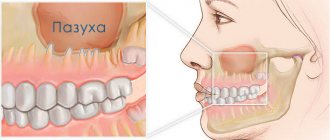
When removing upper molars and premolars, the doctor must act with extreme precision and accuracy. After all, incorrect actions threaten that fragments of the root may get into the cavity of the maxillary sinus. Perforation is also possible when installing an implant used in implantology and in root canal treatment.
Perforation of the bottom of the maxillary sinus in the upper jaw is one of the complications that occurs after tooth extraction in the upper jaw. This is not a separate disease, but during dental exposure it occurs quite often. From the article you will learn what kind of pathological condition this is, how it can be eliminated surgically and therapeutically, and what it means for the patient.
The maxillary sinus is located in the thickest bone tissue located in the upper jaw. It is separated from the oral cavity by the so-called alveolar process, which is required for the formation of the floor. According to physiological indicators, the volume of the nasal sinus in adults can reach sizes of up to ten cubic centimeters.
The location of the maxillary sinus poses a danger when performing certain surgical operations on teeth in the upper jaw. It's all about the roots of the teeth, which can reach the bottom of the nasal sinus or even penetrate the alveolar process. This can only be seen on a targeted photograph, which must be taken by the dentist before surgery.
Molars and premolars are located closest to the maxillary sinuses. It is worth saying that perforation can be predisposed not only by the particularly anatomical location of the upper teeth, but also by the presence of cystic neoplasms, periodontitis, and periodontitis as the main secondary factor.
Why can odontogenic sinusitis occur?
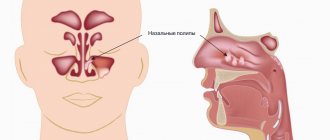
The maxillary (maxillary) sinus is a cavity with bony walls that is located inside the upper jaw. The cavity communicates with the nasal cavity through the anastomosis, which is located on the side wall of the sinus facing the nasal cavity. The lower wall has contact with the upper teeth. Quite often (in about 15% of cases) the apex of the tooth root lies directly under the mucous membrane of the bottom of the maxillary sinus, and there is no bone septum between them.
When an infection enters the maxillary sinus, inflammation of its mucous membrane or sinusitis occurs.
There are two ways of infection:
- rhinogenic - through the nasal cavity. In this case, the infection penetrates from the nasal cavity through natural or artificial (after surgery) communication;
- odontogenic - through the tooth or tissue around it.
Odontogenic sinusitis most often develops slowly against the background of chronic infection in the area of the tooth root. As a result of chronic inflammation, a cyst forms in the root area, which destroys the barrier between the sinus and the tooth. Pathogenic microbes gradually penetrate the sinus mucosa, causing inflammation.
Also, odontogenic sinusitis can occur as a result of the actions of the dentist. Often, after the removal of the upper tooth, the thin barrier between the sinus and the oral cavity may be damaged. As a result, a gateway for dental infection appears. In this case, the anatomical features of the patient with a thin bone septum between the sinus and the tooth root or its complete absence are of key importance.
Infection can occur when cleaning the canals and filling them. In some cases, the filling material gets inside the sinus, causing the formation of fungal sinusitis, and the zinc contained in the filling material promotes the growth of mold fungi (Aspergillus, Mucora). Also, odontogenic sinusitis can develop after the sinus lift procedure and the installation of dental implants in the upper jaw.
Perforation of the maxillary sinus: diagnosis
In order to accurately make a diagnosis, CELT dental surgeons:
- Anamnesis is collected, which includes the removal of an upper jaw tooth or endodontic treatment, surgery to replenish bone volume or implantation of an implant;
- An examination is carried out to identify the cause of the perforation, the hole is probed, and the patient is asked to exhale by opening his mouth and closing his nose;
- The patient is prescribed an X-ray examination of the maxillary cavities and orthopantomography;
- The patient is prescribed an endoscopic examination of the nasal cavities.
Complications
With odontogenic sinusitis, a chronic inflammatory process occurs. Dental microflora appears in the sinus, not typical for the upper respiratory tract, which can destroy bone tissue. Due to the fact that the paranasal sinuses have contact with the orbit and brain, odontogenic sinusitis can lead to severe complications:
- intraorbital (orbital phlegmon, ophthalmitis, optic nerve neuritis);
- intracranial (meningitis, encephalitis, brain abscess).
Therefore, at the slightest suspicion of this disease, you should consult a doctor.
Diagnosis of “dental” sinusitis
Inflammation of the antrum can have several causes and does not necessarily have to come from the teeth. Since treatment should always be cause-and-effect, the doctor must make an accurate diagnosis. In the context of odontogenic sinusitis, unilateral onset of symptoms is typical. Other complaints, such as pain, which is usually worse when bending over, are additional symptoms.
Further investigations include rhinoscopy (nasal endoscopy) and imaging techniques:
- X-ray examinations;
- CT (computed tomography);
- DVT (digital volumetric tomography);
Treatment
The treatment of odontogenic sinusitis requires an integrated approach. As a rule, treatment requires the simultaneous participation of an otolaryngologist and a dentist. Isolated antibacterial and conservative therapy lead only to temporary relief of the condition and removal of the severity of the process.
For a complete recovery, it is necessary to eliminate the source of infection - remove or treat the causative tooth while simultaneously sanitizing the inflamed sinus.
In case of foreign inclusions in the sinus (filling material, sinus lifting material, fungal bodies), their complete removal is necessary. For this, endoscopic techniques are used. They allow you to remove these formations through the nasal cavity. If there is a connection between the sinus and the oral cavity (oroantral fistula), it must be closed using special bioinert collagen-based membranes and mucosal flaps.
Symptoms of perforation
If perforation of the nasal sinus occurred at the time of tooth extraction, then its symptoms will be quite specific:
- The appearance of small air bubbles in the blood released from the tooth socket, the number of which increases with a sharp forced exhalation through the nose.
- The appearance of bloody discharge from the nose on the side of the perforated maxillary sinus.
- Changes in the timbre of the patient’s voice, the appearance of “nasality”.
Sometimes the patient begins to complain about the passage of air through the hole after tooth extraction, as well as a feeling of heaviness or pressure in the projection of the maxillary sinus.
If perforation of the maxillary sinus occurs during implantation or endodontic treatment, the doctor may suspect it by:
- characteristic failure of the instrument or implanted element after applying some force to advance it;
- changing the position of the instrument in the wound;
- the appearance of small air bubbles in the blood.
If perforation of the maxillary sinus for any reason was not diagnosed and treated immediately, then its cavity becomes infected with the development of acute sinusitis or sinusitis, which is characterized by symptoms such as:
- severe acute pain in the maxillary sinus area;
- swelling of the nasal mucosa on the corresponding side with difficulty breathing through the nose;
- the appearance of purulent nasal discharge.
The appearance of general symptoms of intoxication is also characteristic: headaches, chills, high fever, weakness.
Old perforations
If the perforation of the maxillary sinus was not promptly identified and eliminated, then after 2-4 weeks the stage of acute manifestations will subside, and a fistula will form in the area of the defect, connecting the sinus cavity with the surface of the gum.
This process is simultaneously accompanied by symptoms of chronic sinusitis:
- constant dull pain in the sinus area radiating to the orbit and temple;
- nasal congestion on the affected side;
- purulent discharge from the nasal cavity, as well as from the fistula;
- Sometimes patients have swelling of the cheek on the side of the damaged sinus.
Most patients also complain of a sensation of air moving through the fistula when talking or sneezing, difficulty pronouncing certain sounds, and liquid food entering the nasal cavity from the mouth.
Treatment of such chronic perforations with fistulas presents some difficulties, since the presence of a chronic focus of inflammation in the maxillary sinus significantly reduces the effectiveness of therapy and quite often leads to relapse and re-formation of the fistula canal.
Such patients are indicated for surgical intervention, which includes opening the maxillary sinus with removal of all non-viable tissues and foreign bodies from its cavity, excision of the fistula and plastic closure of the defect. Antibiotics after removal of the fistula are prescribed for a course lasting 10-14 days with the simultaneous use of anti-inflammatory and antihistamine drugs, and the use of physiotherapeutic methods of treatment.
Preparing for surgery
Before removing a wisdom tooth in the upper jaw, the doctor prepares the patient for the upcoming operation. The preparatory process consists of:
- X-ray examination of the problematic tooth;
- clinical examination of the patient for the presence of pathologies and other concomitant diseases that may affect the course of the operation;
- removal of subgingival and supragingival deposits from the tooth being removed and adjacent teeth to prevent the penetration of infected plaque into the alveolus.
The surgeon also assesses the patient’s psycho-emotional state and, if necessary, recommends taking a sedative.
Safe and high-quality removal of wisdom teeth in Balashikha
The Berezka dental clinic offers qualified assistance to anyone who, for certain reasons, requires the removal of a wisdom tooth from above or below. The operations are performed by experienced surgeons using safe anesthesia and modern instruments.
Before the procedure, the dentist collects the patient’s medical history, conducts all the necessary examinations, and only if the clinical picture is present is it possible to extract the wisdom tooth.
The operation is performed in a comfortable environment for the patient. Innovative equipment and professional dentists ensure successful and safe removal of the most complex teeth.
Features of tooth extraction in the upper jaw
The structure of the upper and lower jaws is significantly different. They also vary in density and location. Therefore, the method of tooth extraction will differ:
- on the upper jaw the operation is faster;
- the recovery period is shorter;
- pain relief is simpler and more effective.
Complications during tooth extraction in the upper jaw occur less frequently than in the lower jaw.
Anesthesia
The secret of high-quality pain relief is the correct delivery of the drug to the nerve. The choice of anesthesia method takes into account the patient’s age, his general condition, and the complexity of the tooth being removed.
Anesthesia of the upper jaw
The upper jaw is less dense than the lower jaw. It is covered with a cortical plate with many holes. Nerves and blood vessels pass through them. Pain relief is easier and faster than in the lower jaw
Sinus damage
Above the upper jaw is the nasal sinus, also known as the maxillary sinus. Its bottom may be close to the root of the tooth being removed. Then, during removal, sinus perforation may occur. This complication is typical for surgery on molars. This pattern is explained by the fact that the jaw in the area of the incisors is longer, and the nasal cavity is further away relative to them.
The main sign of sinus perforation is the escape of air, food and fluid through the nose. There is foam in the hole. Hospitalization in a hospital may be indicated for treatment.
Entry of part of the root into the sinus
Due to perforation of the sinus, part of the root can get inside it. This is caused by thinning of the bone plate or errors during the removal operation.
The symptoms when part of the root gets into the sinus are the same as when perforation occurs: air and contents of the oral cavity escape through the nose. But at the same time there is pain and increased body temperature. Treatment requires hospitalization.
Features of the maxillary sinuses
Sinus lift surgery is closely related to the anatomy and functioning of the maxillary sinuses. Each maxillary sinus has the same structure, but has certain differences that the dentist must pay attention to when planning the operation.
There are two main types of maxillary sinus:
- Hyperpneumatized. It is a large volume cavity with increased airiness.
- Hypopneumatized. A small space characterized by sclerotic areas.
When assessing the results of radiography or computed tomography, the dentist always pays attention to the structural features of the maxillary sinus in order to accurately calculate his actions during the operation. In addition, examination of the maxillary sinus is required in order to exclude any signs of an inflammatory process, which the patient may not even be aware of.