Adenophlegmon
Adenophlegmon is an acute purulent inflammation of the subcutaneous fatty tissue of an abscessing nature, closely associated with purulent processes in the regional lymph nodes (lymphadenitis). Adenophlegmon accounts for more than 21% of all maxillofacial pathologies; other localizations are much less common. The pathological process develops more often in children, is not gender specific, and is non-endemic. It is worth noting that scientists belonging to the domestic school of dermatology played a major role in the study of adenophlegmon. A. Abrikosov gave a coherent theory of the occurrence of adenophlegmon in 1938, and I. Rufanov supplemented and developed the theory of the pathogenesis of the disease in 1960. The relevance of this issue at the present stage is due to the severity of the purulent process, which affects newborns and preschool children and poses a real threat to their lives due to the development of septic complications. In adult patients, adenophlegmon can cause the development of sepsis and osteomyelitis.
Causes of adenophlegmon
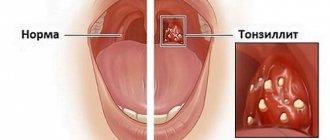
Purulent inflammation of the subcutaneous fat, like any other purulent inflammation, has a clear cause. This is an external or internal infection, most often with coccal flora. As a result of a decrease in the body’s defenses of an exogenous-endogenous nature (focal and perifocal infection, especially in the area of the tonsils, oral cavity, kidneys, previous illness, skin trauma, more often post-injection, pyococcal damage to the dermis), the anti-infective barrier of the lymph nodes decreases.
Typically, lymph nodes and lymphatic vessels, together with the venous system, ensure the natural outflow of fluid from tissues and organs. During inflammation, this plays a decisive role, since in the early stages of development of the process, lymph flow slows down, vascular permeability increases, conditions are created for the accumulation of microbes in the lymph nodes, where pathogenic flora is absorbed by the cells of the reticuloendothelial system, the remnants of microorganisms are broken down, and released into the circulatory system, where they die under the influence of antibacterial therapy. If inflammation increases, the lymphatic vessels thrombose, blocking the outflow, blocking the spread of the inflammatory process. Against this background, microbes from the lymph nodes leak into nearby tissues, causing inflammation in them and forming adenophlegmon.
Classification of adenophlegmon
Adenophlegmons are usually distinguished by the localization of the inflammatory process. The most significant in terms of severity and possible consequences:
- adenophlegmon of the lower jaw and chin is the most common option;
- adenophlegmon of the neck - a consequence of violations of personal hygiene of the oral cavity, auricle, and scalp;
- adenophlegmon of the groin area - the result of hypothermia;
- adenophlegmon of the axillary region - a consequence of infection of skin microtraumas;
- adenophlegmon of the parotid region is a septic complication.
Symptoms of adenophlegmon
Clinical manifestations of adenophlegmon are divided into general, characteristic of all varieties, and local, characterizing exclusively one or another form. General symptoms include a temperature reaction, a feeling of weakness, fatigue, lethargy, increasing signs of intoxication of the body, exacerbation of chronic foci of infection. Against this background, a tumor appears located next to the regional lymph nodes. It is dense to the touch, fluctuating in the center, painful on palpation. With further progression of the process, the tumor abscesses, opens, or septic dissemination of the process occurs. Often such a tumor forms at the injection site.
Symptoms corresponding to the type of adenophlegmon depend on the location of the process and have characteristics. Adenophlegmon of the submandibular region is preceded by dental intervention (for example, removal of a wisdom tooth), regional lymphadenitis. When adenophlegmon forms, pain is observed when swallowing, opening the mouth, and speech is impaired. Adenophlegmon of the neck is formed against the background of a general decrease in immunity, which leads to the activation and proliferation of pathogenic microbes that latently exist on the skin of the scalp and in the oral cavity, especially with errors in hygiene. The trigger for the development of the disease is the accumulation of a critical amount of bacteria, which transforms the latent process into the development of a focus of coccal infection.
The development of adenophlegmons in the groin is a consequence of an inattentive, irresponsible attitude towards one’s health. They arise as a result of periodic prolonged hypothermia, causing urethritis, cystitis, and inflammation of the pelvic organs. The resulting infection is so resistant to the therapy that inflammation occurs and abscess formation of the inguinal lymph nodes occurs. The outcome is often infertility.
How does APO manifest itself?
Adenophlegmon manifests itself with rapidly increasing signs of general intoxication of the body. Further on the neck, in the area where the submandibular lymph nodes are located, a tumor appears and is actively growing. This formation is painful on palpation and has a characteristic hyperemic focus in the center. Adenophlegmon is dense, this indicates the presence of fluid in its cavity (fluctuation). There are multiple small hemorrhages on the skin and mucous membranes located in close proximity to the tumor.
Untreated dental diseases are a common cause of APO
If adenophlegmon develops in children, they become tearful, weak, apathetic, refuse food and active games, and there is increased sweating. Against the background of APO, other diseases worsen in the child - diathesis, dermatitis, ARVI, etc. Sometimes adenophlegmon causes hyperthermia, the abscess can resolve outward (through the skin).
Diagnosis and treatment of adenophlegmon
The clinical picture and anamnesis of the disease are typical. Additionally, ultrasound of soft tissues and x-ray diagnostics are used to exclude osteomyelitis, tumors, and cysts. OBC, OAM, blood biochemistry, blood test for sterility are required. To prescribe etiopathogenetic therapy, culture of punctate purulent lesions on nutrient media is used, followed by determination of sensitivity to the antibiotic. Purulent inflammation is differentiated from phlegmon (choice of surgical intervention), tuberculosis, actinomycosis, osteomyelitis, periadenitis, inflammatory infiltrate, osteophlegmon. Purulent surgeons treat pathology.
Treatment of the disease is complex. The severity of the process dictates the need for urgent surgical intervention in a hospital setting. The phlegmon is opened and drained. The wound is treated in an open manner with washing, administration of antibiotics and enzymes, and dressings. Postoperative antibacterial, anti-inflammatory, and detoxification therapy is mandatory. They include means for general strengthening of the body (vitamin therapy) and increasing immunity (immunostimulants, immunomodulators). It is necessary to sanitize all foci of chronic infection. Prevention consists of timely diagnosis and treatment of chronic infections and strengthening the immune system. The prognosis with timely diagnosis and treatment is favorable.
Pathogenesis of Adenophlegmon:
The occurrence of adenophlegmon is a manifestation of the failure of the barrier-fixing function of the lymph node, in which filtration of lymph occurs, retention of microorganisms by reticuloendothelial cells and their phagocytosis with the transfer of information about their antigenic structure to the immunocompetent organs. When the outflow pathways from an inflamed lymph node are blocked, microorganisms and their metabolic products of an antigenic nature can penetrate through the lining of the lymph node into the surrounding tissue, causing inflammation in it. Clinical picture. From the anamnesis it is often possible to find out that the onset of the disease was preceded by trauma, inflammatory processes of the scalp, mucous membrane of the oral cavity, nose, and tonsils. Then, in the suprahyoid region, in the neck area, a moving, painful “ball” with clear contours appeared. As the “ball” grew larger, it lost its clear contours, and signs of the body’s general reaction such as headache, general malaise, and increased body temperature became more pronounced. Complaints and objective examination data, reflecting the local picture of the inflammatory process, depend on the localization of adenophlegmon. With a similar localization and prevalence of the infectious-inflammatory process, the disturbance of the general condition and the severity of the general reactions of the body in patients with adenophlegmon are usually less than in patients with phlegmon. The possible complications are the same as in patients with phlegmon: progressive spread of the infectious-inflammatory process to adjacent anatomical areas, spaces and vital organs (brain, its membranes, mediastinum), generalization of infection - development of sepsis, increasing cardiopulmonary, renal , liver failure as a result of infectious-toxic damage to these vital organs and systems.
Forecast
If you seek help from a doctor in a timely manner and complete the full course of treatment, the prognosis for APO is favorable. The use of antibacterial drugs in the initial stages of pathology can prevent the acute form of an abscess and reduce the risk of further complications.
So, adenophlegmon is an infectious-inflammatory process in fatty tissue, localized in close proximity to the lymph nodes. The favorite places for the tumor to be affected are the area under the lower jaw, near the ears, in the groin, and on the neck.
Treatment of the pathology is exclusively surgical, followed by drug correction of the general condition. With timely medical care, the prognosis for this disease is favorable; otherwise, adenophlegmon can provoke sepsis.
Symptoms of Adenophlegmon:
Sick children are characterized by adynamism, lethargy, lack of contact, severe weakness and sweating. In approximately a third of children with facial phlegmon, concomitant diseases are diagnosed: ARVI, bronchitis, pneumonia, acute otitis media, exudative diathesis, etc. The source of infection can be teeth, ENT organs, traumatic injuries, including post-injection injuries, due to violation of aseptic rules . The clinical picture of the disease in these patients is characterized by rapidly increasing symptoms of intoxication and the severity of local changes: the presence of diffuse swelling in one or several anatomical areas with pronounced hyperemia in the center. The swelling is painful, has a dense consistency with signs of fluctuation. Multiple pinpoint hemorrhages are observed on the skin and mucous membrane of the vestibule of the oral cavity, tending to merge in the skin area.
Features of children's APO
Children aged 3 to 7 years are at risk. The trigger for the development of pathology can be untreated acute osteomyelitis of the jaw. At an older age (10–14 years), adolescents are faced with adenophlegmon resulting from soft tissue injuries, followed by infection of the wound canals.
The list of main causative agents of the inflammatory process includes:
Treatment of tooth abscess
- staphylococci (white, golden);
- streptococci;
- diplococci, etc.
Important! If the baby suddenly begins to be capricious, begins to refuse to eat, complains of pain under the jaw, there is severe hyperthermia (sometimes the body temperature jumps sharply to 40 degrees) - this is a reason to immediately seek medical help from a pediatrician.
Diagnosis of Adenophlegmon:
Differential diagnosis is carried out with phlegmon in osteomyelitis (osteophlegmon), periadenitis, inflammatory infiltrate. The difficulty in making a diagnosis arises in the early stages of the process, when one nosological form (for example, periadenitis) in its dynamic development, in the absence of treatment, passes into another. The main thing in this case is to correctly determine the nature of the inflammation - purulent or non-purulent. Differential diagnosis with osteophlegmon is also extremely important, since the methods of surgical care for these types of phlegmon are different.
Treatment of Adenophlegmon:
Treatment of patients with adenophlegmons is based on the principles of emergency care. It is advisable to perform surgical interventions in all children under general anesthesia. If the source of infection is a decayed tooth, either its removal or opening of the tooth cavity is indicated. Then a skin incision is made and, if necessary, adipose tissue is dissected. In most cases, incision of the skin followed by pushing apart the soft tissues with the jaws of a hemostatic clamp is sufficient. Usually, the pus comes out under pressure and in large quantities. There is no need to inspect the abscess cavity. This is the main difference between intervention for adenophlegmon and that for osteophlegmon. In the case of the latter, the tissue must be cut up to the periosteum inclusive, and through this wound, the bone should be inspected and drained, with one end of the drainage installed on the bone. A bandage is applied to the wound. Dressings are carried out daily. General treatment is mandatory. The patient receives a complex of anti-inflammatory, antibacterial and, if indicated, detoxification therapy in age-specific dosages. Treatment is inpatient.
How to deal with the disease
After the diagnosis has been confirmed, the patient is sent to the hospital. Treatment of APO includes several successive stages:
- Surgical intervention. It is performed under local (adults) or general (children) anesthesia. In a situation where a tooth has become the source of infection, it is subject to extraction or depulpation (the dental canal is cleaned and a filling is placed). If necessary, an incision is made on the skin and the pus is released from the capsule - often such manipulations are not required, the contents come out on their own under internal pressure. As such, additional cleaning of the affected area is not carried out; the postoperative area is covered with a protective bandage (it is changed daily).
- Drug therapy involves taking anti-inflammatory, antibacterial, and restorative drugs.
- The wound is treated with local antiseptic solutions.
Treatment of APO is exclusively surgical - removal of pus from the capsule followed by the use of local antiseptics and systemic anti-inflammatory and antibacterial drugs. At home, in addition to traditional treatment, you can use several proven effective recipes. First of all, the action of the following compositions is aimed at strengthening the body's defenses and improving the general well-being of the patient.
Take 100 g of dry St. John's wort and 50 g of propolis, pour in 300 ml of vodka (medicinal alcohol). The mixture is poured into a glass container and sealed tightly. The medicine is infused for 7 days in a cool, dark place, filtered. When ready, the tincture is used for rinsing the mouth (the procedure is carried out at least 6 times a month, proportions - 20 g / 100 ml of warm water) and therapeutic compresses.
Compilation of anamnesis, analysis of complaints, visual examination of the patient and assessment of the results of clinical studies are components of the diagnosis of adenophlegmon
A few tablespoons of crushed dry eucalyptus leaves are poured into a thermos and steamed with boiling water and left for several hours. It is recommended to take a third of a glass of this infusion at least 4 times a day before meals. Burdock leaves are washed under running water, finely chopped, mixed with sour cream (2:1). The finished mass is applied to the affected area and left for half an hour. Manipulations are carried out daily.
User Questions (6)
- Evgeny 2018-03-01 21:49:07
When I fell on the glass, I cut my jaw. At the hospital the cut was stitched up. But after 2 days it became bad, they sent me to surgery, they opened the wound, and it was discovered that the salivary gland was affected. They diagnosed phlegmon. U... read the answer >> - Olga 2018-02-03 13:54:20
Hello! After the removal of the lower wisdom tooth, facial phlegmon formed, I was operated on. The incision healed normally, but a month later a small rash appeared in the place where the phlegmon was, in some places... read the answer >> - Irina 2017-02-17 17:40:18
Hello, after the removal of the seventh tooth on the lower right, a phlegmon formed, I spent a week in surgery, today I was discharged home, but there was a lump under my chin, they didn’t open it, they dropped methadone... read the answer >> - Alexey 2016-11-20 11:32:14
Hello. There was phlegmon of the lower jaw under the lingual. They had an operation. As of today, the stitches have been removed, a week has already passed. But in one place it does not linger and the Treasure stands out abundantly. Which... read the answer >> - Tatyana 2016-05-20 17:08:16
We had an autopsy of the phlegmon, but the tumor remained - the wound had not yet completely healed. tell me whether the ointment will draw out the liquid or be sure to consult a doctor (the person cannot walk, but they take him to the hospital... read the answer >> - Tamara 2015-12-03 02:16:33
Hello! I constantly have a clicking sound in my ear and it hurts to chew. They prescribed painkillers, UHF, etc., nothing helps, there is no dislocation on the X-ray, the dentist suspects “Arthrosis”... read the answer >>
Medical institutions you can contact:
Dental Office, network of dental clinics all addresses Orto Plus, dental office DiaGroup, medical center all addresses Biomed, dentistry Aristocrat, dental clinic SENDO, medical center Apollonia, dental office Zubok, dental clinic Doctor Gis, dental clinic Nor-Stom, dental office Dentline, dental clinic all addresses Delta, dentistry Denta-Lux, dental clinic DOCTOR, medical center Generation, medical center all addresses Diamant, dental clinic Favorite dentist, dental center Nika Spring, network of medical centers all addresses Dentist and I, dental office (Yunist ) SMILE, dental center
How to determine adenophlegmon
Adenophlegmon is an abscessive inflammatory process that occurs in the subcutaneous fatty tissue (characterized by the absence of boundaries of the purulent focus) and is localized in the area of the lymph nodes - most often the supramandibular, submandibular, chin and ear are affected.
Causes and pathogenesis
The formation of a purulent focus in the structure of the lymph node occurs due to the penetration of an infectious agent, a sharp weakening of immune defense and disruption of the barrier functions of the lymphatic system, caused by:
- previous infectious and inflammatory disease;
- severe vitamin deficiency;
- injury to soft tissues;
- neglect of the rules of asepsis when performing injections.
The development of an acute inflammatory process leads to the cessation of the outflow of lymphatic fluid; waste products of pathogenic microorganisms freely penetrate through the walls of the lymph node into nearby tissues and begin to form a purulent focus.
Symptoms and first signs
The early stage of adenophlegmon is characterized by :
- general malaise;
- rapid fatigue;
- decreased appetite;
- increased sweating;
- the appearance of a swelling in the area of the lymph node that is painful on palpation.
The progression of the purulent-inflammatory process is accompanied by an increase in body temperature, hyperemia of the affected area, the appearance of signs of fluctuation, damage to adjacent areas of subcutaneous fat and damage to vital organs.
Diagnostics
If adenophlegmon is suspected, the following diagnostic measures are carried out:
Diagnostics
An appropriate diagnosis is made by a specialist based on a visual examination, anamnesis and clinical studies. Treatment of adenophlegmon is carried out exclusively in a hospital setting under the supervision of a doctor. Adenophlegmon of the neck is a dense, hyperemic, inflamed formation (tumor), painful on palpation.
A patient who comes to the doctor for a consultation voices classic complaints of general malaise, weakness, and swelling under the lower jaw. Subsequently, doctors usually discover that there were symptoms of lymphadenitis (a dense ball of varying sizes is present in the area of the lymph nodes). The doctor notes the presence of infiltration, swelling, hyperemia and other signs of APO that are accessible to visual inspection and palpation.
Important! If the lower submandibular triangle is affected by a purulent-inflammatory process, patients experience dysphagia (difficulty swallowing), problems with speech, and discomfort when opening and closing the mouth.
Adenophlegmon, localized in the submandibular region, is the most common type of this disease
Laboratory studies demonstrate an increase in ESR (indicating the presence of acute inflammation in the body), an increase in the number of neutrophils and leukocytes. It happens that APO develops within a few weeks after the patient undergoes dental treatment.
The doctor has no complaints about the condition of the teeth and gums, but under the lower jaw, a small ball appears at first, and then increases in size, a dense ball, which is also painful on palpation. Often such patients are referred to an otolaryngologist, but he also does not find any respiratory abnormalities. The cause of the pathological process and pain syndrome in this case is the same adenophlegmon under the lower jaw.