General information
Sialadenitis is an inflammatory process in the salivary glands. In humans, there are three pairs of salivary glands in the oral cavity, which secrete saliva and discharge them into the oral cavity through special ducts, thereby ensuring a normal digestive process. These are the parotid , submandibular and sublingual glands.
The main functions of saliva are to soften food and also facilitate the process of swallowing it. During the inflammatory process, the production of saliva becomes difficult, and during the process of eating a person feels significant inconvenience. During the development of the disease, pain, swelling of the face, etc. are noted. If the process progresses, a purulent cavity or tumor may form. The disease develops in both young children and adults. Damage to the salivary glands requires consulting a doctor and carrying out the prescribed treatment. The ICD-10 code for sialadenitis is K11.2. How inflammatory diseases of the salivary glands manifest themselves, what treatment is most effective in such cases - this will be discussed in the article.
Lacrimal gland disorders
Disorders of the lacrimal gland manifest themselves in increased tear production ( hyperfunction ) or insufficient production of tear fluid ( hypofunction ).
Increased lacrimation may occur due to bright light, strong wind, cold and other external irritants, or as a result of disturbances in the innervation of the eye. A characteristic sign of lacrimal duct pathology is increased lacrimation (epiphora).
Hypofunction of the lacrimal glands (or “dry eye syndrome”) is one of the manifestations of Sjögren’s syndrome. It also occurs in endocrine and autoimmune diseases, in patients on hormone replacement therapy, in people who work for a long time behind a monitor, in smokers.
Pathogenesis
There are three pairs of major salivary glands in the human mouth. The parotids are located under the auricle in front and are the largest. The submandibular muscles are located under the lower jaw. Accordingly, sublingual - under the mucous membrane of the floor of the oral cavity on both sides of the tongue. These glands produce saliva, which is produced through ducts located in the oral cavity. Saliva ensures normal digestion by softening solid foods.
Reactive-dystrophic pathological processes occur in stages. At the initial stage , there are no symptoms of the inflammatory process, but the lymph stagnates near the blood vessels and ducts. The vessels become overfilled with blood, the lymph around the gland ducts stagnates, and the connective tissue loosens. The acini (terminal sections of the salivary gland) are completely preserved, and mucopolysaccharides and mucin accumulate in them.
The second stage of the disease is characterized by the presence of signs of an obvious chronic inflammatory process. There are signs of atrophic changes in the end parts of the gland, infiltrates are detected in the sclerotic stroma. Fibrous tissue appears near the excretory ducts of the gland. Lymphocytes and epithelial cells accumulate in the lumen of the ducts.
At the third stage, almost complete atrophy of the gland parenchyma occurs, and it is replaced by connective tissue. Blood vessels dilate, the ducts of the gland dilate or narrow if they are compressed by connective tissue.
Prevention
Preventing inflammation of the salivary gland is easier than treating it. To do this you need to follow only 4 rules:
sanitize the oral cavity, cure carious teeth, pharyngitis, tonsillitis; remove foci of infection, especially those located near the ear canal and throat; stimulate and strengthen the immune system; protect your body from stress and be less nervous. The acute process ends either with transition to chronicity or with recovery. Chronic sialadenitis is often complicated by atrophy, sclerosis and is difficult to treat. That is why it is so important to consult a doctor in a timely manner and not self-medicate.
Classification
Taking into account the peculiarities of the process, acute and chronic sialadenitis are distinguished.
According to nosological independence, two forms of the disease are distinguished:
- Primary is an independent disease.
- Secondary – a complication in the development of other diseases ( flu , sore throat , etc.).
Taking into account the causes of the development of the disease, the following are distinguished:
- Traumatic – a consequence of injuries and the influence of external factors.
- Radiation – a consequence of irradiation.
- Toxic – a consequence of chemical influence.
- Infectious – develops after infection.
- Allergic.
- Autoimmune.
- Obstructive - a consequence of blockage of the excretory duct by a foreign body or cicatricial narrowing of the duct.
According to the location of the lesion there are:
- Inflammation of the sublingual salivary gland - the inflammatory process of the sublingual gland is also called sublingual gland.
- Inflammation of the parotid salivary gland - in this case, the cheeks swell and there are signs of general intoxication. Sialadenitis of the parotid gland is also called mumps .
- Sialadenitis of the submandibular salivary gland is an inflammatory process of the submandibular salivary gland. When this gland is damaged, calculous sialadenitis , which is characterized by the development of stones in the ducts of the salivary glands or in their parenchyma.
Taking into account the condition of the parenchyma, the following forms of the disease are distinguished:
- interstitial sialadenitis - only stromal damage occurs.
- parenchymal sialadenitis - in addition to the stroma, the parenchyma is also affected.
Depending on the nature of the inflammatory process, the following forms of sialadenitis are distinguished:
- Purulent.
- Serous.
- Hemorrhagic.
- Connective tissue.
- Destructive.
- Granulomatous.
- Fibroplastic.
- Sialadenitis without deformation of the gland.
- Sialadenitis with scarring of the gland.
There are also epidemic and non-epidemic sialadenitis.
- The epidemic form of the disease develops against the background of viral diseases and infections.
- Non-epidemic form - diagnosed if there is a blockage of the salivary gland. Such blockage can develop as a result of injuries, salivary stones, or foreign bodies entering the ducts.
Symptoms of mumps
Mumps is an inflammation of the parotid gland caused by a viral infection. This pathology is characterized by an acute onset of the disease. Parotid swelling occurs, painful when palpated, and a high temperature rises.
There is no specific treatment for this disease. Therapy comes down to relieving symptoms and providing comfort to the sick person.
The main dangers of mumps are its serious complications:
- acute pancreatitis;
- orchitis;
- oophoritis;
- ovarianitis;
- meningoencephalitis.
Reliable insurance against such serious consequences as the development of infertility in men and women, diabetes mellitus or deafness is vaccination.
Causes
There are a number of factors that provoke the development of sialadenitis:
- Wrong approach to oral hygiene.
- Diseases in which the composition and viscosity of saliva changes.
- Postponed surgeries.
- Infectious diseases - influenza, encephalitis , herpes , ARVI , etc.
- Oral diseases – caries , pulpitis , periodontitis , etc.
- Dry mouth.
- Treatment with chemotherapy , radiation therapy .
- Diabetes.
- Disorders of mineral metabolism leading to stone formation.
The epidemic type of the disease develops as a result of infectious processes. Most often, this condition develops with mumps (mumps) . This virus is transmitted from infected people through airborne droplets.
The non-epidemic form of the disease is usually associated with blockage of the glands. This happens with injuries or exposure to foreign bodies. Also the cause of the development of this form of the disease is the so-called salivary stone disease ( sialolithiasis ). If a person develops sialolithiasis of the submandibular salivary gland, the resulting stones may block the ducts.
What are tears for?
With the help of tears, you can not only express your emotional state, first of all, we need them to protect our eyes. A thin layer of tear film covers the surface of the cornea and makes it perfectly transparent and smooth, protecting the eyes from drying out.
At the heart of tears is an antibacterial enzyme - lysozyme , which helps cleanse the conjunctival sac of small foreign bodies and microorganisms.
In normal conditions, a small amount of tears is required to moisturize the eye - 0.4-1 ml per day; it is produced by additional conjunctival glands. Large lacrimal glands begin to work when additional irritants appear: severe pain, emotional stress, foreign body contact with the conjunctiva or cornea. And also in too bright light, exposure to smoke and toxic substances.
Symptoms of salivary gland inflammation
The signs that inflammation manifests largely depend on where exactly the pathological process is localized.
submandibular sialadenitis develops , symptoms may be as follows:
- Pain in the submandibular area, which becomes worse when chewing.
- Swelling in the area of the salivary gland, which may increase.
- Temperature increase.
- Taste of salt or pus.
- Swelling of the face.
- Redness and swelling in the mouth.
If sialadenitis of the sublingual salivary gland , similar symptoms develop. The mouth of the exit ducts of the gland turns red and swelling develops. The pain may be more severe than with submandibular sialadenitis .
With parotid sialadenitis, more pronounced symptoms appear. There is marked swelling and asymmetry of the face, redness of the skin. The patient is bothered by dry mouth. The pain intensifies when palpating the affected area. The temperature rises and the general condition worsens. Shortness of breath may bother you . Palpation of the parotid salivary gland leads to the appearance of cloudy saliva mixed with pus.
Symptoms of salivary stone disease can manifest themselves in a similar way. I am concerned about soreness and dry mouth. At the same time, it is difficult for a person to open and close his mouth.
Dacryocystitis
Dacryocystitis is called inflammation of the lacrimal sac. The disease can occur in both acute and chronic forms. Chronic forms of dacryocystitis include simple and ectatic catarrhal, empyema and phlegmon of the lacrimal sac, as well as stenosing dacryocystitis. At the same time, it is customary to distinguish dacryocystitis of newborns, which can manifest itself in simple, ectatic catarrhal, purulent and phlegmanous forms.
Acute dacryocystitis, as a rule, is an exacerbation of chronic dacryocystitis and is manifested by purulent inflammation of the walls of the lacrimal sac. If the surrounding tissue is involved in the inflammation process, phlegmon of the lacrimal sac may form.
The occurrence of dacryocystitis is caused by stenosis of the nasolacrimal duct, when stagnation of tear fluid occurs in the lacrimal sac. This promotes the proliferation of pathogenic (usually staphylococcal and streptococcal) flora within. The cause of disruption of the outflow of tears is inflammation of the mucous membrane of the nasolacrimal duct, usually passing from the nasal mucosa. In newborns, the disease occurs due to atresia (infestation) in the nasolacrimal duct of the outlet.
In acute dacryocystitis, patients report lacrimation, swelling, redness and acute pain in the inner corner of the eye. Inspection and palpation of the lacrimal sac, as well as adjacent areas of the nose and cheek, reveals swelling and redness of the tissues, their density and soreness. With swelling of the eyelids, a narrowing of the palpebral fissure is observed. At the beginning of the disease, pus may be discharged from the lacrimal openings when pressing on the lacrimal sac; the tubular test is positive. Frequent: increased body temperature, general weakness and headache. After a few days, the infiltrate softens and fluctuation appears. As a rule, the formed abscess opens spontaneously.
Dacryocystitis of newborns is manifested by the discharge of mucus and pus from the lacrimal openings, the tubular test is positive, and the nasal test is negative. Rinsing the lacrimal ducts reveals obstruction of fluid into the nasal cavity. A possible complication of the disease, developing as phlegmonous acute dacryocystitis.
Treatment of acute dacryocystitis should be carried out only in a hospital. Injections of antibiotics and NSAIDs are prescribed as anti-inflammatory therapy. Until the moment of fluctuation, UHF therapy is used. Fluoroquinolone antibiotic solutions (ciproloxacin, ofloxacin, etc.) are also prescribed conjunctivally.
In case of fluctuation, the phlegmon is opened and drainage is placed with a sodium chloride solution. The wound surface is washed with antiseptic solutions for some time. Then drugs are prescribed to activate tissue regeneration (methyluracil ointment, levomekol).
Dacryocystitis in newborns begins to be treated with a jerky massage of the lacrimal sac from top to bottom. After this, antiseptic solutions are instilled conctivally. If there is no effect, perform passive lavage of the lacrimal ducts with antiseptic solutions or probing the lacrimal canaliculus with a Bowman probe.
Treatment of chronic dacryocystitis is surgical, for which dacryocystorhinostomy is performed (a new path for the outflow of tears is created). In the postoperative period, antibiotics and NSAIDs are prescribed systemically and locally.
By contacting the Moscow Eye Clinic, each patient can be sure that some of the best Russian specialists will be responsible for the results of treatment. The high reputation of the clinic and thousands of grateful patients will certainly add to your confidence in the right choice. The most modern equipment for the diagnosis and treatment of eye diseases and an individual approach to the problems of each patient are a guarantee of high treatment results at the Moscow Eye Clinic. We provide diagnostics and treatment for children over 4 years of age and adults.
Tests and diagnosis of sialadenitis
Diagnosis of sialadenitis is carried out using clinical, instrumental and laboratory methods.
The essence of clinical methods is the collection of complaints and anamnesis. The doctor also examines the patient.
Laboratory methods - a general blood and urine test, a biochemical blood test are performed. A study of saliva is also carried out, in which, during the inflammatory process, leukocytes and an admixture of pus are found.
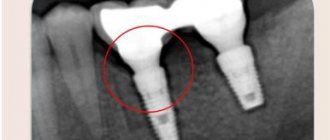
Hardware methods - diagnosis of diseases of the salivary glands involves, first of all, sialography with contrast, that is, x-rays of the gland. With the help of such a study, stones, narrowing of the lumen of the excretory duct, as well as other obstacles to the normal secretion of saliva are determined.
CT, MRI - it is advisable to carry out if the presence of stones is suspected.
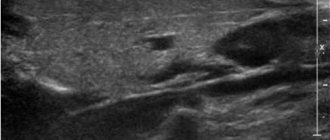
Ultrasound - allows you to determine the structure of the gland and the characteristics of the inflammatory process.
Thermosialography – the temperature of the gland is measured.
Salivary gland biopsy - performed under ultrasound guidance.
Sialendoscopy.
Diagnosis of dacryoadenitis
If characteristic symptoms occur, you must visit an ophthalmologist who will conduct an examination. Diagnosis of the acute form of dacryoadenitis requires the following procedures:
- visometric and tonometric examination;
- biomicroscopy of the organ of vision.
Symptoms of the acute stage are usually severe, so the diagnosis is made quickly.
To diagnose chronic dacryoadenitis, additional measures are required:
- Ultrasound of the eyeball;
- magnetic resonance or computed tomography (to exclude a tumor of the eyelid or lacrimal gland).
Also, in case of chronic dacryoadenitis, in order to clarify the etiology of the inflammatory process, a chest X-ray is taken (this makes it possible to detect changes in the lung tissue), the Mantoux test and other studies.
Treatment with folk remedies
Traditional methods in the treatment process can only be used as auxiliary ones. It is advisable to use the following methods of traditional treatment:
- Rinsing the mouth - for this purpose, a solution of soda and salt can be used (1 teaspoon of salt and soda for 1 glass of water). It is also recommended to rinse the mouth with infusions of herbs - sage, oak bark, calendula, chamomile. To prepare the infusion for rinsing, 2 tbsp. l. raw materials should be poured into 3 liters. boiling water Leave for an hour and rinse your mouth several times a day. In case of purulent processes, rinsing is contraindicated.
- To stimulate salivation, it is recommended to consume lemon juice, cranberry juice, and chewing candies.
- 5 tbsp. l. pine needles pour 1 liter of water, bring to a boil, leave and take 50 ml 2 times a day.
Diet
Diet to boost immunity
- Efficacy: therapeutic effect after 3 weeks
- Terms: 1-3 months or more
- Cost of products: 1600-1800 rubles. in Week
During the treatment period, it is recommended to eat properly to strengthen the immune system. Sometimes doctors advise sticking to the so-called salivary diet. However, if a patient is diagnosed with calculous sialadenitis, then in this case it is necessary to carry out mechanical removal of stones, since nutritional correction will not help cure the calculous type of disease.
The salivary diet involves introducing the following products into the menu:
- Sauerkraut, sour berry fruit drinks, lemon juice, pickles.
- Citrus.
- Sour lollipops.
- Fresh vegetables.
- Juices from cabbage, carrots.
- Rose hip decoction.
You need to exclude from your diet foods that contribute to the formation of stones:
- Cheeses, cottage cheese.
- Tofu.
- Almonds, sesame.
- Fish.
- Milk.
Treatment of the chronic form
To cure chronic inflammation of the lacrimal gland, it is necessary to correct the underlying disease. Consequently, therapy is selected by several specialists - a venereologist, hematologist or phthisiatrician.
Physiotherapy may be prescribed, for example, UHF is a procedure that has an intense absorbable effect. If therapy does not bring results, the affected area is irradiated with x-rays.
In addition, for the treatment of chronic dacryoadenitis, medications necessary for the treatment of the underlying disease are prescribed. For example, if the disease develops against the background of tuberculosis, then the patient is prescribed medications by a phthisiatrician.