A wisdom tooth is the 8th tooth in a row (figure eight) or 3rd molar, its eruption period is 17-25 years. This is a large molar, often with a complex root system. The peculiarities of its development and growth in most cases become the cause of various dental problems. Although the structure of the figure eight is characterized as an ordinary molar, its chewing function is practically absent. If a wisdom tooth hurts, it is rarely preserved. The figure eight is destroyed early, often erupts with a carious lesion, grows at an angle or in a horizontal position.
Why can wisdom teeth hurt?
Currently, dentists consider the third molar to be a vestigial organ, which in the process of evolution has lost its functional load and relevance. For ancient man, it served to chew hard food, which is practically absent in the modern diet, which means there is no longer any need to use the wisdom tooth when chewing. This fact is supported by the presence of approximately 10% of the planet's population, whose representatives do not have eights at all, which is not a pathology. The remaining 90% of the population faces unpleasant wisdom tooth problems. The third molar can hurt and bother you for various reasons.
When teething
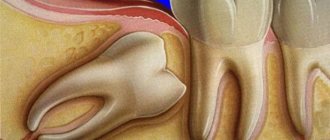
By the age of 18–25, a person’s jaw is already formed. And, naturally, when a wisdom tooth is cut, it may simply not have enough space in the dentition. The eight begins to put pressure on the seven in front, which in turn puts pressure on the sixth molar, etc. As a result, the entire jaw hurts and “aches.”
Often the third molar does not find a place for itself in the dentition and begins to grow dystopically - it deviates to the side, turns around its axis, moves forward or backward. In this case, the gums near the wisdom tooth hurt and inflammation may occur. Not to mention the fact that in adulthood the gums have a fairly dense structure, the resistance of which must be overcome by the figure eight. And in order to erupt safely, it literally tears the soft tissue. Naturally, this process is accompanied by pain and discomfort.
For dental disease
An already formed wisdom tooth will hurt if it is susceptible to any disease. The most common are caries, pulpitis and periodontitis.
- Caries is a pathological process that leads to the destruction of hard tooth tissues, which is initially accompanied by increased sensitivity of the enamel, and subsequently severe pain in the wisdom tooth.
- Pulpitis - inflammation of the internal tissue of the figure eight (pulp) is a consequence of untreated caries. In rare cases, infection enters the pulp through the apical foramen, which may be due to improper position of the molar. With pulpitis, the wisdom tooth hurts very much, since the pulp is penetrated by a large number of nerve endings.
- Periodontitis - inflammation of the periodontium (connective tissue surrounding the tooth) can be caused by injury to the gums or infection during the eruption of the figure eight. In this case, localized, constant pain is observed, which gradually increases and becomes pulsating, which indicates a purulent course of the process.
Important! If an already erupted wisdom tooth suddenly begins to hurt, then you need to show it to the dentist as soon as possible. Timely diagnosis will avoid infection of the pulp, periodontium and the development of complications.
For pericoronitis
Pericoronitis - inflammation of the soft tissue of the gums surrounding the erupting figure eight, is the most common. The problem is that when a wisdom tooth comes in, it first cuts through the mucous membrane with its tubercles, forming a so-called “hood” above itself - part of the gum. Thus, partly the third molar is already visible, and partly is still covered by the “hood” of the gums. Hanging over the figure eight, it creates favorable conditions for the accumulation of food particles, plaque, and microbes, which, sooner or later, leads to inflammation. The development of pericoronitis will also be accompanied by pain.
Important! If the gum above the wisdom tooth forms a “hood” and is inflamed, then it must be excised (removed). The procedure is carried out in the sterile conditions of a dental clinic.
How long will the cutting and toothache last?
The process of cutting through the figure eight is long and highly individual. In some patients it “appears” in 3–4 months, in others it may take 1–2 years, and in others it remains incompletely erupted. Quite often, a wave-like “appearance” of the third molar is observed - either it is intensively cut, or it freezes.
As for severe pain, as a rule, it is present only at the beginning of the process - at the stage when the figure eight cuts through the dense gum tissue. And again, this moment can happen quite quickly or drag on for a long time.
When the first signs of figure eight eruption appear, it is better not to postpone a visit to the doctor. Even if the process does not cause severe pain or discomfort, it is better to show it to the dentist. An experienced specialist will examine the condition of the third molar and provide assistance that will facilitate the process of “the birth of the tooth.”
Signs of inflammation
Inflammatory reactions at the base of the third molar manifest themselves as follows:
- aching or sharp pain;
- an increase in the volume of soft tissues (they seem to increase in size, become taller);
- redness of the mucous membrane;
- swelling of the cheek;
- unit mobility;
- discomfort when pressing;
- enlarged cervical lymph nodes;
- bleeding, bad breath;
- pulsation and burning in the mouth on the affected side;
- the formation of fistulas through which pus and bloody exudate come out;
- hyperthermia of the inflamed area.
Often there are no accompanying symptoms. Then the patient complains only of discomfort at the base of the figure eight.
How to understand that a wisdom tooth is cutting?
It's not difficult to understand. Normally, this process is accompanied by discomfort, engorgement and slight swelling of the gums in the place where the tooth is cut. At the moment of eruption, increased salivation, a feeling of fullness and tolerable pain will be observed. They can intensify during eating and hygiene procedures. Visually and by touching the tongue, you can see and feel the protruding tubercles of the figure eight.
In the pathological course of the process, the following symptoms may join the above-described symptoms.
- Redness and swelling of the gums indicate inflammation of the “hood”.
- It hurts to open your mouth - the inflammation process is progressing and has spread to the masticatory muscle.
- It hurts to swallow - a symptom indicates the presence of purulent inflammation of the soft tissues closer to the tongue.
- High temperature - the inflammatory process progresses.
- The third molar, the adjacent tooth and gums are very painful - most likely, the figure eight is growing in the wrong direction.
Additionally, symptoms may occur depending on the location of the wisdom tooth.
- The upper eights can erupt towards the cheek and injure its mucous membrane, causing pain.
- The lower molars often form a “hood” and grow with an inclination towards the seven, forming a gap. It is difficult to clean with a brush. Over time, a stable plaque and tartar form in it, which leads to the development of caries.
You should not trust various kinds of myths, they say, the appearance of a wisdom tooth is always excruciatingly painful, very problematic and you just need to endure it. It is not true! Normally, the process does not cause excruciating pain and passes with tolerable discomfort. On the contrary, problem eights hurt a lot, provoking the development of inflammation and complications. Therefore, it is better not to delay visiting the dentist.
What to do at home
If your gums are swollen and painful, and you cannot visit a doctor in the near future, you should try to reduce the inflammation and relieve the pain. For this purpose it is permissible to use:
- pain medication or NSAIDs, which can be found at the pharmacy;
- anti-inflammatory dental gel (it’s good if it contains an antibiotic);
- rinse solution with antiseptic effect.
If the pain is associated with a removable denture, then it is advisable to remove it. It is important to understand that painkillers and anti-inflammatory drugs should never be taken every day. Their use should be regarded as a “one-time action” when you can’t bear the pain, and you can only see a doctor tomorrow.
It is unacceptable to use oral antibiotics to “silence” inflammation without medical advice. These are systemic drugs with a large number of side effects. Only a doctor can prescribe them during an in-person examination.
Does it make sense to treat wisdom teeth?
An experienced and self-respecting dentist will always fight for every tooth to the last. And wisdom teeth in this case are no exception. After all, no one knows how the patient’s life will turn out in the future. Perhaps in the future he will need prosthetics, and the figure eight will be used as a supporting tooth for installing a prosthesis. Therefore, if the appearance of a third molar does not pose a threat to neighboring teeth and oral health, the dentist will take actions aimed at facilitating the process and preserving the tooth. Well, unless, of course, the patient insists on its removal.
If the current situation is serious, then removal of the wisdom tooth is inevitable. Including in those cases when the figure eight does not hurt much (or does not hurt at all), but is covered with caries and is gradually destroyed. It is more rational and safer to remove such a tooth and forget about the problems.
When do you need to see a dentist urgently?
Contacting a dentist is required in the following cases.
- Pericoronitis
– the “hood” will be excised. - The figure eight puts pressure on neighboring teeth
- it needs to be removed. - Initial caries
– treatment will be carried out. - Medium, deep caries or rotten tooth
- a clear removal of the figure eight. - The wisdom tooth is loose
- a diagnosis of its condition will be carried out, according to the results of which the molar will be treated or removed. - Pulpitis
– if the root canals are passable, they will be filled.
This list should also include the above symptoms of pathological teething - pain when opening the mouth, swallowing, high temperature. If they appear, you should contact your dentist immediately, since this is a serious inflammatory process, the localization of which requires adequate treatment.
The reason for contacting a specialist may also be the “normal behavior” of the number eight. In this case, the doctor will simply make a small incision on the gum, thereby facilitating the eruption of the wisdom tooth. After a simple procedure, the process will be less painful, and the incision site will heal quickly, after pain for 2 to 4 days.
Recovery after surgery
The removal of the figure eight itself is painless, since it is performed under anesthesia. But due to injury to the gums and bone socket, after the anesthetic wears off, the figure eight, or rather the periodontal tissues, hurt for several days. Painful sensations after a simple removal usually go away within 2-3 days, after a complex one they can persist for about a week. On days 2-3, swelling increases, which subsides after 2 days and the pain subsides. After the intervention, the doctor gives recommendations regarding care, nutrition, lifestyle, and prescribes drug therapy - antibiotics, painkillers, anti-inflammatory drugs, antihistamines.
When should a tooth be removed?
Direct indications for wisdom tooth removal are the following pathologies and conditions.
- There is no place in the dentition for a number eight.
- Dystopic tooth (molar occupies an anatomically incorrect position).
- The appearance of wisdom teeth threatens the molars in front.
- Severe forms of caries that destroy the tooth.
- The third degree of mobility of the figure eight.
- Upcoming installation of braces.
If removal is not carried out, the development of complications is inevitable. The number eight will destroy adjacent teeth and provoke the development of pulpitis, periodontitis, and extensive caries. Eventually it will fall out on its own, but at too great a cost to the patient.
There is no need to be afraid of wisdom tooth removal. Depending on the complexity of the problem, third molar extraction will last from 20 minutes to 2 hours. The operation is performed using local anesthesia or sedation, which ensures that the procedure is painless.
Treatment
The treatment regimen depends on the degree of inflammation and the severity of the disease. It includes the use of:
- solutions and gels for applications;
- antiseptic compositions for rinsing;
- antibiotics;
- vasodilators.
If it’s all about the hormonal background, then it must be put in order. This process is long. Therefore, in parallel, to relieve painful symptoms, the patient can use local anti-inflammatory gels.
If caries is to blame, then urgent treatment at the dentist’s office is indicated. Often, a carious cavity in the crown of the figure eight is regarded as an indication for its removal. This is due to the difficult-to-reach location of the unit and the inability to carry out full treatment.
For pericoronitis, therapy is simple if a person consults a doctor at the first symptoms of the disease. Then antibiotics are prescribed to neutralize inflammation. If pus begins to accumulate in the tissues, the patient suffers from symptoms of general intoxication, and a simple dental operation is performed. The dental surgeon cuts the gum under local anesthesia, rinses the cavity from pus and exudate and installs a drainage tube to drain the accumulated masses. The hood covering the molar is excised so that nothing prevents the unit from erupting completely.
How to relieve pain?
When visiting the clinic, the attending physician gives valuable recommendations that will help relieve the process of the “appearance” of the figure eight. If you decide to act on your own, you can use the following medicines and folk remedies.
Pills and medicines
- Tablets: “Nimesil”, “Analgin”, “Solpadein”, “Tempalgin”, “Ketanov”, “Paracetamol”, “Ibuprofen” are used according to the instructions.
- Gels and ointments: “Cholisal”, “Kamistad”, “Kalgel”, “Metrogil Denta” are applied to the site of tooth eruption.
- Solutions: “Chlorhexidine”, “Miramistin” and “Furacilin” are used for antiseptic treatment of the oral cavity.
Folk remedies
- Soda, saline or soda-salt solution - 1 teaspoon of product for 1 glass of warm water, stir until completely dissolved, rinse the problem area every 2 - 3 hours.
- Sage, calendula, plantain, St. John's wort - to prepare a decoction, pour 1 tablespoon of the product into 1 glass of boiling water, leave for 20 - 30 minutes, use for rinsing every 2 - 3 hours.
Home methods of pain relief will be effective if there are no serious problems with the eruption of the figure eight. If inflammation occurs, the tooth is rotten or very loose, then they will not help, but will only aggravate the problem, which will lead to the development of complications.
Wisdom teeth removal with 20% discount
Moscow
Diagnostics
Any pathology associated with the problematic eruption of one or more wisdom teeth should always be investigated through x-ray diagnostics. To determine the position of the tooth in the jaw (inclination, shape, configuration, structure, how it grows), an orthopantomogram is used.
OPTG is a high-quality panoramic image of all teeth on both jaws. Another diagnostic method that will help you understand why your wisdom tooth hurts is visiography.
Where can the pain go?
Quite often, the process of growth of eights is accompanied by uncharacteristic symptoms. Moreover, some of them are due to the growth of the molar itself, and the other part indicates the development of complications. Let's take a closer look - can a wisdom tooth give into...?
- Head
- in case of complicated teething it can. - Eye
– with complicated eruption of the upper molars and the development of an abscess, it can. - Tongue
- a symptom indicates the presence of purulent inflammation of the soft tissues closer to the tongue. - Ear
– indicates the development of inflammation, pulpitis or dental cyst. - Throat
- most likely we are talking about pulpitis. - Jaw
- a symptom characteristic of complicated teething and inflammation. - The neck
is unlikely, unless we are talking about the spread of infection and inflammation of the lymph nodes. - Temple
– Clicking and pain in the temple may be present due to tension in the temporomandibular joint, which occurs from constant pain. - The teeth are nearby
- of course, because the figure eight can put pressure on them.
Important! The above list is a serious signal to contact a dentist. Don't delay your visit to the clinic!