The ENT organs, being an outpost of the immune system on the path of infection into the body, are the first to encounter the effects of various pathogens. That is why inflammatory processes often begin in them. Inflammation of the paranasal sinuses is called sinusitis . In total, a person has 4 pairs of paranasal sinuses, these are cavities filled with air. As a result of inflammatory processes, pus is formed in the sinuses, and the person begins to feel weak and unwell.
1
Nasal endoscopy in MedicCity
2 Nasal endoscopy in MedicCity
3 Rhinoscopy in MedicCity
Symptoms of sinusitis
There are acute and chronic forms of sinusitis, which differ in their symptoms.
Acute sinusitis. Symptoms:
- Runny nose lasting more than 7-10 days, without signs of improvement;
- nasal congestion, mucous or purulent discharge from the nose;
- mucus running down the back of the throat, copious discharge of purulent sputum in the morning;
- headache, heaviness and pain in the inflamed sinus area. Sometimes pain in the teeth, eyes, cheekbones, cheeks;
- increased sensitivity of the facial skin in the projection of the affected sinus;
- increase in body temperature (up to 38°C and above). As a rule, this symptom is observed in an acute case. In a chronic process, body temperature rarely rises or remains at subfebrile levels (37-37.50°C);
- weakness, fatigue, irritability. Photophobia, lacrimation, loss of appetite, sleep disturbance;
- weakened or absent sense of smell;
- swelling of the cheeks and eyelids.
Chronic sinusitis. Symptoms:
Symptoms of chronic sinusitis depend on the form of the disease. Outside of an exacerbation, symptoms may be very mild or absent. The most common symptoms of concern are:
- nasal congestion, difficulty in nasal breathing;
- scant mucous or purulent discharge from the nose, may be in the form of drying crusts;
- constant leakage from the nose, causing cracks and abrasions at the entrance to the nose;
- mucus running down the back of the throat;
- dry throat;
- headache;
- bad breath.
As the disease worsens, symptoms characteristic of acute sinusitis may appear.
Results and discussion
Analysis of the results of radiological diagnostic methods revealed signs of RFS in 110 (66.2%) of 166 cases. 66 (39.7%) patients had characteristic clinical symptoms of the disease (headache, low-grade fever, sleep disturbance, a feeling of heaviness in the corresponding half of the face when tilting the head anteriorly, nasal congestion on one side only); these patients were referred for radiation examination by otorhinolaryngologists. The remaining 44 (26.5%) people did not have complaints from the maxillary sinuses; Previously, they were sent for examination by dentists and maxillofacial surgeons for the following reasons: 22 (13.2%) patients - to clarify their dental status, 12 (7.3%) patients - before dental implantation, 10 (6%) patients - for postoperative control after surgical interventions on the upper jaw. In these cases, the identified inflammation of the maxillary sinus was a diagnostic finding.
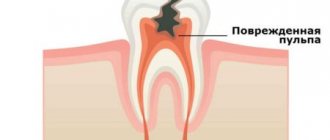
As is known, acute odontogenic inflammation of the maxillary sinus develops within 1-3 days. Quite often the cause is an inflammatory process of the upper jaw (acute or exacerbation of a chronic one). Such conditions include complications of dental caries, periodontitis, periostitis, osteomyelitis, as well as suppuration of dental cysts or granulomas [7, 8].
Typical complaints of patients with acute maxillary sinusitis were: difficulty in nasal breathing, rhinorrhea, loss of smell, headache and facial pain, a feeling of heaviness in the corresponding half of the face when tilting the head forward, low-grade fever, as well as night cough and sleep disturbances. Odontogenic sinusitis, in contrast to rhinogenic sinusitis, has the following distinctive features: isolated damage to one of the maxillary sinuses, pain in the tooth or in periodontal tissues that precedes the disease, disruption of the facial configuration as a result of swelling of the soft tissues of the cheek and pain on palpation of the anterolateral wall of the maxillary sinus.
In acute sinusitis, x-rays showed thickened mucous membranes, darkening, and fluid levels. In chronic sinusitis, a decrease in sinus transparency was noted.
When assessing and analyzing diagnostic images, the criteria for odontogenic sinusitis were the following: the presence of a foreign body of metallic density corresponding to a filling material or implant in the sinus cavity; deep caries and signs of periodontitis of premolars and molars of the upper jaw; destruction of the lower bone wall of the maxillary sinuses in the area of pathologically changed teeth, as well as partial adentia of the upper jaw in the area corresponding to changes in the maxillary sinus.
During an X-ray examination, in 44 (26.5%) patients with acute maxillary sinusitis, a thickened mucous membrane and/or subtotal darkening with a horizontal fluid level was detected on a plain radiograph. In 78 (47%) patients, there was a total decrease in sinus transparency, of which 38 (22.8%) patients had foreign bodies of metal density (corresponding to filling material) found in the sinus cavity. However, the low contrast of liquid and soft tissues and the summation of shadows made it difficult to objectively assess the obtained radiographs. For additional assessment of the condition of the teeth of the upper jaw, all patients underwent orthopantomography, which did not allow reliably assessing the condition of the maxillary sinuses, and in 13 (7.8%) patients, accurately interpreting changes in the area of the apexes of the teeth of the upper jaw (due to the reflection of the projection layering of complex anatomical structures ).
According to the results of our study, 24 (14.5%) patients showed signs of chronic periodontitis in the area of premolars and molars of the upper jaw (Fig. 1). Deep caries was diagnosed in 4 (2.4%) patients, maxillary cysts in the area of the roots of premolars and molars were visualized in 6 (3.6%) cases.
Rice. 1. CBCT. Panoramic (a) and multiplanar reconstructions of the right (b) and left (c) maxillary sinuses of patient M., 37 years old. Diagnosis: bilateral odontogenic chronic maxillary sinusitis. CT signs of chronic granulomatous periodontitis of teeth 1.8, 2.7, 2.8 are noted (in the form of foci of destruction at the apices of the roots, round in shape, with clear, even contours). The lower bone walls of the sinuses are thinned and cannot be traced in the periodontal area of teeth 1.8 and 2.8 (indicated by arrows). In the lower part of the right maxillary sinus, a parietal soft tissue formation of a homogeneous structure with a polycyclic upper contour is determined. The left maxillary sinus is subtotally filled with soft tissue contents of a homogeneous structure with a rounded upper contour.
Filling material was found in 38 (22.8%) patients (Fig. 2). Of these, in 34 (20.4%) patients in the submucosal layer of the lower wall of the sinus, in 4 (2.4%) - in the upper section near the medial wall of the sinus (Fig. 3). 8 (4.8%) patients were diagnosed with dental implantation errors: the tip of the implant was immersed in the sinus cavity, which caused the development of chronic odontogenic maxillary sinusitis, as well as complications in the form of chronic polysinusitis ( n
=4; 2,4%).
Rice. 2. MSCT. Coronal (a) and sagittal (b) reconstruction of the right maxillary sinus of patient K., 29 years old. Diagnosis: right-sided odontogenic chronic maxillary sinusitis. The roots of teeth 1.6, 1.7 and 1.8 are immersed in the cavity of the maxillary sinus. Condition after endodontic treatment of teeth 1.6 and 1.7, with removal of the filling material beyond the apex of the palatal root 1.7. In the area of the roots of teeth 1.6 and 1.7, there is a rarefaction of bone tissue with fuzzy, uneven contours (radiological signs of granulating periodontitis). In the lower part of the sinus, a parietal soft tissue formation with a polycyclic contour is determined; the bony walls of the sinus are not traced in this area.
Rice.
3. CBCT. Sagittal reconstruction, right maxillary sinus. Patient U., 48 years old. Diagnosis: right-sided odontogenic chronic maxillary sinusitis. Teeth 1.6 and 1.7 after endodontic treatment, the filling material is removed from the apex of the roots of tooth 1.6 (the material is located in the bone tissue of the alveolar process and in the submucosal layer of the sinus). A loss of bone tissue is determined in the area of roots 1.6 and 1.7; the bone wall of the sinus is not visible in this area (arrow). In the lower part of the sinus, thickening of the mucous membrane up to 10 mm is determined, in the superomedial part of the sinus an irregularly shaped foreign body of metal density is visualized (corresponding to fragments of filling material). In our study, 30 (18.1%) patients had absence of maxillary teeth in the area corresponding to changes in the maxillary sinus, which also made it possible to judge the odontogenicity of maxillary sinusitis.
In all cases, computed tomography (MSCT or CBCT) made it possible to accurately diagnose the form of the disease, determine the extent of damage to the sinuses, assess the condition of the lower bone wall of the sinus (identify a violation of its integrity and the communication of the tooth socket with the sinus), determine the source of inflammation in the periodontium, and also identify the presence of foreign bodies in the maxillary sinus. At the same time, the data from MSCT and CBCT were completely comparable with each other, significantly superior to traditional X-ray techniques in terms of diagnostic information content and had such advantages as the absence of superposition, high contrast resolution and the ability to obtain higher-quality reconstructions of images in various planes and 3D images of the area of interest, and also a significant reduction in patient examination time and a reduction in radiation exposure. After computed tomography, treatment tactics were adjusted in 38 (22.9%) patients.
Sinusitis in children
Sometimes sinusitis in children is more difficult to see than sinusitis in adults. The disease usually develops after an infection: influenza or sore throat, and is often accompanied by otitis media. The symptoms are somewhat blurred and appear weaker than in adults. Here are the main ones:
- purulent or mucous discharge from the nose;
- general weakness, malaise;
- pungent odor from the mouth.
With sinusitis in children, one side of the face is often inflamed. While sinusitis in adults is often accompanied by headaches, headaches in children are extremely rare.
Types of sinusitis
There are several types of sinusitis:
- sinusitis;
- frontal sinusitis;
- ethmoiditis;
- sphenoiditis, but the latter type of sinusitis is extremely rare and almost always together with ethmoiditis.
1 Examination of the nasal cavity in MedicCity
2 Examination of the nasal cavity in MedicCity
3 ENT unit Atmos S 31
Sinusitis
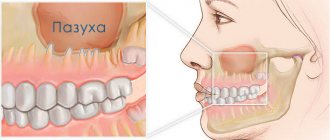
Sinusitis is one of the most common types of sinusitis. This disease is accompanied by inflammation in the maxillary and maxillary cavities. During inflammation, swelling of the mucous membrane occurs, which blocks the opening from the sinus to the nasal cavity. Mucus begins to accumulate in the sinus space, pathogenic bacteria multiply, and pus appears. Inside the cavity, pressure occurs on the vessels, and the person begins to feel pressing pain at the site of accumulation of pus.
Chronic sinusitis is the result of a long inflammatory process, when a person has had sinusitis for more than 2 months. The patient develops general weakness, nasal discharge has an unpleasant odor, the sense of smell is impaired, and a night cough appears. Chronic sinusitis is characterized by inflammation of only one sinus, right or left. Pressure in the sinus can cause a deviated nasal septum.
Symptoms of sinusitis
The following symptoms are characteristic of sinusitis:
- increased body temperature;
- copious discharge, nasal congestion;
- disturbances of smell;
- weakness;
- headache radiating to the forehead, bridge of the nose, teeth;
- pain that intensifies when tilting the head and pressing on the sinus;
- constant, intense pain;
- a feeling of fullness in the forehead and cheeks, aggravated by tilting the head, coughing and sneezing;
- photophobia and lacrimation.
Signs of sinusitis
If after a flu or cold the temperature rises again, your health worsens, severe pain appears when tilting your head and when pressing on the sinuses, then you need to urgently consult an otolaryngologist. These could be manifestations of sinusitis! Sinusitis in adults is often advanced, since adults are usually in no hurry to see a doctor.
Treatment of sinusitis
Antibiotics for sinusitis are used only after a complete examination of the patient, based on the characteristics of his body and possible allergic reactions.
Antibiotics are not advisable in case of sinusitis of allergic or fungal origin. For mild sinusitis, inhalations, rinses and immunotherapy are also sufficient.
1 Rhinoscopy in MedicCity
2 Video endoscopy of the nasopharynx in MedicCity
3 ENT office in MedicCity
Patients and methods
In the period from 2013 to 2015 in the Department of Radiation Diagnostics of Clinical Hospital No. 1 of the First Moscow State Medical University named after. THEM. Sechenov examined 166 patients with maxillary sinusitis of various etiologies. In 110 patients (66.2%) the odontogenic etiology of the disease was confirmed. An analysis of the distribution of patients according to age and gender showed that of the examined patients with TFS, the majority - 91 (54.8%) people - were young and mature, from 21 to 60 years of age. There were 19 (11.4%) patients over 60 years of age; the average age of patients was 48 years (from 21 to 81 years). The majority were female (62 (37.3%) women and 48 (28.9%) men) of working age.
A comparison of the clinical manifestations of odontogenic HFS and the X-ray picture made it possible to conditionally group patients into two groups: 66 (39.7%) patients with an acute inflammatory process in the maxillary sinus had corresponding clinical symptoms of the disease, and 44 (26.5%) patients had complaints from the maxillary sinus no sinuses were presented (the inflammatory process in the maxillary sinus was chronic).
A comprehensive X-ray examination was performed in all cases. All patients underwent computed tomography (MSCT or CBCT): MSCT - 76 (45.8%) patients, CBCT - 90 (54.2%) patients. 122 (73.5%) patients underwent radiography of the paranasal sinuses in the nasomental, semi-axial projections. To clarify the condition of the teeth of the upper jaw, orthopantomography was performed ( n
=166, 100%) and intraoral contact radiography (
n
=12, 7.3%).
When assessing and analyzing diagnostic images, the criteria for odontogenic sinusitis were the following: the presence of a foreign body of metallic density corresponding to a filling material or implant in the sinus cavity; deep caries and signs of periodontitis of premolars and molars of the upper jaw; destruction of the lower bone wall of the maxillary sinuses in the area of pathologically changed teeth.
Frontit
Frontal sinusitis (frontal sinusitis) is an inflammatory disease of the frontal paranasal sinus. This type of sinusitis is the most severe. There are forms of acute and chronic frontal sinusitis.
Symptoms of sinusitis
Acute frontal sinusitis, symptoms:
- pain and swelling around the nose and eyes;
- increased pain when tapping in the projection area of the inflamed sinuses;
- heavy breathing due to inflammation of the nasal passages;
- runny nose with thick yellow or green mucus;
- increase in body temperature to 38-39 degrees;
- severe headache (minor relief occurs when lying down);
- pain radiating to the ears and teeth;
- fear of light;
- severe weakness;
- sometimes sore throat, difficulty identifying odors, decreased pungency of taste.
Chronic frontal sinusitis, symptoms:
- aching headache;
- purulent, unpleasant-smelling nasal discharge in the morning;
- slight increase in temperature;
- difficulty breathing through the nose;
- sputum discharge in the morning.
Causes of frontal sinusitis
The following reasons for the development of frontal sinusitis are distinguished:
- viral, bacterial or fungal infection;
- complication after influenza, ARVI, etc.;
- getting foreign objects into the nose;
- long-term infectious or allergic rhinitis (rhinitis);
- deviated nasal septum;
- adenoids;
- allergy;
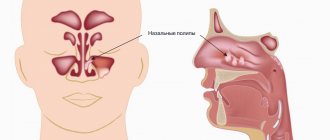
- nasal polyps.
Treatment of frontal sinusitis
How to treat frontal sinusitis? Definitely under the supervision of an otolaryngologist! The disease is not only difficult for many patients to tolerate, but also has dangerous complications, including orbital abscess, meningitis, sepsis, etc.
Treatment of sinusitis is aimed at eliminating infection in the sinuses and stopping inflammation. Medicines will help relieve swelling, improve ventilation of the sinuses and lead to the discharge of contents from them. If the disease is viral in nature, then antibiotics for frontal sinusitis are mandatory!
The following antibiotics are used to treat sinusitis:
- penicillin antibiotics (semi-synthetic or synthetic amoxicillin preparations);
- cephalosporin antibiotics;
- macrolide antibiotics (they do not affect the intestinal microflora);
- local antibiotics in the form of nasal drops, nasal spray, aerosol;
- homeopathic medicines;
- symptomatic remedies for frontal sinusitis in the form of vasoconstrictor nasal drops, antipyretics and anti-inflammatory drugs.
In case of severe frontal sinusitis and insufficient effectiveness of conservative treatment, sinus lavage using the method of displacement and puncture is prescribed.
1 Rhinoscopy in MedicCity
2 Consultation with an ENT specialist in MedicCity
3 ENT consultation in MedicCity
Prevention of frontal sinusitis
To prevent frontal sinusitis, you need to monitor the state of your immune system, promptly eliminate foci of inflammation in the ENT organs, harden your body, and lead a healthy lifestyle.
Causes
There are three reasons for the appearance of pathology. They usually cause disease in the presence of provoking factors, which lead to a drop in immunity and a weakening of the body's natural defenses. In individuals who suffer from a constant decrease in immunity, the likelihood of pathology occurring is especially high. The following reasons provoke the development of the disease:
- penetration of infection into the nasal sinuses - the problem is most often caused by bacteria and somewhat less frequently by viruses. Exceptional cases would be fungal sinusitis. Penetration of bacteria can occur from the pharynx, nasal passages, or the infection enters the sinuses with air;
- an allergic reaction also often provokes the appearance of pathology. Due to allergies, swelling of the mucous membrane develops, which disrupts the outflow of the contents of the paranasal sinuses. As a result of this, stagnation develops in them, which becomes the cause of further formation of sinusitis, which in most cases is bilateral;
- mechanical blocking of the sinus lumen - various polyps in the nasal cavity are often bilateral, which is why the ventilation of the paired sinuses is impaired. This cause of pathology is not common, but it can occur.
Doctors identify the following types of effects on the body as factors that lead to a drop in local immunity and allow the problem to begin to develop:
- smoking in active and passive forms;
- severe general hypothermia;
- the presence of chronic inflammatory pathologies of the pharynx;
- chronic inflammatory diseases of the nasal cavity;
- proliferation of adenoids;
- the presence of carious teeth in the upper jaw that are left without treatment;
- chronic lack of sleep;
- chronic fatigue - not only physical, but also emotional;
- severe stress;
- monotonous diet, in which the body does not receive enough vitamins and minerals.
If there are predisposing factors that significantly increase the likelihood of developing sinusitis, special attention to your health is required. In such a situation, any runny nose that persists for more than 7 days requires a mandatory visit to an otolaryngologist. It is unacceptable to refuse professional treatment in such cases.
Ethmoiditis
Ethmoiditis is an acute or chronic inflammation of the mucous membrane of the cells of the ethmoid labyrinth (anatomical labyrinth in the bridge of the nose). Ethmoiditis is bacterial or viral in nature.
There are acute and chronic ethmoiditis. Acute ethmoiditis accompanies influenza, rhinitis and is complemented by inflammation of the paranasal sinuses.
Ethmoiditis in adults affects both the frontal and maxillary cavities. With weak immunity, the acute form of ethmoiditis turns into long-term chronic ethmoiditis with periods of exacerbation and remission.
Polypous ethmoiditis is characterized by the appearance of polyps in the mucous membrane of the ethmoid labyrinth of the forehead. Polypous ethmoiditis may appear after chronic, allergic rhinitis.
Catarrhal ethmoiditis occurs due to the activity of viruses. It is characterized by increased lacrimation, weakness, nausea, dizziness, swelling in the bridge of the nose, and fever.
Ethmoiditis in children is a very serious disease. The infection spreads very quickly due to the anatomical structure of the ethmoid labyrinth. The development of ethmoiditis in children requires urgent hospitalization.
Symptoms of ethmoiditis
Acute catarrhal ethmoiditis. Symptoms
- pain in the bridge of the nose and at the wings of the nose;
- heavy breathing through the nose;
- loss of smell;
- headache, weakness;
- profuse nasal discharge, which gradually becomes purulent;
- temperature rises to 38 degrees;
- In children, the inner corner of the eye socket also swells and turns red.
In the acute form, primary and secondary ethmoiditis are distinguished.
With primary ethmoiditis, anxiety, vomiting, dyspepsia and toxicosis appear, the temperature is 39-40 degrees.
Secondary ethmoiditis is more severe and develops faster. The patient is in extremely serious condition with pronounced septic symptoms. The eyelids become swollen and cyanotic, swelling of the conjunctiva and noticeable protrusion of the eyeball are observed, and nasal breathing becomes difficult.
Chronic ethmoiditis. Symptoms
- headaches that are difficult to register by localization;
- weakness, rapid fatigue of the patient;
- soreness in the bridge of the nose when pressed and painful points at the wings of the nose;
- purulent discharge with a nauseating odor;
- extensive mucus in the nasopharynx, which is difficult to spit out;
- emerging polyps.
Complications after ethmoiditis:
- meningitis;
- encephalitis,
- intraocular and intracranial pressure;
- destruction of the ethmoid bone.
Treatment of ethmoiditis
Treatment of ethmoiditis in acute form is predominantly conservative. It is necessary to ensure the outflow of mucus with the help of vasoconstrictors and physiotherapeutic procedures.
Treatment of ethmoiditis in chronic form is predominantly surgical.
1 MRI in MedicCity
2 Laboratory diagnostics in MedicCity
3 Ultrasound examination of the paranasal sinuses in MedicCity
Diagnosis of sinusitis using modern techniques
To confirm the diagnosis of sinusitis, the following types of examination are used:
- Video endoscopy of the nasal cavity and nasopharynx to identify features of the anatomical structure and determine predisposing factors for the development of sinusitis;
- radiography of the paranasal sinuses;
- Ultrasound examination of the paranasal sinuses is a safe method with no contraindications, used to diagnose sinusitis and monitor the treatment process;
- CT, MRI - according to indications;
- laboratory diagnostics according to indications in full.
Diagnostics
A presumptive diagnosis is made by a specialist at the first appointment. During it, a history of the disease is collected and the patient’s complaints are listened to. Palpation of the sinus areas and rhinoscopy are also performed. To further confirm the diagnosis, an examination is indicated. This makes it possible to accurately determine the degree of damage and diseased sinuses.
1. X-ray of the facial part of the head. It is carried out most often, as it allows you to immediately assess the condition of the sinuses. At the same time, this method also has contraindications. It should not be used during pregnancy or childhood.
2. Magnetic resonance or computed tomography. Allows you to identify the affected sinuses as accurately as possible, as well as immediately assess the general condition of the nasal cavity and detect neoplasms, if any.
3. General blood test. It is not always required, but is usually prescribed only if there is a significant impairment in the patient’s condition.
If the main reason for the appearance of the pathology is an allergic reaction, the patient is referred for an allergy test. This skin procedure identifies the irritant.
Treatment of sinusitis at MedicCity
Conservative methods of treating sinusitis
If you are concerned about how to treat sinusitis in Moscow, be sure to contact the MedicCity specialists! Our clinic provides treatment for sinusitis without puncture and without pain. However, non-surgical treatment of sinusitis is possible only at the initial stage. Don't waste time!
In the vast majority of cases, treatment of sinusitis in our clinic is carried out without a puncture.
- Using YAMIK (sinus catheter). The YAMIK method is the use of a device called the “YAMIK sinus catheter.” Using the YAMIK sinus catheter, controlled pressure is created in the nasal cavity and the purulent contents of the sinus are pumped out through the natural anastomosis (openings), and then a medicinal substance (antibiotics, mucolytics) is administered.
- Rinsing the nose and paranasal sinuses using the moving method (“cuckoo”). It is carried out using a special suction - an aspirator; in the process, pathological contents are removed from the nasal cavity and sinuses and the drug is injected into the sinuses.
- Inhalation therapy using a special inhaler PARI SINUS. This method is based on the introduction of microparticles of the drug into the affected paranasal sinuses through a pulsating supply of an aerosol. In this case, the aerosol of the medicinal substance is deposited in the sinuses and has an effect directly at the site of inflammation.
All proposed methods for treating sinusitis are painless and effective.
When using combined treatment, complete recovery in case of acute sinusitis is achieved within 7-10 days.
If puncture treatment is necessary, it is possible to install special catheters in the sinus, which eliminate the need for repeated punctures.