There are a wide variety of dental diseases that damage the health of the teeth and oral cavity. Some pathologies - for example, primary caries - can be treated quickly and even without drilling the tooth; therapy for other diseases requires a whole course of procedures. For example, the treatment of periodontitis is always a complex process, since the disease affects not only the tooth itself, but also the tissues located next to it, which has a negative effect on the body as a whole.
If periodontitis develops to a certain stage, then all therapeutic measures may turn out to be useless and there will only be one way out - to remove the tooth. We will talk in detail about what periodontitis is, its forms, symptoms, and treatment methods in the following sections of the article.
Periodontitis: how does the disease appear and how does it develop?
Periodontitis is a term dentists use to refer to an inflammatory process that affects the tissues that surround the tooth and help keep it in the socket. The causes of periodontitis may vary in etiology (origin) and the disease is classified into subtypes. Correct diagnosis of the subtype of periodontitis is of fundamental importance: on its basis, the specialist will select the most effective treatment methods. Below we will get acquainted in detail with the forms of the disease, and also consider in detail their characteristic symptoms.
Infectious periodontitis
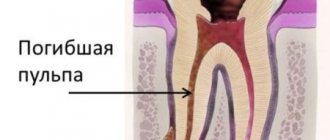
Dentists have to treat the infectious form of periodontitis in 90% of cases. The disease appears due to infection entering the root canals of the tooth and usually against the background of caries or pulpitis, the timely treatment of which was ignored. Infection in the canal cavities can also occur due to errors in endodontic treatment. The inflammatory process begins to actively develop from the moment pathogenic microflora enters the cavity of the dental canal. As inflammation spreads, not only soft but also hard tissues are destroyed; a granuloma can form, and if left untreated, a cyst.
IMPORTANT: The process of cyst formation can be asymptomatic, but the formation can grow to significant and dangerous sizes and lead to various types of pathologies, including deformation of the jaw joint.
Review of popular drugs
Today, pharmacy shelves offer a wide variety of medications, and it is very difficult to understand the assortment on your own. But this is not required when it comes to antibiotics. Such potent drugs can only be prescribed by the attending physician. Let's look at the most popular remedies that are commonly used in the treatment of periodontitis.
Tetracycline group
Broad-spectrum antibiotics aimed at inhibiting the growth of pathogenic microflora by suppressing protein synthesis. Taking medications belonging to this group is fraught with the development of side effects, among which it is worth highlighting a change in the color of dental tissues - the enamel can become very yellow or even acquire a brownish tint. This usually happens if the patient takes the drug for a long time.
The photo shows tetracycline teeth in a child
This category includes drugs such as Doxylicin and Biomycin. The first is characterized by rapid penetration into the affected tissues and almost instantaneous stopping of destructive processes. It is especially effective in the rapid development of inflammatory processes and the juvenile form of pathology. Biomycin is used in tablet form, but not orally. Half the tablet is dissolved in water, after which the affected canals, namely their mouth, are treated with it. The second part of the tablet is used to prepare a special paste for treating the canal and reducing the risk of complications.
Penicillin group
These include Sulbactam or Clavulanate. May be prescribed in combination with other antibiotics. The use of these drugs is also fraught with the development of side effects, the most common of which is an allergic reaction. It should be borne in mind that penicillin group products are quite toxic and therefore require strict adherence to the instructions.
Macrolides
This category includes drugs such as Clarithromycin, Azithromycin and Erythromycin. They have a fairly intense effect on pathogenic microorganisms, but can also cause adverse reactions. Typically, patients complain of minor problems in the functioning of the stomach and intestines, and digestive disorders.
Sulfonamides
They have a pronounced effect on pathogenic bacteria. They help stop the production of folic acid, thereby completely blocking the further development of pathological processes. Can be prescribed in combination with other antibiotics. For topical use, medications such as Dermazin, Sulfacetamide and Co-trimoxazole are prescribed.
"Metronidazole"
Available in various forms - both for oral administration and for external use. It is characterized by a fairly rapid concentration in the gingival fluid and effectively inhibits the proliferation of various bacteria. It has a number of categorical contraindications, including liver disease, leukopenia, heart failure and epilepsy. Even when using the drug externally, drinking alcohol is prohibited.
"Biseptol"
It is not an antibiotic, but is often prescribed as an antibacterial drug in the treatment of periodontitis. It usually comes in combination with drugs such as Tavegil, Fenkarol and other antihistamines. It should be noted that consuming animal and plant proteins while taking the drug reduces its effectiveness. Therefore, experts strongly recommend limiting the consumption of meat, dairy and legumes during treatment, including when using the product topically.
"Ciprofloxacin"
Antibacterial agent related to fluoroquinol derivatives. Prevents further proliferation of harmful microorganisms and suppresses the growth of pathogenic microflora by blocking the synthesis of deoxyribonucleic acid. Usually prescribed for oral administration, it is characterized by rapid absorption and rapid onset of effect. On the other hand, it can provoke a fairly wide range of adverse reactions, including disturbances in the functioning of the hematopoietic organs and nervous system, problems with the stomach, intestines, heart and blood vessels.
"Lincomycin"
Included in the glucosamine category. Suppresses the process of protein production in bacteria, which ultimately leads to their death. It is not an antibiotic, although it is widely used as an antibacterial drug, including for the treatment of inflammatory processes in the soft tissues of the oral cavity. It accumulates in the hard tissues of the tooth and jawbone, which is a significant drawback.
"Ofloxacin"
This is a drug related to fluoroquinol derivatives. Effective against gram-negative bacteria. It is often prescribed in cases where the patient is resistant to other medications. It is easily tolerated, but in some situations it leads to the development of increased sensitivity of the skin to sunlight, that is, it provokes photosensitivity1.
The decision about which antibiotics are best to take for periodontitis always remains at the discretion of the attending physician. Self-administration of potent medications is fraught with serious complications for the entire body.
Retrograde periodontitis
This form of the disease is quite rare. Periodontitis of this form begins to develop against the background of infection penetration into the periodontium through the blood flow or lymph flow.
Traumatic periodontitis
Periodontitis of traumatic origin appears against the background of trauma, when a person receives a sufficiently severe bruise. Some medical errors made during dental treatment can lead to traumatic periodontitis:
- A small piece of an instrument that was “forgotten” after treatment in the cavity of the dental canals;
- Re-filling of the dental canal, which consists of excessive filling of filling material, which ultimately protrudes beyond the apical part of the tooth root;
- Incorrectly restored natural tooth crown, prosthesis, which constantly injure the tissues of the oral cavity.
Toxic periodontitis
This form of periodontitis usually occurs after poorly treated caries, and can occur due to tissue irritation caused by certain medications.
Each form of periodontitis has its own symptoms, but inflammation in the periodontium can also be determined by some general signs:
- Pulsating and clearly localized pain, the intensity of which gradually increases. The pain impulse intensifies at the slightest attempt to touch the teeth, during the period of their closure, while eating;
- The appearance of elevated body temperature due to toothache;
- Feeling of fullness in the area of the inflammatory process;
- Swelling of soft tissues.
IMPORTANT: Severe symptoms during the development of periodontitis are not present in all cases. Some phases of the disease can occur without the slightest external signs at all, or the person feels slight discomfort, which he mistakes for ordinary caries. Professional dental examinations, which are recommended to be carried out at least once every six months, will help to identify periodontitis in a timely manner for treatment.
Characteristic symptoms
- discomfort in the area of the causative tooth, a feeling that it has become longer,
- pain when pressing, when eating,
- enlarged lymph nodes,
- general weakness, headache, fever,
- swelling of the tissues surrounding the diseased tooth,
- redness of the gums in the causative area,
- discharge of purulent exudate,
- tooth mobility.
The photo shows periodontitis
Treatment methods for periodontitis
The treatment method for periodontitis will be selected based on the characteristics of the clinical case. Methods that are used to treat inflammation in the periodontium can be divided into two groups - conservative and surgical. However, the goal of any treatment method for periodontitis will be to obtain the following results: elimination of all tissues that are affected by the infectious process, elimination of inflammation, restoration of healthy tissue, as well as restoration of the aesthetics and functional qualities of the dental unit.
To accurately diagnose, determine the form of periodontitis and select the optimal treatment method, a number of measures are carried out: a thorough examination of the patient’s oral cavity, radiography, CT, OPTG.
Stages of treatment of chronic periodontitis
The nature of the inflammatory process during periodontitis may vary depending on its type, and the set of manipulations that a specialist will resort to for high-quality treatment of the disease will depend. Chronic periodontitis, according to the nature of the development of the inflammatory process, is divided into several types:
1. Fibrous periodontitis. With this form, patients are rarely disturbed by pain impulses, and there is no deterioration in their general condition. Minor pain can be observed only when immunity is reduced due to colds, as well as when there is a noticeable mechanical load on the area of the diseased tooth. Most often, fibrous periodontitis is diagnosed during an X-ray examination.
2. Granulomatous periodontitis, a feature of which is the formation of granulomas in the upper part of the dental root system - formations of a special kind that separate infected tissues from healthy ones. This form of the disease can also develop for a long time without revealing itself, but under the influence of certain factors it can develop into acute periodontitis. Therapy for granulomatous periodontitis can be either conservative or surgical.
The course of treatment for fibrous periodontitis is faster and easier than the granulating form of therapy. This is explained by the fact that with fibrotic inflammation of the periodontium, no significant pathological changes are observed in the upper part of the tooth root, and therefore dental canals can be filled during the second visit to the dentist.
Therapy for granulomatous periodontitis can take several months and during this time you will have to visit the dentist quite often. Below we will describe in detail all the stages of treatment of chronic forms of periodontitis.
Therapeutic treatment of periodontitis: features and key stages
Therapeutic treatment of periodontitis is a complex, lengthy process and associated with certain difficulties. In particular, a fairly large amount of time is required to restore periodontal tissues damaged by inflammation; competent and high-quality treatment of dental canals will not be easy.
The complex of therapeutic measures for the treatment of periodontitis includes the following procedures:
- Drilling the diseased tooth to gain access to the canals;
- Work on expanding channels to a certain size, allowing for their high-quality processing;
- Painstaking cleaning of the canals from damaged and destroyed tissues;
- Flushing the canal cavity with antiseptic agents;
- Placement of antibiotic-impregnated linings into the tooth canals;
- Permanent canal filling;
- Restoration of the natural tooth crown.
Treatment of periodontitis may require repeated changes of medications in the canals, and therefore the patient is given a temporary filling for this period. After the inflammatory process can be completely eliminated, the tooth canals are filled with gutta-percha and a permanent photopolymer filling is placed on the tooth.
IMPORTANT: The more stages there are in the therapeutic treatment of periodontitis, the higher the price of the service as a whole will be.
When carrying out filling, it is extremely important to achieve complete sealing of the dental canals and all branches coming from them. After endodontic treatment of periodontitis, the doctor may additionally prescribe a number of medications for the patient to take that will help accelerate tissue recovery. Endodontic treatment of periodontitis can be supplemented by a number of physiotherapeutic procedures:
- UHF;
- Laser and magnetic therapy;
- Ozone therapy.
The need for additional physiotherapeutic procedures is determined by the dentist when drawing up a plan for the therapeutic treatment of periodontitis and based on the diagnostics performed and the characteristics of the clinical case.
What are the risks?
Antibiotics are potent medications, so their use is justified only as prescribed by a doctor. Most of these drugs have many contraindications, and their use is always associated with the likelihood of side effects. To reduce all risks, you must strictly follow the instructions of your doctor. In some cases, skin rashes, disturbances in the functioning of the digestive system, and acute allergic reactions are possible.
If the patient knows that he has hypersensitivity to certain drugs, he must inform the doctor about this. If adverse reactions develop while taking antibiotics, you should contact your dentist to prescribe another remedy.
- Tsarev, V.N. Transcanal use of new generation antibiotics in the treatment of chronic periodontitis, and assessment of their effectiveness using gene diagnostics, 2004.
Operative (surgical) treatment of periodontitis
Surgical techniques for the treatment of periodontitis are used if conservative therapy turns out to be ineffective or initially inapplicable due to clinical reasons. In 90% of cases, doctors try to perform tooth-preserving operations, that is, resort to a type of intervention that will eliminate inflammation, but at the same time preserve the dental unit. These types of interventions in the treatment of periodontitis include:
- Resection of the root apex. It is indicated for use when cysts and granulomas are identified during diagnostic procedures. The essence of the operation is to remove all infected tissues along with the apical part of the tooth root;
- Cystectomy. During this type of intervention in the treatment of periodontitis, the formed cyst or granuloma is removed, and the apical part of the root is excised, in which inflammation has caused pathological tissue changes.
After the operations, treatment and hermetically sealed dental canals are also carried out.
Another surgical method for treating periodontitis is an operation to amputate the apex of the tooth root. But it is possible only on multi-rooted teeth and taking into account the healthy state of the other roots of the dental unit. During intervention for the treatment of periodontitis, the crown part of the tooth can be preserved completely or partially removed. In our dental clinic in St. Petersburg you can receive services for safe and painless treatment of periodontitis. At all stages of the treatment process, dental specialists will use ultra-modern dental techniques and instruments to ensure the effectiveness of the treatment as a whole and guarantee the absence of complications.
When are antibiotics prescribed?
Antibiotics can be used in a variety of ways to treat periodontitis. The drug may be indicated for administration into the mouth of the affected canal, that is, under the crown, or into the area of the periodontal pocket. Some medications are intended for oral or topical use. Periodontitis can occur in acute or chronic form. The latter can be fibrous or granulomatous. If we are talking about an acute form of pathology, then experts in the field of periodontology distinguish serous and purulent forms.
Antibiotics are usually prescribed for acute periodontitis. Among the main indications for the use of such drugs are the following conditions:
- low effectiveness of other treatment methods,
- development of degenerative processes of the epithelium,
- concomitant somatic pathologies that complicate therapy,
- the use of surgical treatment methods,
- presence of significant periodontal abscesses.
Photo: periodontal gingival abscess
Antibiotics give the desired effect in cases where it is not possible to completely clean the periodontium surgically, as well as if there is a gingival abscess with purulent contents.
Features of the treatment of periodontitis in teeth with previously treated canals
Retreatment of tooth canals with periodontitis is an extremely difficult undertaking, during which the dentist will have to thoroughly clean the cavities from filling material. Only a truly competent and experienced specialist can perform such work in the treatment of periodontitis, because in the course of it it will be necessary to use different methods of cleaning the canals (using specialized reagents and files) and act in fact “blindly”.
After the tooth canals are completely freed from gutta-percha, they need to be thoroughly sanitized. At this stage of treatment of periodontitis, the care and literacy of the dentist are also important, because sanitary treatment of the canal cavities should ensure the complete exclusion of recurrence of inflammation in the future.
Typically, the canals for periodontitis are washed with a specialized solution, after which the doctor places medicine in their cavities and closes the tooth with a temporary filling. In the treatment of periodontitis, a pause is made, which is necessary for the complete cessation of the inflammatory process and the beginning of regeneration of tooth tissue. As soon as the desired effect in the treatment of periodontitis is achieved, secondary permanent filling of the canals and restoration of the tooth crown with a photopolymer filling are performed.
Inspection and primary treatment of dental canal cavities
Treatment of periodontitis begins with a thorough examination of the patient by a dentist, after which the specialist prescribes an x-ray for the patient. The image will help make the diagnosis as accurately as possible, as well as study in detail the number of dental canals, their length and shape. Next, an anesthetic injection is made into the area of the diseased tooth, without which treatment of periodontitis can be a very painful and uncomfortable process for the patient.
After the drug takes effect, the doctor will perform the following manipulations:
- It will remove from the diseased dental unit all tissues damaged by the carious process, as well as some healthy enamel and dentin. This is necessary to gain access to the mouths of the dental canals;
- If the tooth has not been treated before, the doctor will remove the inflamed pulp from it. If treatment of the unit with the removal of nerves has previously been carried out, the tooth canals are unfilled;
- Expand the tooth canals manually, using specialized instruments for this purpose. After expansion, the tooth canals are thoroughly washed with an antibacterial solution;
- Place a medicine with enhanced antiseptic action into the channels.
After applying the antiseptic to the dental unit, a temporary filling is installed, and the specialist thoroughly advises the patient on oral care, prescribes anti-inflammatory drugs and medications that reduce the risk of allergic reactions. The next time you will need to visit the doctor approximately three days after completing the first stage of periodontitis treatment.
Traditional medicine: can its recipes help with periodontitis?
It is important to understand that periodontitis is a serious disease that affects the entire body as a whole and is fraught with serious complications. Its treatment cannot be carried out at home, since the infectious process occurs deep in the root canals of the tooth and it is important to thoroughly clean them of all tissues affected by inflammation. Only a doctor can do this - in a clinical setting and using a specialized instrument.
Remedies from folk recipes will be absolutely useless in the fight against periodontitis and, moreover, they can aggravate your condition. For example, hot compresses for periodontitis can provoke an acceleration in the rate of spread of inflammation.
Herbal decoctions and tinctures are powerless against periodontitis. They can only temporarily make the pain less pronounced, but in this case the inflammation will actively develop, affecting an increasingly larger area of tissue. If you are bothered by even a minor toothache, a reasonable solution would be to immediately consult a dentist. Remember that it is not always possible to save a tooth with periodontitis (especially with an advanced stage of inflammation).
The goal of treatment is to get rid of the infection. To achieve this, the dentist may prescribe:
- Surgical intervention
. The dentist makes a small incision in the abscess, allowing the pus to drain, and then disinfects the area with a special solution.
- Root canal treatment
. This will help eliminate the infection and save the tooth. To do this, the dentist drills into your tooth to remove the diseased central tissue (pulp) and then removes the abscess itself. The root canals are then filled. In this case, a crown can be installed on the tooth to make it stronger, especially for teeth - molars. If you take proper care of your restored tooth, it can last you a lifetime.
- Removal
. If the affected tooth cannot be treated, the dentist will remove the tooth and then remove the abscess to get rid of the infection.
- Antibiotics
. If the infection has spread to nearby teeth, or other areas of the jaw, your dentist will likely prescribe antibiotics to stop further spread. Antibiotics may also be recommended if you have a weakened immune system.
Periodontitis treatment time
If you have been diagnosed with periodontitis, you should prepare for a lengthy treatment process. You will have to visit the dental clinic more than once, and in addition, strictly follow all the recommendations that the specialist will give you during the treatment process. Violation of medical recommendations can lead to complications that will increase the complexity and duration of periodontitis treatment. In the simplest case, when treating periodontitis, you will have to visit the dentist two or three times; treatment will be longer if it is supplemented by physical procedures and will require repeated placement of antibiotics into the tooth canals and consultation with highly specialized specialists. Remember that high-quality treatment of periodontitis will imply mandatory control photographs after each stage.
Radiography will allow you to track the positive changes achieved after certain procedures for the treatment of periodontitis, and evaluate the quality of canal filling. Only this approach guarantees a stable and positive result in the treatment of periodontitis and eliminates relapses of inflammation and complications.
Periodontitis in children: treatment
Treatment of periodontitis in primary teeth is not an easy task, which requires the dentist to have great skill in performing manipulations and, more importantly, making the right and consistent decisions. The choice of adequate treatment depends on the accuracy of the assessment of the condition of the tooth.
Milk teeth affected by periodontitis must be removed in a number of cases: for example, if less than two years remain before their natural loss or if the tooth has acquired noticeable mobility as a result of the disease. The tooth is also removed if most of its root is affected by the pathological process, and if the patient’s history contains references to previous exacerbations of the chronic inflammatory process. A tooth that does not respond to treatment can become a constant source of infection, which poses a significant danger - especially if the patient's immune status is reduced as a result of illness or other factors.
Unfortunately, a simple examination and even instrumental diagnostics do not always provide accurate information about the condition of the tooth and surrounding tissues. A small carious cavity can cause extensive damage to the root and periosteum. However, in many cases, periodontitis in children can be asymptomatic. For this reason, an obligatory component of treatment is to conduct X-ray examinations at various stages - to monitor the condition of the tooth and the effectiveness of the manipulations performed.
Sources:
- Prevention of recurrence of localized periodontitis in young A.K. YORDANISHVILI, Doctor of Medical Sciences, Professor, North-Western State Medical University named after. I.I. Mechnikov, Military Medical Academy named after. CM. Kirov, International Academy of Sciences of Ecology, Human Safety and Nature.
- The role of anti-inflammatory rinse in the treatment of periodontal diseases (L.Yu. Orekhova, A.A. Leontyev, S.B. Ulitovsky) L.Yu. OREKHOVA, Doctor of Medical Sciences, Prof., Head of Department; A.A. LEONTIEV, dentist; S.B. ULITOVSKY, Doctor of Medical Sciences, Prof. Department of Therapeutic Dentistry of St. Petersburg State Medical University named after. acad. I. P. Pavlova
Periodontitis treatment price
The cost of periodontitis treatment is always calculated individually, because it consists of a number of factors. The price of the service will depend on the set of diagnostic measures that are carried out not only at the beginning of treatment, but also at its intermediate stages. The price of the service will be influenced by the form of the disease, method of treatment, additional procedures, equipment and drugs that can be used during its course.
If you want to know the price of periodontitis treatment or make an appointment with Uni Dent dentists, just dial our contact phone number!
Temporary filling
During a second visit to a dentist-therapist during the course of treatment of chronic periodontitis, the area of manipulation is examined. The specialist will also clarify whether the patient has any complaints of pain, swelling in the gum area or other discomfort. If such negative phenomena are not observed, temporary filling of the dental canals is performed.
For this purpose, the temporary filling is initially removed, as well as the antiseptic placed in the tooth canals. The canal openings are thoroughly washed with an antiseptic and then filled with a special type of composite material used for temporary filling. This composite contains calcium hydroxide, a substance that destroys pathogenic microflora and also catalyzes the process of bone tissue regeneration in the area of the upper zone of the tooth root. Temporary filling of canal cavities is done for a fairly long period - from two to three months. The dentist then places a temporary filling in the crown of the tooth.
Treatment of purulent periodontitis
Therapy comes down to two main points:
- Ensuring the drainage of pus. For this purpose, the infected pulp, which has already become gangrenous, is removed from the dental cavity and root canals. In some cases, for quick drainage, they resort to dissecting the periosteum. After the first day of treatment for purulent periodontitis, the tooth remains open, and the patient is prescribed a course of antibiotics and rinses to stop the inflammatory process.
- Restoration of tooth structure. During the next visits to the doctor (their number will depend on the presence or absence of pain in the patient), instrumental and medicinal treatment of the root canals is performed, after which the tooth is filled.
Symptoms and signs of periodontitis.
As mentioned earlier, periodontitis may not manifest itself for a long time; the patient runs the risk of finding out about the disease too late, when it has entered the acute stage. In this case, the signs of inflammation of periodontal tissues will be felt much more clearly. Periodontitis is characterized by the following symptoms:
Deterioration of general condition.
There is an increase in temperature, worsening sleep, weakness, etc.
- Pain when chewing food and when closing the jaws.
- Change in gum color (become darker).
Based on this symptom, periodontitis can be identified in its initial stages of development. Also, the periodontal tissues may swell, and the swelling may spread to the cheek and neck.
Painful sensations.
In the acute course of the disease, the patient begins to be bothered by a sharp, aching pain that radiates to neighboring teeth.
- Slight tooth mobility.
- The appearance of bad breath.
- Increased sensitivity due to mechanical impact on the tooth.
Flux on the gum
First visit
The doctor prescribes general treatment for periodontitis to alleviate the symptoms of intoxication in the patient’s body caused by purulent inflammation. Treatment is carried out using the following drugs:
- non-steroidal anti-inflammatory drugs;
- antibiotics supplemented with Metronidazole;
- antihistamines.
Second visit
A second visit is usually scheduled after a few days. Here the root canals are thoroughly washed with antiseptic solutions. After this, a long-acting antiseptic drug is placed in each of the root canals, and the tooth is covered with a temporary filling.
Third visit
If the pain is reduced and there is no pus in the root canals, they are washed again and permanently filled with gutta-percha. Then, as part of the control plan, an x-ray is taken to confirm that the root canals are filled to the root apex.
Fourth visit
Finally, during the fourth and final visit, a permanent filling is placed. It is impossible to put her in the same visit when the root canals were filled!
Diagnosis and treatment
Diagnosis of the disease begins with asking the patient about previous dental treatment, the nature of the pain and general well-being.
To establish an accurate diagnosis and determine the disease, X-ray diagnostics are used. In the image, purulent periodontitis is visualized as a white spot in the tooth cavity, which fills the entire hole. The formation of a cyst or granuloma is also possible, so if these elements are present, the image will show an oval or round compaction, depending on the type of neoplasm.
An alternative diagnostic method is electroodontometry. It allows you to diagnose the disease using current. If a certain amount of electricity is applied, the tooth should not normally react to it. If the tooth still responds, this indicates the presence of periodontitis.
Treatment of acute periodontitis and exacerbation of chronic
These forms of the disease are characterized by concomitant severe inflammation in the gums and the development of suppuration. The patient is in pain. If the situation is ignored, it sometimes leads to swelling of the soft tissues of the face and a rise in temperature.
Such symptoms should be treated urgently. When a person goes to the hospital, the doctor identifies an exacerbation of chronic or diagnoses acute periodontitis and performs an autopsy of the tooth. This way, the pus leaves the root canals, and the patient feels better.
If the abscess has spread further into the tissues of the mouth, even into the cheeks, the dentist will cut the gum.
After the operation, fillings are not placed and the treatment steps described above are not applied. The patient lives for several days with an open tooth or accessible canals to ensure the outflow of pathological contents. While eating, the tooth is closed with a cotton ball, then opens again. The main thing for the patient is to prevent pieces of food from getting into uncovered cavities, avoiding re-inflammation.
In a paid clinic, the mentioned procedures are performed at the patient’s expense; the cost depends on the rating of the institution and the category of the doctor. Usually - in the range of 2000-2500 rubles.
When visiting a hospital at the place of residence with an insurance policy and passport, the patient has the right to count on free medical care.