Composition and release form
Miramistin is a 0.01% solution of eye drops, colorless, transparent, and may foam when shaken. Each milliliter contains:
- Active ingredient: benzyldimethyl-myristoylamino-propylammonium chloride monohydrate – 0.1 mg
- Additional components: purified water.
Packaging: white polyethylene bottles of 50, 100, 200 ml in cardboard packs.
The bottle can be equipped with an applicator with a screw cap, as well as a sprayer or a spray pump to create an aerosol (however, this form is practically not used in ophthalmology). What cardboard packaging might look like is shown in the photo on the page. In some cases, the design may differ from what is shown.
Pharmacological properties
Miramistin solution is an antiseptic drug with a bactericidal effect. Shows activity against gram-positive bacteria and viruses, including herpes viruses and human immunodeficiency viruses. It also has an antifungal effect. It is also effective against antibiotic-resistant bacteria and sexually transmitted pathogens.
Miramistin prevents infection of burns and wounds. Stimulates regeneration processes. Activates local protective reactions, due to the improvement of the absorption and digestive functions of phagocytes, potentiates the activity of the monocyte-macrophage system. It has hyperosmolar activity, which allows it to stop wound and perifocal inflammation, absorbs purulent exudates, and promotes the formation of a dry scab. The use of the drug does not damage granulations, does not suppress marginal epithelization, and does not affect viable skin cells. The drug stimulates the resorption of dark spots on the cornea, prevents the formation of cataracts, prevents perforation and the development of ulcerative-necrotic and purulent complications, including when used in the treatment of burns and eye injuries.
When applied topically, it does not cause irritation or allergic reactions. The medicine, including in the form of eye drops, does not have embryotoxicity, carcinogenic or mutagenic properties: the antiseptic is harmless to the body when applied topically. It is not absorbed through the skin and mucous membranes, and practically does not enter the systemic circulation.
Indications for use
- Conjunctivitis, including chronic.
- Blepharoconjunctivitis.
- Traumatic keratitis.
- Eye burns, corneal erosions.
- Ophthalmochlamydia.
- Keratouveitis and corneal ulcers.
- Purulent-inflammatory processes in the anterior segment of the eye.
- Preoperative preparation, conditions after eye surgery.
In ophthalmology, Miramistin is used in complex treatment of the consequences of thermal and chemical burns and injuries to the visual organs in adults and children over 3 years old, as well as for infectious and inflammatory diseases. The drug can be used in combination with other antiseptic and antibacterial agents as prescribed by a doctor.
Directions for use and doses
The standard dosage of Miramistin solution is 2 drops conjunctivally 4-5 times daily. The frequency and volume of use in a particular case may differ from the standard ones, since in each situation the format of use is determined by the attending physician. The course of treatment can last from 3 to 10 days, which is determined by the doctor and depends on the severity of the pathology. It is not recommended to use a package form with a spray or a spray pump and spray the medicine into the affected area: this makes it difficult to calculate the dosage. It is recommended to use a package with an applicator to adjust the dose more accurately.
In order to prevent surgical infections, Miramistin solution is prescribed two days before surgery, 1-2 drops three times a day, and another 10-15 days in the postoperative period (at the same dosage) in combination with other drugs that suppress pathological activity. In some cases, the drug is dripped in a hospital setting during pre- and postoperative hospitalization.
Treatment of children with acute pharyngitis with local anti-inflammatory drugs
What are the symptoms of acute pharyngitis? What do treatment measures include? What are the features of treating infants?
Acute pharyngitis is an acute inflammation of the pharyngeal mucosa - a common manifestation of acute respiratory diseases. Typically viral in origin, it may also be associated with group A β-hemolytic streptococcus, Mycoplasma pneumoniae, or other pathogens.
As a rule, with pharyngitis, children complain of pain, discomfort in the throat (burning, soreness, itching), coughing, and sometimes itching and pain in the ears. Infants cannot complain of being unwell, but attentive parents pay attention to restless behavior, sleep disturbances, and worsening appetite. Pharyngitis can be combined with other manifestations of acute respiratory infections, such as runny nose, cough, fever, conjunctivitis.
The diagnosis of pharyngitis is made based on examination of the pharynx: there is hyperemia, swelling and infiltration of the mucous membrane of the posterior wall of the pharynx, velopharyngeal arches, and sometimes the soft palate. With lateral pharyngitis, hyperemia and swelling of the lateral ridges of the pharynx are determined. It is difficult to distinguish viral pharyngitis from bacterial pharyngitis based only on physical examination data. In both cases, during pharyngoscopy, the mucous membrane of the pharynx may be slightly hyperemic or severely inflamed and covered with a film or purulent exudate. Fever, cervical lymphadenopathy and leukocytosis are observed with both viral and bacterial pharyngitis, but perhaps they are more pronounced with the latter.
Therapeutic measures for pharyngitis include the following manipulations.
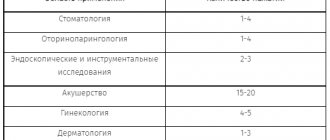
- Gargling with antiseptic, herbal solutions (for example, a solution of chlorophyllipt, rotokan, sea salt, eucalyptus, etc.) 3 - 4 times a day after meals.
- Irrigation of the pharynx with antiseptic or antibiotic-containing aerosols (such as Hexoral, Ingalipt, Cameton, Stopangin, Yox, Bioparox, Tantum Verde, etc.) 2-3 doses 2-4 times a day.
- Resorption of tablets or lozenges with an antibacterial, analgesic, emollient substance (faringosept, falimint, strepsils, laripront, etc.).
- For bacterial pharyngitis, systemic antibiotics are necessary.
Infants and young children cannot gargle or swallow tablets, so they are only prescribed to drink plenty of fluids and irrigate the throat with an antiseptic. It should be noted that children under two years of age should use all aerosols with caution due to the possibility of developing a spasm of the glottis.
The purpose of this study was to evaluate the effectiveness of a complex of local conservative measures administered to children with acute pharyngitis.
The study covered the period from October to December 2002. We observed 32 children (15 boys and 17 girls) aged 5 to 15 years (average age 9 years) with a diagnosis of acute pharyngitis. In most cases, pharyngitis was a manifestation of an acute respiratory viral infection. Children with ARVI complicated by other pathologies of the ENT organs or upper respiratory tract (sinusitis, acute catarrhal otitis media, tracheobronchitis), as well as patients with tonsillitis, were not included in the study.
| Table 1. Prevalence of complaints in acute pharyngitis in children |
The main complaints made by children are reflected in table. 1.
As can be seen from the table, the main complaints presented by children were pain, soreness and/or itching in the throat. Approximately half of the children had other signs of acute respiratory infection (runny nose, coughing). 10 children (31.3%) had a rise in body temperature (maximum up to 37.8°C), and 8 (25%) had general malaise. Sleep disturbance and loss of appetite were observed in isolated cases.
Pharyngoscopy revealed more or less pronounced hyperemia of the mucous membrane of the anterior palatine arches and the posterior pharyngeal wall in all children. Swelling and hyperemia of the lateral ridges of the pharynx were observed in 7 (21.9%) patients. In 5 (15.6%) patients, pronounced inflammatory phenomena were observed.
All children underwent the following course of conservative treatment with local anti-inflammatory drugs.
- Gargling with a 1% solution of chlorophyllipt 3 times a day.
- Irrigation of the pharynx with hexoral solution, 2 doses 2 times a day.
- Resorption of pharyngosept tablets, 1 tablet 3 times a day.
The duration of treatment was 7 days.
The effectiveness of treatment was assessed on the 4th and 7th days after the start of therapy. The criteria for the effectiveness of treatment were the following indicators:
- cessation of complaints;
- normalization of the pharyngoscopy picture;
- good drug tolerance.
The results of the treatment are presented in table. 2.
| Table 2. Treatment results |
From the presented data it is clear that on the 4th day after the start of the course of treatment, complaints ceased in more than half of the patients (56.3%), the pharyngoscopic picture returned to normal in 12 patients (37.5%). By the end of treatment (on the 7th day), none of the children had any complaints; In all children, inflammatory manifestations in the pharynx were relieved. No adverse reactions were observed during treatment with these drugs in any of the subjects studied.
Thus, a set of conservative measures using local anti-inflammatory drugs is effective in the treatment of uncomplicated acute pharyngitis in children and allows one to avoid the use of systemic antibacterial agents.
R. Kh. Nurmukhametov, Candidate of Medical Sciences, Moscow
Note!
- Acute pharyngitis is an acute inflammation of the pharyngeal mucosa and is a common manifestation of acute respiratory diseases.
- Pharyngitis can be combined with a runny nose, cough, fever, and conjunctivitis.
- The diagnosis of pharyngitis is made based on examination of the pharynx
- The main complaints presented by children are pain, soreness and/or itching in the throat.
- Carrying out a set of conservative measures using local anti-inflammatory drugs is effective in the treatment of uncomplicated acute pharyngitis in children
Contraindications
- Individual hypersensitivity.
- Pregnancy, lactation.
- Children under 3 years old.
Information on the use of the drug during pregnancy and lactation is not provided, which does not allow us to predict whether Miramistin will have any effect on the fetus. If indicated, the use of the drug may be justified if the potential benefit to the mother outweighs the possible risk to the fetus. In this case, the drug is prescribed by a doctor. Since Miramistin is practically not absorbed and does not enter the bloodstream, the risk of negative effects on the fetus is minimal. However, due to the lack of any reliable data and studies on the use of Miramistin in pregnant women, it is not recommended to instill the solution without a doctor’s prescription.
Instructions for use MIRAMISTIN (MYRAMISTIN)
As a rule, the hydrogel is easily removed from the surface of the wound. After its removal, a mucous film consisting of a mixture of hydrogel and fibrin often forms on the surface of the wound, which is easily removed with a gauze swab. In rare cases, some “drying out” of the hydrogel occurs, which makes it difficult to remove. In this situation, it is necessary to place a gauze pad, abundantly moistened with saline or Ringer's solution, on the hydrogel for 5-10 minutes, after which the hydrogel will swell and can be easily removed from the surface of the wound.
When applying the drug “Miramistin hydrogel plates 0.05%” to traumatic wounds with soft tissue defects, exposed bone and tendons
wound covering functions as a temporary covering tissue, preventing their dehydration, degeneration and infection. Dressings are performed according to indications. For minor exudation, every 1-2 days; for active exudation, daily.
For granulating infected wounds
the application is carried out after necrectomy, toilet of the wound surface. Dressings are carried out daily or every 1-2 days.
In the treatment of trophic flaccid granulating ulcers
— application of Miramistin hydrogel plates is carried out after necrectomy and toilet of the wound surface. Dressings are carried out every other day, if indicated - daily.
When performing autodermoplasty
the application is made to the donor (site where the graft is taken) and recipient beds. Dressing is performed on the 5th day during the normal course of the wound process. The hydrogel can remain in the area of the donor bed until the epithelization process is completed.
When treating conflicts
Complete excision of the necrotic epidermis and toilet of the wound surface are performed. Miramistin hydrogel plates 0.5 mg/g are applied to a clean wound surface. Dressings are performed every 1-2 days, if indicated - daily.
Bedsores:
after necrectomy and toilet, the hydrogel is applied to the wound surface. Dressings are performed daily. If granulations appear in the wound and there is no active infectious process - after 1-2 days. Direct application to necrotic scab is possible if it is necessary to soften and remove it.
Thermal burns:
- application after excision of necrotic epidermis directly onto the burn surface. Dressings are performed daily with severe exudation, with moderate exudation - after 1-2 days.
If there is abundant purulent-necrotic discharge in the wound, the hydrogel wound covering may melt with loss of medicinal properties. Use with caution in patients with a history of allergies, as well as in cases of suspected individual intolerance to miramistin.
Application in geriatric practice.
Not studied.
Application in pediatric practice.
Not studied.
Use during pregnancy and lactation.
Not studied.
Impact on the ability to drive vehicles and other potentially dangerous mechanisms.
Does not affect.
special instructions
During treatment with Miramistin solution, it is better to refrain from wearing any types of contact lenses. It is recommended to use other methods of vision correction, since wearing contact lenses for inflammatory eye diseases can complicate treatment and lead to negative consequences. If for some reason the use of alternative methods of correction is impossible, the lenses must be removed before using the drug and put on 15 minutes after instillation.
After instillation of Miramistin solution, you should not drive or engage in potentially dangerous activities for 30 minutes.
The drug is intended for external use only. Ingestion of the medicine, as a rule, does not cause serious consequences, but can lead to nausea and the development of individual allergic reactions. In case of accidental ingestion of the product, especially by young children, it is recommended to perform gastric lavage and use enterosorbents (for example, activated carbon) according to the instructions. If any negative reactions occur, you should consult a doctor as soon as possible.
Store Miramistin solution at a temperature not exceeding +25° C. It is recommended to keep the drug in a place inaccessible to young children.
Shelf life – 3 years. Do not use after the stated expiration date.
Dr. Komarovsky: Children suffer from acute respiratory infections more often than adults - this is the norm, this is the law of life
In the specialized medical literature, the abbreviation BBD is often found. The standard decoding is children who are often ill. Sometimes the expression “frequently and for a long time ill children” is used.
Maturation of the immune system
In clinics, children who are often ill are kept under special dispensary care. But let's look at the situation objectively: is it worth worrying or are these statistics arbitrary? Adults lead a less healthy lifestyle than their children, but suffer from acute respiratory infections much less often. Although our mothers told each of us that in childhood we got sick 10 times a year, and then less and less. This is a law of life: children get sick with acute respiratory infections more often than adults - this is the norm.
A child is born with an immature immune system; it takes time to develop. Babies are surrounded by many people, each of whom is a carrier of a huge number of viruses and bacteria. The child will have to develop immunity to these microorganisms. But nature has done everything to ensure that frequent childhood illnesses are not dangerous. Children's bodies easily cope with acute respiratory infections. And every encounter with the virus is training, formation, and improvement of immunity. How will this all end? A frequently ill child will become an adult and healthy parent.
Tolerate or treat?
No matter how much I urge parents to treat childhood illnesses calmly, not everyone succeeds. Sometimes a mother literally cannot count how many times a year the child has had acute respiratory infections - they simply never end. But parents should know that congenital disorders of the immune system, so-called primary immunodeficiencies, are very rare. They manifest themselves not just as frequent ARVIs, but as severe ARVIs with dangerous bacterial complications that are difficult to treat. Congenital immunodeficiency is a fatal condition and has nothing to do with a two-month runny nose. On the other hand, frequent acute respiratory infections may be a consequence of secondary immunodeficiency - that is, the child was born healthy, but some external factors interfere with the normal development of his immunity.
The main conclusion: if a child who is normal from birth does not recover from illness, it means that he has a conflict with the environment. There are two options for help: try to reconcile the child with the environment with the help of medications, or try to change the environment so that the child is satisfied with it.
Environment
The formation and functioning of a child’s immune system is determined by his lifestyle. If a child often suffers from acute respiratory infections, no pills will solve this problem. Eliminate conflict with the environment, change your lifestyle.
Housing. Organize a child's room where there is no accumulation of dust, everything is subject to wet cleaning and regular ventilation. Night temperature – 18°C, humidity – 50–70%. Soft toys are accumulators of dust, allergens and microorganisms.
Nutrition. Never force a child to eat. It is ideal to feed when he begs for food. Stop snacking, don’t overuse foreign foods, and don’t diversify your diet too much. For sweets - dried fruits, not chocolates.
Drink. Optional: mineral water, compotes, fruit drinks, fruit tea. The temperature of the drinks is room temperature.
Cloth. A sufficient minimum, since sweating causes illness more often than hypothermia. The child should not be wearing more items of clothing than the parents.
Walks. Daily, active, preferably before bedtime.
Sport. Outdoor activities are ideal, rather than in confined spaces. Swimming in a pool is not appropriate for CBI.
In summer. The child should take a break from contact with people, from city air, chlorinated water and household chemicals. Holidays “at the seas” have nothing to do with improving your health, since most of the harmful factors remain, plus public catering and worse living conditions. An ideal vacation for a private person: a village, an inflatable pool with well water, a pile of sand nearby, in shorts and barefoot. A dirty naked child who jumps from water to sand, begs for food and breathes fresh air, restores immunity in 3-4 weeks.
Prevention of acute respiratory infections. Frequent illnesses are caused not by cold, but by viruses. We must avoid unnecessary contact with people, wash our hands, maintain local immunity, and vaccinate all family members against the flu.
Treatment of ARVI
Treating ARVI does not mean giving medications, but means creating conditions so that the child’s body can cope with the virus as quickly as possible and with minimal losses. It is necessary to ensure optimal temperature and humidity, dress warmly, do not overfeed, and actively water. Saline drops in the nose and antipyretic medicine if necessary are enough. Any active treatment prevents the formation of immunity. The drug should be used only when it is clearly impossible to do without it. This is especially true for antibacterial therapy.
Actions after recovery
It is important to remember: improvement in condition and normalization of temperature does not indicate that immunity has been restored. The next day after the child’s condition improves, he goes to a group where he encounters a new virus, and a new disease will begin in a weakened body. It will be more severe than the previous one and will require the use of medications.
When it gets better, you need to live a normal life for another week - walks, “working up” your appetite, healthy sleep, restoration of the mucous membranes. Antibodies to the virus are produced no earlier than the fifth day of illness. Therefore, you can resume visiting children’s groups no earlier than the sixth day after the onset of ARVI, regardless of its severity.
There are no non-kindergarten children
When the phrase “I wasn’t sick until I was three” is said, it means we have an absolutely normal child. We went to kindergarten, the environment changed - illnesses began. We must acknowledge the fact that it is impossible to start actively communicating with children and not get sick. Constant illness means either you are in a hurry to return to your children after illness, or something is fundamentally wrong in the kindergarten itself.
Even very frequent acute respiratory infections with proper treatment do not affect the child’s health.
But if every sneeze is a reason to prescribe a dozen syrups, tablets and antibiotics, a reason for a thorough examination and consultation of a dozen specialists, such acute respiratory infections are a clear and obvious evil. If a child suffers from acute respiratory infections often, even very often, but recovers not with the help of medications, but naturally, then let him be sick, let him go to kindergarten. Published: September 26, 2016