Indications for local injection anesthesia
Most dental treatment is performed under local anesthesia.
It is mandatory to use:
- Removing a nerve from a tooth
- Gum operations – gum plastic surgery, deep periodontal cleaning – curettage and others.
- Installation of orthopedic structures on living teeth.
- Removal of any teeth and roots, as well as oral surgery
During minor interventions, such as the treatment of superficial caries, some patients can easily do without any anesthesia at all.
There are also types of treatments in dentistry for which anesthesia is not usually given, but there are people with increased sensitivity and a low pain threshold who may need it.
- Teeth cleaning by a hygienist
- Artistic restoration without preparation
- Making removable dentures - at the stage of taking impressions, anesthesia is sometimes given to people with an increased gag reflex
In pediatric dentistry, there is no need to rush with anesthesia - the sensitivity of the internal tooth tissue - dentin - is less pronounced in children than in adults. Therefore, first you need to try to prepare the tooth without an injection - and give anesthesia only at the request of the child. After all, many children are afraid of an injection more than anything else, and after it they may simply refuse to open their mouth again.
Sedation in pediatric dentistry
The risk of developing dental phobia or fear of dentists is increased in childhood. This should be taken into account when choosing an anesthetic. In some cases, it is better to additionally use a mask type of sedation, when the child, in addition to pain relief, also noticeably calms down, can sit quietly for 30-40 minutes or more, and does not experience strong fear and anxiety.
The place where the anesthetic is injected is pre-frozen. This prevents children from developing fear of the injection itself. In the future, the child will not be afraid of dental treatment, even the most complex and lengthy.
Contraindications to local injection anesthesia
- Allergic reactions to anesthetic
- Severe fear of dental treatment
- Mental disorders
- The child’s age is too young (usually under 3 years old)
- Lack of effect from drug administration
Cost of anesthetics and anesthesia
The cost of one carpule of anesthetic is approximately 10-20 UAH. Carrying out one anesthesia in a dental clinic will cost an average of 130 UAH.
What to do if you are afraid of anesthesia
Many people are afraid of injections, because each person has their own pain sensitivity threshold. During anesthesia, the pain from the injection may depend on the professionalism of the doctor, the anesthesia technique, and also on the speed of administration of the anesthetic. An experienced doctor does not save time and administers painkillers for at least 40 seconds. Immediately before the injection, you can ask the doctor to treat the area of the upcoming injection with an anesthetic spray (for example, Lidocaine spray).
Types of local anesthesia
- Application anesthesia
Typically, topical anesthesia is used as the first stage - its essence is that a lidocaine-based gel or liquid is applied to the mucous membrane, which penetrates well through the surface layers and causes numbness. Most often, thanks to it, they achieve dulling of sensitivity for a more painless injection.
Sometimes it can be used as an independent method of pain relief - for example, to remove a baby tooth that is supported only by a thin strip of gum.
Preparations for topical anesthesia are made with a pleasant smell and taste - this makes it easier for patients to accept the treatment.
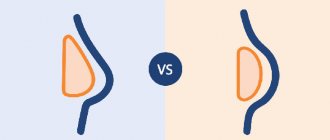
- Infiltration anesthesia
Infiltration anesthesia is a type of local anesthesia that spreads to 2-3 adjacent teeth and is currently the most popular method of anesthesia.
During the injection, our doctor creates an anesthetic depot in the projection of the root of the tooth that is going to be treated. The anesthetic penetrates into the bone within a couple of minutes and blocks the transmission of nerve impulses in the injection area. If a single-rooted tooth is being treated, then one injection is given from the side of the cheek, but if the tooth is multi-rooted, an injection is often added from the palatal side.
This is why infiltration anesthesia is more effective on the upper jaw than on the lower jaw - the bone of the upper jaw is more spongy and allows the solution to pass through more easily.
This method of anesthesia is not recommended for purulent foci of inflammation - it is not effective enough in this environment and at the same time brings more pain. When treating purulent inflammations, it is better to use conduction anesthesia.
- Conduction anesthesia
Conduction anesthesia in dentistry is one of the most effective methods of anesthesia. With this option, it is not small nerve endings that are blocked, but larger nerve trunks. Due to this, it is not the area of 2-3 adjacent teeth that becomes numb, but half of the jaw and adjacent tissues.
Types of conduction anesthesia: palatal anesthesia, tuberal anesthesia, infraorbital anesthesia, incisive anesthesia - these are subtypes for the upper jaw.
For the lower jaw, conduction anesthesia is divided into: mental anesthesia, mandibular anesthesia and torus anesthesia.
- Intraosseous
It is most often used during extraction and involves administering an anesthetic under pressure directly into the bone tissue between the roots of the teeth. The effect of intraosseous anesthesia does not last long, since a very small amount of the drug is injected. But the action comes almost instantly.
- Intraligamentary
With this type of anesthesia, the drug is injected into the space between the tooth and the bone. Since there is little space there, a very small amount of anesthetic is injected, and the numbness will last up to half an hour. Thanks to this, you can treat several teeth at once in one visit.
- Intracanal anesthesia
When a nerve is removed, there is often residual pain even after intraligamentary anesthesia. Then our doctor injects the anesthetic directly into the nerve cavity - in this case, numbness occurs immediately and lasts quite a long time.
Local anesthetics
In Russia, 4 types of anesthetics are most widely used: novocaine, lidocaine, articaine and mepivacaine.
Novocaine (procaine) was synthesized in 1905 and became widespread throughout the world as the first non-narcotic anesthetic. It is a basic reference point - all subsequent anesthetics are compared in terms of effectiveness and toxicity with novocaine, whose indicators are taken as one. After the introduction of lidocaine, it lost popularity in developed countries. There is a high frequency of allergic reactions to novocaine.
Lidocaine was invented in 1943. Its effectiveness turned out to be 4 times higher than that of novocaine (with only twice the toxicity). Widely distributed throughout the world (1st place in the number of injections among anesthetics in the USA). However, like novocaine, it has a relatively high percentage of allergic reactions (including the development of anaphylactic shock). In addition, it is often used with increased concentrations of the vasoconstrictor 1:50000 and 1:25000, which increases its effectiveness, but increases the number of complications from the cardiovascular system. Indicated for pregnant women - FDA category B (see article Use of local anesthetics for dental treatment during pregnancy; safety for women in labor).
Articaine was synthesized in 1969. It began to be used in Germany, where it was registered under the commercial name "Ultracaine". This name of the drug is now no less popular than articaine, although it represents the product of only one, “Septanest”, “Alfacaine” and several other commercial names - this is the same as “Ultracaine”. The most common local anesthetic in Europe and Russia (it was approved in the USA only in 2000, 10 years later than here). 5 times more effective than novocaine. 1.5 times more toxic. According to the FDA classification, it is classified as category C.
Mepivacaine was developed in 1957. It is equivalent in effectiveness to lidocaine and inferior to articaine. It is noteworthy that, despite category C, it is often used for pregnant patients, due to the permission of non-adrenaline release forms (lidocaine and articaine carpules are sold only with a vasoconstrictor). Although in fact it is not the first choice drug for expectant mothers (see the article Is it possible to do local anesthesia during pregnancy?).
Adrenaline , also known as epinephrine, is not a local anesthetic, but is used in the vast majority of cases for dental injections. By narrowing the blood vessels, it helps preserve the anesthetic depot at the injection site, reduces its toxic effect on the body, and also reduces bleeding (which improves visibility during surgical procedures). Its use in pregnant women and patients with cardiovascular diseases (paroxysmal ventricular tachycardia, atrial fibrillation) is undesirable. Use with caution in patients with arterial hypertension, diabetes mellitus, and hyperthyroidism.
In addition to the anesthetic and vasoconstrictor, the solution may contain preservatives (methylparaben) and adrenaline stabilizers (sodium pyrosulfite). Both methylparaben and sodium pyrosulfite (metabisulfite) have a high frequency of allergic reactions, including the most dangerous - anaphylactic shock. This risk is significantly higher than that of the anesthetics themselves (and in principle there cannot be an allergic reaction to adrenaline). Therefore, methylparaben was completely abandoned in carpules - it is needed only when using large containers for preserving an unused solution after opening the ampoule. Sulfites are necessary to prevent the oxidation of adrenaline - they cannot be abandoned in carpules with a vasoconstrictor. Therefore, anesthesia without adrenaline is recommended for patients with multivalent allergies. The frequency (up to 5%) of sulfites provoking an attack of bronchial asthma is high, so anesthesia with adrenaline is also not recommended for asthmatics.
Instruments for local anesthesia
At the moment, a carpule syringe is used to inject the anesthetic - this is a metal syringe, it can be used many times, it is sterilized in the same way as other dental instruments. A carpule with an anesthetic is inserted into the carpule syringe - a special glass cartridge, factory-made.
Currently, the Trilogy Medical and Dental Center uses carpule syringes for injection anesthesia - they are much more convenient and more sophisticated than conventional disposable syringes.
The thickness of the carpule syringe needle is only from 0.3 to 0.5 mm - thanks to this, the injection is much more painless than when using a conventional disposable syringe.
The needle is also very flexible and not brittle - thanks to this, the doctor can bend it at an angle convenient for himself and perform anesthesia even more accurately and conveniently for the patient.
What drugs are used for pain relief
Based on the experience of visiting dentists, many people ask the question: why is it painful to be treated in one clinic, but not in another? The patient's sensations may depend on many factors, but the most important is the painkiller itself.
At the beginning of the last century, novocaine was actively used, and from the middle of the century they began to use a more powerful anesthetic - lidocaine. This was considered a breakthrough in medicine, but the pain could not be completely eliminated.
Modern dental clinics use painkillers based on articaine. Let's look at the most popular of them:
Ultracaine
The most commonly used anesthesia, since the drug contains a small proportion of epinephrine (adrenaline) and almost no preservatives. Available in three forms: with an adrenaline concentration of 1:100000, 1:200000 and without it at all. The analgesic effect is achieved after 10 minutes and lasts for 2-3 hours. It is used even in the presence of allergic reactions, suitable for patients with heart disease and pregnant women. Its effectiveness is very high, while it is instantly eliminated from the body and does absolutely no harm.
Ubistezin
The drug is produced in Germany. Contains adrenaline, due to which it has a vasoconstrictor effect at the injection site. The drug has 2 release forms with an adrenaline concentration of 1:200000 and 1:100000. The analgesic effect occurs after a few minutes, and the duration of action is at least 1.5 hours.
Septanest
It has been used in dentistry for quite a long time. Available in 2 forms: with an adrenaline content of 1:100000 and 1:200000. It is used in complex cases and in the absence of contraindications. Allowed for pregnant women and children over 4 years old. A distinctive feature is good tissue tolerance and moderate vasoconstrictor effect. The duration of exposure is at least 45 minutes.
Scandonest
This drug does not contain adrenaline or preservatives. Used for adrenaline intolerance. It is not used for bronchial asthma, but is suitable for patients with diabetes, thyroid diseases, allergies and the elderly. Provides fast and strong pain relief. One drawback is the short validity period. Requires repeated administration during prolonged manipulations.
Does it happen that the anesthesia does not work?
In fact, such situations are very rare. Less than 1% of all patients are sensitive to a certain type of drug, so you just need to find the right one. Here, most often the reason lies in the incorrect administration of anesthesia or incorrectly selected anesthesia.
And in conclusion, I would like to emphasize once again: do not be afraid of dentists. Today, anesthesia allows treatment to be carried out as comfortably and painlessly as possible. And the anesthetics used for pain relief are not only effective, but also safe.
Pain relief methods
The most common method is local anesthesia, designed to reduce the patient's sensitivity to pain in the desired area. Under its influence, a person understands what is happening and can speak and hear calmly. At the same time, he does not feel anything in the place where the dentist is working.
Indications for such anesthesia may be:
- removal of the tooth and its root (not always suitable if we are talking about the “eight”);
- minor surgical interventions;
- removal of tartar (various sprays and gels are used for this);
- treatment of incompletely erupted teeth;
- elimination of periodontal disease;
- treatment of caries, especially advanced ones;
- removal of nerves;
- root canal filling;
- installation of a metal-ceramic crown.
Partial anesthesia is not relevant for major operations, injuries to the bones of the maxillofacial area and allergies to the drugs used.
General anesthesia is used extremely rarely, mainly only when the patient experiences extreme fear and stress. And it can also be recommended for psychosomatic diseases, allergic reactions to local anesthetics and extensive surgical interventions, for example, prosthetics on implants.
General anesthesia in dentistry is not allowed in the following situations:
- if more than six months have passed since the stroke and/or heart attack;
- with cardiopulmonary failure in the stage of decompensation;
- if there are serious heart rhythm disturbances;
- for diseases of the thyroid gland;
- while intoxicated;
- when the patient is under the influence of drugs;
- in case of impaired functioning of the kidneys and liver.
Scandonest SVC
If the patient belongs to a risk group (with severe concomitant diseases , in particular cardiovascular pathology ), the use of an anesthetic solution with adrenaline, a vasoconstrictor, should be completely abandoned. In such cases we use Scandonest SVC . This anesthetic exhibits a vasoconstrictor effect, i.e. has vasoconstrictor properties and can therefore be used without adrenaline, which means that the drug does not contain sulfites and can also be used in patients with bronchial asthma and allergic conditions (after an allergy test). Scandonest SVC is a medium-strength anesthetic; provides anesthesia, depending on which part of the jaw the doctor disconnects from pain sensitivity, for 20 - 90 minutes, which sets it apart from the group of other non-adrenaline anesthetics.
Local anesthesia for treatment and extraction of teeth –
If previously novocaine and lidocaine were produced in the form of vials or ampoules, and injections with these drugs were performed using ordinary disposable 5.0 ml syringes, now all modern anesthetics are produced in the form of disposable carpules (cartridges). Each carpule usually contains 1.7 ml of anesthetic, and before anesthesia it is inserted into a special carpule syringe. Next, a very thin needle is screwed on (many times thinner than ordinary needles on disposable syringes), after which the syringe is ready for use.
What does an assembled carpule syringe look like?
Carpule of anesthetic and a special needle –
The cost of anesthetics and anesthesia - the cost of one anesthetic carpule for 2022 (be it ultracaine, ubistezin, septanest or others) - will be approximately 40-50 rubles. This is the price at which dental clinics purchase anesthetics. But the total cost of anesthesia for dental treatment in a dental clinic will be about 400-500 rubles per 1 carpule of anesthetic.
It is also worth noting that pain relief during the treatment and extraction of teeth in dentistry is included in the guarantee program of the health insurance fund. Therefore, anesthesia in public dental clinics should be provided free of charge, but only when using Lidocaine or Novocaine (imported anesthetic will be paid for). Next, we will talk about the types of anesthesia in dentistry.
Anesthesia of the anterior and middle superior alveolar nerves with a single injection into the palate
Traditionally, anesthesia of teeth in the upper jaw is carried out by injection into the transitional fold in the projection of the apexes of the roots. It is a simple, safe and effective way to achieve anesthesia of the pulp and associated tissues. The main disadvantage of this procedure is the need for multiple injections to anesthetize more than one tooth, as well as excessive anesthesia for the lip and facial muscles.
However, the sensitivity of the teeth in the upper jaw can also be turned off using conduction anesthesia (infraorbital, torusal) or intraosseous and intraligamentary. The literature does not contain information about performing anesthesia with one injection for several teeth, which would not turn off facial sensitivity. Therefore, Friedman and Hochman (1998) proposed a maxillary anesthetic technique to block the anterior and middle superior alveolar rami. The authors describe effective anesthesia from the central incisor to the second premolar with a single injection into the palate. Anesthesia is expected to last 45 minutes to 1 hour (Figure 1), and the injection is performed using a computerized Wand Plus system (Milestone Scientific, Deerfield). In addition, the authors claim that numbness of the lips and facial muscles does not occur during anesthesia.
Photo 1. Anesthesia zone for blocking the anterior and middle alveolar nerves: gingiva of the vestibule of the oral cavity, teeth (central, lateral incisors, canine, first premolar, second premolar and mesial buccal root of the first molar), gums from the palatal side and oral mucosa to midline.
The essence of anesthesia is the supply of anesthetic to the anterior and middle superior alveolar branches by diffusion through many nutrient foramina on the palatine process of the maxilla (Photo 2). Both nerves are collaterals of the infraorbital nerve in the canal of the same name, which is a branch of the maxillary nerve. The anterior superior alveolar nerve departs from the infraorbital branch not reaching 5-8 mm of the infraorbital foramen. It is responsible for the innervation of the pulp of the central, lateral incisors and canines. The middle superior alveolar nerve arises from the infraorbital branch approximately 10 mm before the infraorbital foramen. This nerve supplies the pulp of the premolars and the mesial buccal root of the first molar. However, the middle branches are not present in all people. Research reports that they are found in 30-72% of individuals. When these branches are absent, the innervation of the corresponding zone is provided by plexuses between the posterior and anterior branches.
Photo 2. Arrows indicate nutrient openings
The zone of anesthesia for an anterior and middle rami block extends from the palatal side, detaching the premolars and reaching the midpalatal suture, while affecting the free gingiva (Photo 3). Theoretically, this technique is advantageous because the bilateral block of the anterior and middle branches provides simultaneous anesthesia of 10 upper teeth without numbness of soft tissues and facial muscles, which is especially convenient for restorative manipulations.
Photo 3. The injection site is indicated by an arrow, the middle of an imaginary line (a) connecting the midpalatal suture (b) and the free gingival margin (c).
Fukayama and Lee found high efficiency when using this technique using a computer system (Wand), but the resulting pulpal anesthesia percentage remained controversial. Other studies have reported the use of the technique in periodontal surgery, but only using a conventional syringe. The advantages include excellent hemostasis, no facial anesthesia and fewer injections.
The purpose of this study was to study the level of successful anesthesia of the anterior and middle superior alveolar nerves using a conventional syringe (carpule type).
Materials and methods
This clinical controlled study involved 30 Caucasian patients (16 men and 14 women) with a mean age of 22 years (range 21-25 years). During the selection process, exclusion criteria from the study were established: the presence of systemic pathology that prevents the use of an anesthetic with a vasoconstrictor, pregnancy, taking medications that affect pain perception, active orthodontic treatment, condition after tooth extraction, patients with fixed dentures, a large number of filled and endodontically treated teeth in the examined area (upper central incisor, lateral incisor, canine, first and second premolars). All information was obtained through a written survey and clinical examination. The study was approved by the ethics committee of the school of dentistry, and written informed consent was obtained from each patient.
30 patients underwent anesthesia of the anterior and middle alveolar branches on a randomly selected one half of the jaw using a carpule syringe (Hu-Friedly), 1 ml of 2% lidocaine with epinephrine 1:100,000. All injections were performed by a single specialist.
Then the upper central incisor, lateral incisor, canine, and first and second premolars of the selected side were examined. The lower canine is selected as a control tooth to monitor the performance of the pulp tester. At the very beginning, before the injection, the experimental tooth and the control canine were examined for vitality using a pulp tester (Sybron Endo). The pulse level on the pulp tester is adjusted from 0 to a maximum of 80.
The injection was carried out according to the landmarks described in the original technique of Friedman and Hochman. The injection site is located midway between the midpalatal suture and the gingival margin of the first and second premolars (Figure 3). An application of local anesthetic (20% benzocaine) is applied for 1 minute at the injection site.
The injection was performed with a 30G 22mm needle (Teruno). The bevel of the needle to the bone was oriented at an angle of 45 degrees. The needle was then slowly penetrated into the palatal mucosa until it contacted the bone and 1 ml of anesthetic solution (lidocaine 2% with epinephrine 1:100,000) was injected over three minutes (Figure 4).
Photo 4. Implementation of the technique.
The success of anesthesia was monitored by an electronic pulp tester (Sybron Endo). During the study, a protocol was drawn up. At 1 minute after injection, pulp test data were obtained for the first and second premolars. After 2 minutes the canine was tested, 3 minutes - the lateral and central incisor. At the fourth minute, the control canine was tested. The control continued with a 4-minute cycle for an hour. The criterion for pulpal anesthesia was a negative response at the maximum impulse (80). Anesthesia was considered successful when at least two consecutive negative responses were obtained at pulse 80 within one hour.
The time of onset of anesthesia and duration of effect were also taken into account.
results
The study involved 30 adult patients, 16 of whom were men and 14 women. The average age of the group was 22 years (with a range of 21-25 years). All patients received an injection to anesthetize the anterior and middle superior branches of the maxillary nerve on one side of the jaw. The injection consisted of 1 ml of 2% lidocaine with epinephrine 1:100,000. Successful pulpal anesthesia was 16-66% in the teeth examined. The onset of anesthesia is from 6 to 12 minutes and the duration is 23-40 minutes.
All subjects experienced anesthesia of the palatal tissue from the central incisor to the mesial buccal cusp of the first molar, without crossing the midline. No patient experienced pulpal anesthesia from the second premolar to the central incisor and facial tissues. While 8 patients (26.7%) did not experience anesthesia at all in any of the experimental teeth. No severe pain was experienced when the anesthetic was injected into the tissue of the palate. Also, no complications or adverse reactions were observed during and after the technique.
Discussion
The main advantage of the technique of one-stage block of the anterior and middle superior alveolar branches is the reduction in the number of injections and the amount of anesthetic solution compared to conventional infiltration anesthesia for each tooth. In addition, this technique can be ideal in cosmetic dentistry since it does not cause numbness to the lip and face.
However, the study showed the success of anesthesia in only 16.7-66.6% of cases. The criterion was a device impulse block with a value of 80. Dreven and Certosimo proved that transmission disruption at any device reading below 80 would indicate the presence of pain during the intervention.
In our study, blockage of all five experimental teeth did not occur in any of the cases, as was described by Friedman and Hochman. The effect of the anesthetic gradually decreased over 60 minutes; our study could not confirm the data of other authors who reported the effect of anesthesia within an hour. On the other hand, the absence of numbness of the lips and facial muscles is completely confirmed.
Tests of this technique using a computer system (Fukayama, Lee) showed a range of 42-86% and 35-58% successful anesthesia. In our study, when using a conventional syringe, the rates were significantly lower (17-66%). The low percentage when using a conventional syringe may be due to the less perfection of the method compared to the computer-controlled one. Automated injections are characterized by a controlled constant flow of solution. With the traditional technique, the solution flow and pressure depend on the specialist, although all injections in the study were carried out by one doctor. Lee suggests that computer-controlled injections create a special pressure gradient that allows the anesthetic to better penetrate the many feeding holes on the hard palate.
In cases of ineffective anesthesia of the central and lateral incisors, it can be assumed that the primary innervation is from the middle upper branches. While the middle branches are well anesthetized in such cases, the anterior branches remain uninvolved due to their distant location to the injection site. The study of cadaveric materials has shown that the middle superior alveolar branches are present in only 30-72% of people, and in cases of their absence, the innervation of the corresponding area is carried out by a plexus formed by the anterior and posterior alveolar nerves. The exact role of the effect of the absence of middle branches on the success of the block remains unclear.
The technique is described by the authors as a nerve block, while Malamed calls a nerve block only the process of bringing the anesthetic solution very close to the main nerve trunk, in this particular case directly to the middle and anterior superior alveolar nerves, which will ensure high efficiency of anesthesia. However, we do not observe this in the described study, since the anesthetic is deposited at the palatine process of the maxilla.
On the other hand, reducing the number of injections allows for the introduction of a smaller amount of vasoconstrictor, which is especially important in patients with cardiovascular pathology. For interventions on the mucosa and gums, anesthesia of the anterior and middle branches provides excellent hemostasis, which does not require reinforcement with subsequent injections.
One of the main disadvantages of this technique is the severe pain of the injection into the palate. Wahl states that palate injections are the most painful of all oral injections, possibly due to the pressure created in the tissue. However, in our study, patients did not experience significant discomfort due to pre-application of local anesthetic, as well as slow and controlled administration of the drug. Another disadvantage is that the technique is limited to anesthetizing only five teeth, so periodontal surgery requires a different, more complete method of anesthesia.
Another option for anesthesia with one injection from the central incisor to the second premolar is an infraorbital block. This injection is less painful, since it is not performed on the palate, however, the inconvenience of performing it causes some side effects, including numbness of the face. Karkut found that infraorbital nerve blocks are ineffective for complete pulpal anesthesia of the upper central incisor (15% success) and lateral incisor (22% success). The effectiveness of anesthesia for the canine is 92% and for premolars is 80%. Moreover, anesthesia lasts much less than an hour in all of these teeth. According to Berbeich, who studied 40 patients, the ineffectiveness of the technique in relation to incisors is also confirmed. Successful pulpal anesthesia of the canine and premolar teeth is estimated to range from 75-92%.
Corbett conducted a study comparing anterior and middle alveolar branch blocks with infraorbital foramen blocks. The success of anesthesia in the incisors was much more pronounced when performing blockade of the middle and anterior branches (42.9%). However, anesthesia of canines and premolars occurred better with blockade at the infraorbital foramen. Lip numbness was observed in 100% of cases with the infraorbital technique and in 14.3% with the palatal technique. There was no significant difference in discomfort between both techniques. It has been determined that the infraorbital technique causes more pronounced pulpal anesthesia, while the palatal one is more widespread and does not cause numbness of the face.
The shape of the palate was not taken into account in the study, but we believe that the distribution of the anesthetic between different parts of the palate was in any case homogeneous. Since the technique was used in a group of young people, the results may not be applicable to children or the elderly.
Conclusion
Since the described technique is unpredictable and not always effective, it cannot be considered the technique of choice in clinical practice. However, it is very useful when carrying out restorative manipulations, while it does not distort the smile and does not affect the facial muscles. The technique is also applicable in periodontal surgery due to excellent hemostasis in the soft tissues of the palate.
Authors: Ignacio Velasco, Reinaldo Soto Department of Oral and Maxillofacial Surgery, Los Andes University, School of Dentistry, Santiago, Chile
Medications to relieve fear and anxiety before visiting the dentist
There are many sedatives that reduce anxiety, one of which is Afobazole. This drug does not have a hypnotic effect, however, for positive results, you should start drinking it a week before the expected visit to the dentist.
Cheaper drugs (Corvalol, valerian extract, etc.) should be started three days before visiting the doctor, but these drugs in high doses can lead to weakness, drowsiness and decreased performance.
Also, in many clinics you can be given premedication - the administration of sedatives intramuscularly half an hour before dental procedures. Such drugs are classified as tranquilizers and are available by prescription (Seduxen, Relanium, etc.).