Causes of inflammatory damage to the trigeminal nerve
Factors contributing to inflammation of the trigeminal nerve are:
- surgical interventions on the jaw bones;
- fractures of the base of the skull, lower and upper jaws;
- tumors;
- complex tooth extraction;
- hypothermia;
- surgery on the maxillary sinus;
- improperly administered anesthesia;
- incorrectly performed dental prosthetics;
- metabolic disorders;
- the presence of foreign bodies that irritate the nerve trunk or injure nerve endings;
- bacterial or viral infection;
- various types of intoxication of the body;
- hypovitaminosis;
- weakening of the immune system.
Examination for facial nerve disease - find and eliminate the cause of the disease
The symptoms of facial nerve pain are almost the same in all cases, but its causes are different and require different treatments. Treatment “blindly” can delay the healing process. Therefore, in our clinic everything starts with searching for the exact cause and location of the nerve damage.
MRI of the brain, temporal bone. MRI scans show the brain centers of the facial nerve and its area of exit (root) to the base of the brain, blood vessels, and temporal bone. Circulatory disorders, cysts and tumors are easily recognized.
Blood tests to check for infections, biochemical changes that damage the facial nerve. The trigeminal nerve is a favorite area of attack by the herpes virus group. The suspicion of the presence of the virus and its activity can be easily verified using a blood test.
Electromyography, Blink reflex - measurement of electrical potentials of facial muscles. Helps assess the function of impulse transmission along the facial nerve, the degree of its impairment, judge the effectiveness of treatment, the presence of complications, and help in choosing the correct treatment tactics.
Stimulation electromyography of the facial nerve (electroneuromyography, myography of the facial nerve)
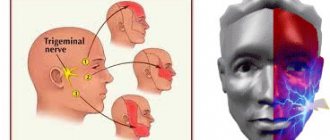
Symptoms of trigeminal neuritis
The maxillary trigeminal nerve consists of three types of nerve fibers:
- vegetative;
- motor;
- sensitive.
The symptomatic picture of neuritis may vary depending on which fibers were affected by the inflammatory process.
Damage to sensory fibers
In particular, with inflammation of the sensory fibers, the patient may complain of a tingling sensation, numbness, and weakened sensitivity in the area innervated by the trigeminal nerve.
Damage to motor fibers
When motor fibers are damaged, there is a partial or complete decrease in strength in the innervated muscles, their atrophy and deterioration of tendon reflexes.
Damage to vegetative fibers
When the vegetative fibers are inflamed, the patient experiences cyanosis and swelling of the skin, dryness and thinning of the skin, and the potential risk of developing a trophic ulcer increases.
Diagnosis of inflammation of the facial nerve
If the doctor is properly qualified, then only based on the patient’s complaints will he be able to make a diagnosis and identify the severity of the pathological process. But even if the clinical picture is typical, the patient will have to undergo a series of diagnostic examinations:
- take blood and urine tests;
- undergo magnetic resonance imaging;
- do electroneurography.
The results obtained will help determine what treatment for inflammation of the facial nerve will be. In addition, such an examination will allow the doctor to identify the body’s perception of non-steroidal anti-inflammatory drugs - these are the drugs that will be used for therapy.
Pain due to inflammation
In addition, a disease such as inflammation or neuritis of the facial trigeminal nerve makes itself felt with attacks of pain of a very diverse nature:
- cutting,
- burning,
- pricking,
- tearing
- shooting, etc.
In this case, the area of pain does not always correspond to the area of innervation and can spread to the lower jaw, cheeks and chin.
Pain may be accompanied by:
- muscle spasms (facial, chewing),
- the appearance of nasal discharge,
- development of hypersalivation,
- increased lacrimation.
Lack of sensation in the tongue, lips and chin
With inflammatory damage to the trigeminal nerve, not only the entire nerve can be damaged, but also its individual branches. This is why numbness and pain can occur in various areas of the face. For example, when the lingual branch of the nerve is inflamed, patients complain of pain and sensitivity disturbances in the anterior part of the tongue, and when the mental branch is damaged, in the area of the lips and chin.
Pain when laughing, chewing, brushing teeth and shaving
Pain due to neuritis of the maxillary trigeminal nerve can intensify with touching, chewing, laughing and with changes in temperature. That is why patients, trying to prevent the recurrence of painful attacks, avoid excessive mobility and prolonged conversations, and refuse brushing their teeth and shaving.
Treatment of the facial nerve at the Echinacea clinic
The treatment will be structured like this:
- Find and eliminate the factor that damaged the nerve (viruses, for example);
- Stimulate nerve regeneration.
If you neglect the first point, the chances of restoring the nerve are reduced, and the risk of facial contracture increases. The average duration of treatment is 2 months; you can complete most of the course at home on your own.
The planned result is restoration of the functioning of the facial muscles. Possible difficulties are advanced disease, significant narrowing of the facial nerve canal, damage to the myelin sheath of the nerve, leading to the appearance of a nervous tic of the eye, which to some extent complicates the treatment process. Read more about the causes and treatment of nervous tics.
Treatment of neuritis of the maxillary trigeminal nerve
Therapy
The treatment program for trigeminal neuritis is drawn up taking into account the causes of the disease and its clinical signs. The main goals of treatment are:
- achieving a sensitizing effect;
- fight against bacterial and viral infection;
- increasing the body's immune forces;
- elimination of swelling of the nerve trunk;
- restoration of natural adaptive and compensatory reactions;
- normalization of the patency of nerve impulses.
Healing procedures
The set of procedures aimed at blocking the inflammatory process and eliminating all manifestations of neuritis includes:
- antibacterial therapy;
- antiviral therapy;
- elimination of factors contributing to the occurrence of intoxication;
- removal of tumor-like neoplasms or dissection of adhesions compressing the nerve;
- prescribing vitamin and mineral complexes to the patient;
- stimulation of nerves and muscles;
- acupuncture;
- physiotherapy (electrophoresis, phonophoresis, UHF, ultrasound, paraffin therapy).
People suffering from trigeminal neuritis are advised to regularly visit dental clinics and have their oral cavity sanitized.
Reasons for development
Facial nerve neuropathy can develop for the following reasons:
- progression of herpes, polio, mumps, enterovirus;
- hormonal imbalances (the disease appears especially often in the first half of pregnancy);
- tooth infections;
- sudden and severe hypothermia;
- injuries of the skull and jaws;
- sinusitis, otitis;
- diabetes;
- poor circulation in the blood vessels of the face;
- multiple sclerosis.
Most often, the disease in question develops when the facial nerve is cold - a short stay in a draft is enough for the inflammatory process to begin its progression.
Classification
Neuritis of the facial nerve can be primary or secondary.
The primary form of inflammation occurs as an independent disease in a healthy person due to hypothermia. This type of neuritis is called catarrhal neuritis.
The secondary form of inflammation develops against the background of infection, otitis media or another disease.
In the vast majority of cases, the disease is acquired, much less often it is congenital.
The congenital nature of the disease may be indicated by Melkersson-Rosenthal syndrome - swelling of the face combined with folding of the tongue.
If treatment does not bring results. Synkinesia and facial contracture
Facial symmetry returns in an average of 3 months. If your treatment has not brought results, facial asymmetry persists, pain or other symptoms appear, you should immediately clarify the cause of the dysfunction of the facial nerve. The location and cause of the nerve injury may not have been recognized and treatment was prescribed blindly. Perhaps little attention was paid to restorative procedures.
Facial synkinesis is a condition when, for example, closing the eye is accompanied by movement of the mouth and cheek, and smiling is accompanied by closing the eye, etc. Synkinesis occurs more often in cases of long-term, chronic disease of the facial nerve. Most often in these cases we find a chronic inflammatory process in the area of the nerve bed.
The most problematic complication of facial paralysis is contracture, i.e. cicatricial degeneration of facial muscles. The result of contracture is loss of elasticity and immobilization of the facial muscles, even after the function of the facial nerve itself has been restored. Contracture appears as a result of prolonged untreated paralysis of the facial muscles and/or as a result of inadequate recovery procedures (insufficient intensity of exercise or, conversely, excessive stimulation of the facial muscles). Facial contracture is partially reversible. We usually use local injections of the anti-scar drug Longidaza: we inject it with a very thin needle directly into the area of scarring of the facial muscles.
Symptoms
The first attack of pain can be triggered by elementary things that no person can do without: laughter, smiling, articulation, brushing teeth, eating, frostbite on the face. Pain appears in one half of the face. At first, the painful attacks are short-lived. They end, just as they begin, abruptly. Over time, pain occurs more frequently and lasts longer. Often the pain begins to originate in the jaw and can be confused with toothache. Then the painful sensations move to the area of the cheek, ear, and forehead. There is lacrimation, paresis of the facial muscle, and the face becomes asymmetrical. After the attack, a period of remission occurs, which lasts several minutes. During remission there is no pain.
Diagnosis of neuralgia
Diagnosis of neuralgia in the CELT Clinic does not cause difficulties, since it has a number of pronounced signs. When talking about the clinical manifestations of the disease, patients try not to touch the affected side of the face and remain in a tense state because they expect a new attack.
Studies are carried out on the functions of the facial and trigeminal nerves, which begin with assessing the symmetry of the patient’s face. In addition, a number of tests are carried out to check taste and sensitivity.
For the most accurate diagnosis of pathological processes in the nerves of the face, an ultrasound scan of the nerves is performed.