (extending no more than 2 teeth). How to remove a cyst on the root of a tooth:
- administration of local anesthetic;
- cut the gum above the formation;
- gain access to the capsule;
- remove the tumor;
- in case of union with the root, resection of its apex is performed;
- a bone-restoring drug is placed inside the resulting cavity;
- stitches are placed.
In the postoperative period, the patient is prescribed drug therapy.
Hemisection
Used on multi-rooted teeth. During the intervention, the destroyed root is amputated along with part of the crown and the capsule is removed. The cavity is filled with a polymer composition, the upper part is expanded with a composite material or prosthetic crown.
Cystotomy
The operation consists of resection of the anterior wall of the cyst. The contents of the capsule are pumped out through the formed hole, which eliminates internal pressure. This leads to a gradual reduction of the cavity. The manipulation is low-traumatic, but requires careful postoperative care.
Tooth extraction
Tooth-preserving operations cannot be used in all cases. In some clinical situations, it becomes necessary to remove a tooth. Indications for such a decision may include:
- significant size of education;
- the presence of an extensive zone of bone destruction around the segment;
- tumor growth into the maxillary sinus;
- other methods did not work.
After surgical treatment, the doctor gives recommendations on oral care in the postoperative period. If you ignore the dentist's advice, after removal of a dental cyst, adverse consequences are possible: wound infection, bleeding, relapse.
Characteristic age-related changes during growth
Eruption of the crown means that it becomes vulnerable to external factors, which include both pathogenic bacteria and mechanical stress. The enamel and dentin layers undergo the first changes - studies show that the height of teeth decreases by an average of 0.035 mm every year, which is caused by the wearing off of the protective coating. A more intense decline is a pathological sign, as well as a consequence of the abuse of bad habits.
With age, the natural shade and structure of the enamel coating changes. Cracks and chips form, coloring pigments accumulate, and areas are formed through which plaque containing pathogenic microorganisms penetrates into the fabric. It is worth noting that the human body does not have a mechanism for regenerating tooth enamel, so any damage requires a medical examination and, if necessary, comprehensive treatment that eliminates negative consequences.
Age-related changes in the pulp
Aging also affects the internal structure of teeth. A reduction in pulp volume, as well as the formation of fibrous deposits, leads to the accumulation of minerals that worsen the condition of the internal vessels and capillaries that provide nutrition to the element. Among patients in the older age group, pulpal atherosclerosis is often diagnosed, which results in fragility and vulnerability of the teeth.
Changes in bone and gum tissue
Another characteristic sign of age-related changes is a decrease in the density of the bone tissue structure, expressed in a reduction in height, as well as the manifestation of excessive mobility of elements of the dentition. Jaw osteoporosis is considered a common pathology, affecting patients over 50 years of age. In addition, weakening of bone tissue leads to adentia - tooth loss - which results in incorrect distribution of the chewing load, leading to atrophy.
Negative processes also affect the soft tissues of the oral cavity. Gum recession, as a rule, is the result of the development of periodontal pathologies, genetic predisposition, non-compliance with medical recommendations and the presence of bad habits. Ultimately, age-related changes lead to complete tooth loss, requiring surgical dental treatment. At the same time, premature adentia can be avoided by regular visits to the doctor, which include preventive and physiotherapeutic procedures, as well as the restoration of individual lost or destroyed units.
When do baby teeth appear?
The rudiments of baby teeth appear in the embryo at about 5-7 weeks of pregnancy. By the time a child is born, the crowns of 10 temporary and 8 permanent teeth have already been formed in his jaws. The timing of the eruption of baby teeth is quite arbitrary. The average formula is as follows: the child’s age in months minus 6. That is, the first 2 teeth (usually the lower middle incisors) appear at 6-7 months, the next 2 (upper middle incisors) at 8-9 months. Next, the upper lateral incisors usually come out, then the lower lateral incisors, then the front molars, canines, and back molars. Thus, by the age of 2-2.5 years, the child should have all 20 milk teeth. These are ideal timing and ideal sequence; deviations from them are quite common. Teeth may begin to appear as early as 4 months, or may linger for up to 8-9 months. In rare cases, a baby is born with teeth already erupted.
If your little one doesn’t “meet the deadline,” don’t be alarmed. This does not mean that the child is developmentally delayed. You should also not be proud of the early appearance of teeth - it does not indicate the child’s superpowers. Early or late appearance of teeth may be a hereditary factor. In case of a strong deviation from the schedule - the appearance of teeth before 4 months or their absence after 9 months - just show the baby to the pediatric dentist. In general, the first examination by a pediatric dentist should be scheduled at least when the child is one year old. The doctor will see how the teething process is progressing and talk with you about the baby’s oral hygiene. The baby will get acquainted with the environment of the office, with the doctor, will get the first positive experience of visiting the dentist, because nothing unpleasant awaits him during this visit, and funny pictures on the walls of the clinic, toys, a chair in which he can ride with his mother - all this will certainly have an impact on him. him a good impression. From now on, you should take your child to the pediatric dentist at least twice a year.
What is a dental cyst (root cyst)
A cyst on the root of a tooth is a tumor-like formation surrounded by a dense fibrous membrane consisting of stratified mucous epithelium. The internal space of the sac is filled with serous or purulent fluid. The size of the cavity can vary widely: from 0.1 to 3 cm. Cysts less than 5 mm are called granulomas.
The most common location of dislocation is the area of the apex of the tooth root. Therefore, such cavities are called radicular (“radix” - root). They can be located near the entrance to the root canal, between the roots, or at the top under the crown. Other localization areas:
- near the alveoli of the frontal segments;
- under the third molars (wisdom teeth);
- inside the maxillary sinus.
A cyst in a tooth can have different origins. According to this feature, the following types of formations are distinguished:
| Variety | Description |
| Radicular | Found in the area of the apex of the roots of any tooth. The main reason is the destruction of osteocytes due to advanced caries and pulpitis. |
| Follicular (pericoronal) | Benign tumor of non-inflammatory origin. Occurs in the area of transition between enamel and cement. Formed from the tooth germ due to disruption of eruption. |
| Periodontal | A congenital dental cyst formed from remnants of the epithelium of the dental plate. Most often localized in the premolar area. |
| Retromolar | Formed as a result of carious inflammation or abnormal eruption of the eighth segment |
| Residual | Appears due to incorrect extraction of the dental unit and poor revision of the alveoli. |
| Primordial (keratocyst) | Develops from epithelial cells of the enamel organ. Capable of keratinization. Localized in the corner of the lower jaw, near the lower premolars. |