Installation of implants is a surgical operation that is performed under anesthesia. Most often, local anesthesia is used, that is, eliminating the sensitivity of tissue in the area of the upcoming invasive manipulation. Since the anesthetic lasts for several hours, numbness after implantation is quite normal. It may be associated with swelling, which often accompanies the installation of artificial roots in the jaw. As a rule, the numbness goes away as soon as the effect of the drug wears off. But if sensory impairment persists several days after surgery, this may indicate the development of one of the complications.
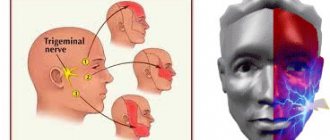
Trigeminal nerve injury
Prolonged numbness of tissues after implantation can also be caused by incorrect selection of the length of implants or their installation without taking into account the anatomical characteristics of the patient. In this case, damage to one of the processes of the trigeminal nerve is possible. Most often, when screwing in dental implants, the inferior alveolar nerve is affected. If it is damaged in the area of the lower lip, cheek and gums (up to the second molars), the following may occur:
- complete numbness of tissues;
- not disappearance, but a violation of sensitivity, without other unpleasant phenomena;
- a change in sensitivity, which is accompanied by an abnormal reaction to certain stimuli and other pathological symptoms.
If the lingual nerve is damaged during implantation, the following may also appear along with numbness:
- uncontrolled tongue biting;
- increased salivation;
- loss of taste;
- swallowing dysfunction;
- difficulties with pronouncing sounds.
If such symptoms appear and prolonged loss of sensitivity after implantation, you should contact the dentist who performed the operation.
Nerve damage during implantation: diagnosis, treatment, prevention
Damage to branches of the trigeminal nerve (eg, inferior alveolar, lingual, mental, or infraorbital) is a potential complication that can develop during the dental implant procedure.
Direct damage to the nerve fiber can be caused by injury, inflammation, or the result of an infectious factor. Most often, the branches of the trigeminal nerve are affected during anesthesia, flap separation, bone augmentation, osteotomy and direct installation of a titanium intraosseous support. Since the restoration of damaged nerve fibers is quite problematic, the best tactics for treating such complications is prevention. Therefore, it is extremely important for the doctor to understand the features of the histology and anatomy of the nerves of the maxillofacial region, and to be informed about the symptoms that most often accompany their lesions. Also, the clinician must take into account aspects of differential diagnosis in order to correctly establish the cause of the development of certain symptoms, based on which in the future he will have to carry out appropriate treatment. Treatment options for trigeminal nerve branch lesions include the use of various pharmacological agents, monitoring with physical therapy, or even removal of the problematic dental implant.
In this article we will discuss approaches to the treatment of dental patients with damage to the nerves of the maxillofacial area associated with the dental implantation procedure, as well as the main aspects of the etiology and pathogenesis of such pathologies in general.
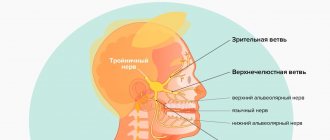
Anatomy and histology of the trigeminal nerve
The trigeminal nerve is the fifth and largest pair of cranial nerves, which consists of the following branches: the ophthalmic nerve (V1), the maxillary nerve (V2), and the mandibular nerve (V3). The mandibular nerve is the largest branch and innervates the lower lip, chin area, teeth, adjacent soft tissues, lower jaw and part of the external ear. The motor fibers of the mandibular nerve are not damaged during the implantation procedure because they arise from the main branch of V3 before exiting the mental foramen. The main structural unit of a nerve is the nerve fiber. The structure of V3 is dominated by myelinated nerve fibers. Each axon and Schwann cell is covered in connective tissue called the endoneurium. Groups of nerve fibers form bundles that are surrounded by epineurium. Damage to any part of the nerve bundle can lead to neurosensory impairment. The trigeminal nerve consists of 7000-12000 axons, and the number of bundles varies in different parts of the maxillofacial region. The inferior alveolar nerve (IAN) is polyfascicular (consisting of more than 10 fascicles), while the lingual nerve contains only a few similar nerve structures. Since the NAN is characterized by a large number of nerve bundles, its regenerative abilities are also significantly higher compared to the lingual nerve.
Types of nerve lesions
Lesions of the trigeminal nerve can be caused by compression, stretching, complete or partial disruption of the integrity of the nerve fiber. Damage may result in neurosensory changes in touch, pressure, temperature, and pain. Such pathologies significantly affect the patient’s comfort and ability to talk, eat, kiss, shave, apply makeup, brush teeth and drink normally. In addition, neurosensory disorders also affect the patient's ability to interact normally in society. Signs of these pathologies can be identified directly during surgery (if there is a pain symptom), or during long-term monitoring of the patient’s condition. To describe traumatic lesions of axons of varying degrees of complexity, the following terms are used:
- neurapraxia - a lesion in which the integrity of the nerve fiber is preserved, and the mechanism of injury is associated with stretching or impact such as blunt trauma; Sensitivity usually returns to normal within a few days or weeks.
- axonotmesis - damage to the nerve, in which the processes of its degeneration and regeneration develop, but the axon itself does not lose its integrity, and sensitivity is normalized over 2-4 months; however, sensitivity after recovery may be slightly less than before the intervention, and in some clinical cases it is characterized by accompanying dysesthesia.
- neurotmesis - damage to the nerve, in which there is a violation of its integrity, and the prognosis for the restoration of normal sensitivity is unfavorable.
The International Association for the Study of Pain has standardized nomenclature regarding traumatic nerve injuries. In particular, the definition of the term paresthesia, which was previously used to refer to loss of sensation, was changed. Current terminology provides the following definitions:
- paresthesia - a change in sensitivity without accompanying discomfort;
- dysesthesia - a change in sensitivity, which is accompanied by unpleasant sensations;
- anesthesia - loss of sensitivity.
To describe changes in neurosensory functions, terms such as allodynia (the occurrence of pain to stimuli that normally do not provoke pain), causalgia (the presence of persistent burning pain), hypoesthesia (decreased sensitivity to the action of stimuli), hyperesthesia (increased sensitivity to action) are also used. irritants).
When nerves are stretched or compressed, the perineurium protects the bundles from damage. However, lengthening the nerve by more than 30% can provoke structural damage. When the integrity of the nerve is completely disrupted, symptoms of anesthesia and a decrease in certain sensory functions develop. When the integrity of the nerve fiber is partially disrupted, various symptoms of damage, including dysesthesia, may be observed. It should be noted that the presence of persistent pain after surgery is not a criterion for determining the potential for complete restoration of the function of the affected fiber.
After damage to the peripheral nerve, Wallerian degeneration begins to develop, which continues for several weeks and even months. Axonal necrosis develops distal to the site of traumatic intersection. Degeneration in such cases is progressive and irreversible and lasts for up to 18 months. The ability of the affected nerve area to heal is influenced by factors such as the patient's general health, age, and type of injury. A key point in the process of nerve recovery after damage is the formation of scar tissue in the area of endoneurial tubules.
Evaluation of traumatic lesions of the trigeminal nerve
NAN is most often affected during the installation of dental implants. Signs of inferior alveolar nerve involvement include anesthesia, paresthesia, or dysesthesia in the skin, lower lip, cheek, and gums up to the second molar site. Patients with damage to the lingual nerve are characterized by uncontrolled salivation, biting the tongue, a feeling of heartburn, loss of taste, changes in speech and swallowing function, numbness of the mucous membrane and tongue. Both during and after surgery, all potential symptoms of sensorineural impairment should be documented. Areas of altered sensitivity are mapped (both by location and area of the affected area). Thus, it is possible to monitor changes in all parameters in the future, and determine whether the patient needs microsurgical intervention or not. To identify and determine the extent of disorders, both objective and subjective diagnostic tests are used, which are conventionally divided into mechanoceptive (response to mechanical stimuli and compression) and nociceptive (sensation of pain).
Mechanoceptive tests include static touch with a soft brush, two-point discrimination, and determination of the direction of brush movement. The sensation of a needle prick and the recognition of thermal stimuli are classified as nociceptive diagnostic procedures. To compare indicators, not only the affected area is always diagnosed, but also a symmetrical area, thus accurately identifying the fact and degree of neurosensory impairment. If the patient complains of loss of taste, a cotton swab moistened with salt or sugar is used for diagnosis.
Prevalence of traumatic nerve injuries
After implantation, permanent loss of sensitivity in the lip area due to traumatic damage to nerve fibers is observed in 0-36% of clinical cases. However, these data can be considered somewhat outdated and do not correspond to the approaches of modern implantological practice. After all, earlier during operations, dental surgeons more often used vestibular incisions, which caused sensitivity disorders to develop. Today, during the installation of dental implants, midline mucosal incisions are made along the top of the residual ridge, and the entire procedure is pre-planned, taking into account the data obtained after a computed tomographic examination. Thus, it can be assumed that the prevalence of nerve fiber damage due to implantation is significantly less than 36%.
Dannan et al reported that the incidence of nerve damage with implantation was as high as 2.95% (5 of 169 patients treated) in cases of temporary neurosensory changes, and 1.7% in cases of irreversible implant-associated neuropathies. Another study found that the incidence of nerve damage after maxillofacial surgery was 2.69% (42 of 1559 patients), with an even lower percentage of irreversible neurosensory damage, but the exact number was not specified in the study. . In the author's opinion, however, even such rates of implant-associated damage to neural structures are too high for clinical practice. Transient loss of sensation in the lip can often be associated with swelling, which is observed during the first two weeks after surgery.
Traumatic damage to the lingual nerve during surgical procedures
The lingual nerve in the region of the mandibular molars passes through the soft tissues on the lingual side of the jaw. Sometimes the nerve is located coronal to the surface of the bone tissue and is tightly adjacent to the cortical bone plate on the lingual side. Therefore, any surgical interventions must be carried out very carefully in this area. After removal of the third molars of the mandible, lesions of the lingual nerve are observed in 0.5-2.1% of clinical cases. Traumatic disorders of the lingual nerve during dental implantation are not a common phenomenon and are recorded quite rarely. To prevent such complications when installing dental implants, the following rules should be followed: only intrasulcular incisions can be made without releasing incisions and flap separation from the lingual side; During flap separation, it is necessary to avoid overstretching it and maintain a safe distance when performing osteotomy. 90% of all recorded cases of neurosensory changes associated with lesions of the lingual nerve resolve within 8-10 weeks after surgery.
Preoperative planning: prevention of traumatic nerve injuries
To prevent most complications associated with the installation of dental implants, it is necessary to ensure careful planning of the surgical intervention. Using the capabilities of computed tomography and surgical templates allows you to avoid unexpected outcomes of iatrogenic intervention. When installing a dental implant, a minimum of 2 mm of bone thickness must be left between the apical part and the coronal part of the mandibular nerve canal. In addition, it is important to adhere to the specified osteotomy length and strictly follow the bone preparation protocol. The presence of 2 mm of bone thickness also avoids excessive bone compression in the area of the nerve after installation of a titanium intraosseous support (photos 1 - 2).
Photo 1. The implant was installed in the area of the 30th tooth. After the anesthesia wore off, the patient began to complain of parasthesia in the area of the right lip and chin. On an x-ray taken immediately after implantation, there are no signs of implant penetration into the mandibular nerve canal.
Photo 2. The implant was installed 10 years ago, and during this time the patient was able to adapt to changes in sensitivity. The CBCT image shows that the implant in the area of the 30th tooth is much closer to the nerve canal than previously thought.
If necessary, to ensure the safety of the intervention, short dental implants can be used. It is also important for the doctor to be familiar with the absolute length of all drills that are used during the manipulation, since failure to take these parameters into account can provoke excessive deepening by more than 0.4-1.5 mm relative to the selected safe boundary. To control the deepening into the bone tissue, it is also recommended to use special stoppers. However, the physician must understand that neither the thickness nor the density of the bone tissue over the area of the nerve ensures the safety of its condition during the osteotomy procedure, therefore applying too much force and pressure during the preparation of the bone tissue is strictly prohibited. Finally, it should be noted that up to 50% of lawsuits related to nerve damage after implantation are caused by the lack of informed consent on the part of the patient, which the doctor must obtain before surgery. It is also a good idea to assess the patient’s neurosensory parameters before the intervention in order to compare them with the data that will be obtained after implantation.
Local anesthesia: a potential cause of nerve damage
Traumatic lesions of the mandibular and lingual nerves can occur during anesthesia due to needle trauma, hematoma, and exposure to the components of the anesthetic solution. The mechanisms of such lesions are still quite unexplored. One retrospective study estimated the incidence of nerve injury during anesthesia to be between 1/26,762 and 1/160,5716 cases, while Haas and Lennon predicted the incidence of such complications to be 1/785,000. Other data suggest that the prevalence of short-term transient lesions of the mandibular and lingual nerves as a result of anesthesia ranges from 0.15% to 0.54%. Whereas cases of the development of permanent changes in sensitivity of the same etiology are quite rare, with a prevalence of 0.0001-0.01%. After performing mandibular anesthesia, 3-7% of patients experience electrical sensations that resolve spontaneously over time. However, when the clinician notes that the patient has overreacted to the needle insertion, the needle may need to be withdrawn and repositioned slightly. Methods for the treatment or prevention of nervous complications associated with the anesthesia procedure have not yet been developed. Between 70% and 89% of anesthesia-related neurosensory lesions develop in the region of the lingual nerve. This trend can be explained by the fact that the lingual nerve consists of only a few bundles, while the lower alveolar nerve consists of a huge number of them, which, in turn, increases its potential for regeneration. From a geometric point of view, everything is explained much more simply: the size of the needle is on average 0.45 mm, while the diameter of the lingual nerve is 1.86 mm, and the diameter of the inferior alveolar nerve is 3 mm.
Anesthesia-associated nephropathy most often develops after anesthesia with 4% solutions of articaine or pilocarpine. Compared to lidocaine, pilocarpine and articaine cause 7.3 and 3.6 times more neurosensory impairment. Garisto et al reported that in 4 of 9 studies, the complication rate was higher with prilocaine or articaine 4% solutions than with lower concentration anesthetic injections. According to the authors, local anesthesia with these drugs should be avoided in order to reduce the incidence of associated neuropathies after iatrogenic interventions. However, according to Malamed, the cases in which Arcticaine has demonstrated a greater association with neuropathies than lidocaine are anecdotal, and do not have sufficient evidence-based argumentation. Similarly, in 2013, after an extensive review of the literature, Toma and colleagues concluded that studies suggesting extreme neurotoxicity of articaine were retrospective in design, the data presented were at high risk of bias, and the findings should not be regarded as sufficient evidence. . The authors concluded that direct trauma to the nerve fiber is the predominant cause of neurosensory impairment, and the latter has little to do with the chemical toxicity of the anesthetics used. In general, there is disagreement in the literature on this issue; Therefore, clinicians should make decisions regarding the use of higher concentrations of anesthetics based on the conditions of each individual clinical case, while interpreting prior information and taking into account the recommendations of the drug manufacturers.
Osteotomy procedure for implantation
The osteotomy procedure should be performed using well-sharpened drills and abundant irrigation. Hypothetically, overheating of the intervention area during osteotomy can provoke traumatic nerve damage. The extent of bone necrosis caused by overheating is directly proportional to the preparation temperature under which iatrogenic intervention was performed.
Eriksson and Albrektsson summarized that performing an osteotomy at 47°C for 1 minute may provoke subsequent bone resorption. In cases of progressive resorption, given the shift in the position of the mental foramen, a transcrete incision is contraindicated; instead, it should be shifted to the lingual side. When placing implants anterior to the mental foramen, careful analysis of CT images should be performed, which may help detect the presence of a loop of mental nerve.
Flap separation procedures
As a rule, flap separation does not provoke any neurosensory disturbances, however, the doctor should still pay great attention when performing this iatrogenic intervention in the chin area. The doctor must clearly understand where the mental nerve exits the mental foramen, so that when separating the flap it does not cause damage to the nerve fiber.
Tooth extraction
Before extracting molars and premolars in the lower jaw for subsequent installation of dental implants, the relationship between the position of their roots relative to the course of the inferior alveolar and mental nerves should be carefully studied. Care should also be taken to curettage the sockets after resection, since periapical lesions may often be close to neural structures (Figures 3–4).
Photo 3. The patient sought help for pain in the area of the 31st tooth. The X-ray image shows signs of acute apical periodontitis.
Photo 4. The results of CBCT diagnostics indicate that the pathological focus is located near the nerve canal. The tooth was carefully removed, followed by careful curettage of the defect area.
Pharmacological therapy of neuropathies associated with the installation of dental implants
There is no clear opinion regarding which drugs are best to use in diagnosing traumatic lesions of the nerves of the maxillofacial area. Some authors prefer corticosteroids and nonsteroidal anti-inflammatory drugs (NSAIDs). It is worth remembering that the use of various pharmacological agents is relevant only if the integrity of the nerve fiber as a whole is preserved. In cases of sensory impairment after injection, the patient can be given dexamethasone 4 g/ml directly to the area of the injury, and after 3 days the dose of steroids can be increased. If a nerve is compressed or a fiber is injured during surgery, 1-2 ml of dexamethasone is administered intravenously, after which dexamethasone is prescribed orally for 6 days (4 mg, 2 tablets after meals for three days, then 1 tablet after meals for another three days). If the integrity of the nerve is compromised, steroids may be prescribed for a period of 5 to 7 days. Impaired sensitivity can be relieved by 800 mg of ibuprofen, which should be taken three times a day for 3 weeks. If neuropathy develops after removal of the implant, patients can also be prescribed 800 mg of ibuprofen three times a day and with the same frequency 500 mg of amoxicillin for 5-7 days. In parallel, 50 g of prednisolone is prescribed, reducing the dose by 10 mg every day (for 5 days). Post-traumatic neuropathy can be treated with low doses of antidepressants and antiepileptic drugs.
In combination with a pharmaceutical approach, Renton and Yilma recommend physical therapy interventions for patients with chronic neuropathy. The goal of such a treatment algorithm is to reduce the patient’s discomfort and help him get rid of pain. Bagheri and Meyer generally question the effectiveness of corticosteroids in the treatment of traumatic lesions of the inferior alveolar nerve, since the density of the bone tissue forming the nerve canal is so high that it is simply impossible for medications to reach their space. At this time, there are no results from clinical studies that confirm the feasibility and success of using corticosteroids or NSAIDs for traumatic neuropathies associated with the installation of dental implants.
When to refer a patient to a microsurgeon
Universal recommendations regarding when to refer patients with traumatic trigeminal neuropathies to a microsurgeon have not yet been developed. Some authors argue that the patient should be referred to a specialist immediately after noticing sensory disturbances after the implantation procedure. Other researchers recommend referral to a microsurgeon after 2, 3, 4, or even 6 months of monitoring if signs of traumatic neuropathy are observed during these months. Ziccardi and Zuniga recommend microsurgical intervention for up to 1 year after the implantation procedure, since the effectiveness of microsurgical correction noticeably decreases one year after the intervention. When determining the fact of traumatic neuropathy after implantation, the physician must determine whether the patient needs to be referred to a microsurgeon, or whether the situation can be improved with the use of various pharmacological drugs.
Sometimes explantation, or slight “unscrewing” of the implant from the bone, can help resolve the symptoms of traumatic sensory dysfunction. The results of individual studies indicate that the advisability of referral to a microsurgeon is justified only by stating the fact of a complete violation of the integrity of the nerve. When the doctor is sure that he did not violate the integrity of the bone canal of the nerve, then the disturbance in sensitivity can be caused by compression of the nerve fiber or an inflammatory effect. In such cases, a pharmacological approach to treatment can also help. Meanwhile, the doctor must understand that even if he did not perforate the main nerve canal, the nerve often has additional branches, the course of which is quite difficult to predict. The latter is possible only with a careful analysis of the data obtained after CBCT scanning, because two-dimensional radiographs provoke superimposition of individual anatomical structures, therefore, the prediction of possible traumatic nerve damage with their help is ineffective (photo 1-2).
In cases of discomfort after implant installation, if it can be confirmed that the intraosseous support is not located near the nerve canal, treatment algorithms are variable. Bagheri and Meyer suggest monitoring for 3 to 4 months to see if sensory improvements are observed before referring the patient to a microsurgeon. The authors also claim that if the position of the implant is too close to the nerve, the level of compression of the latter can be reduced by a slight reverse movement of the implant. Other researchers suggest explanting the intraosseous construct within 36 hours and immediately prescribing steroids if the patient exhibits signs of neurosensory impairment after surgery.
Khawaja and Renton described four clinical cases of the development of sensory symptoms after the installation of dental implants, in which the intraosseous structure was not located near the nerve. However, upon explantation, the symptoms of neurosensory disorders resolved quite quickly in two of the four patients. Interestingly, positive dynamics were observed in patients whose implants were removed within 18 and 36 hours, and residual symptoms were observed in patients whose explantation was performed 3 and 4 days after surgery.
Renton, Dawood and colleagues suggest that patients with such symptoms should be monitored for no more than 3 months, since after this period the risk of developing neural changes outweighs the potential success of microsurgery. Ziccardi and Steinberg in their review article recommend initial monitoring for 1 month, and if symptoms improve, continue to monitor the patient. If the symptoms do not improve or worsen, it is necessary to refer the patient to a microsurgeon. Research results indicate that patients operated on for neurosensory impairment 6-8 months after implantation have the same level of success as patients operated on in a shorter period after iatrogenic intervention. According to the authors, earlier intervention is possible and more effective, but there is no evidence to support this assumption. In addition, microsurgery is not indicated in cases of only minor neurosensory changes, since the risk from the intervention itself in such cases exceeds the predicted success rate. There is also a 12-week waiting period - on average, this is the amount of time a doctor needs to decide whether to refer a patient for microsurgical surgery.
It is logical that in cases where patients have acute pain, it is not necessary to wait 12 weeks. Before arguing for certain approaches to treatment, the doctor must objectively compare X-ray data and clinical symptoms, and then take into account all possible medico-legal aspects of the violations.
Surgical restoration of damaged trigeminal nerve
There are specific reasons that justify the need for microsurgical restoration of the damaged trigeminal nerve, and contractual factors that determine the prognosis of this manipulation. Ziccardi and Zuniga formulated the following list of reasons that justify referral of a patient to a microsurgeon: sensory impairment that persists for more than 3 months and interferes with the patient’s normal life activities, confirmation of the fact of nerve transection, lack of improvement in signs of hypoesthesia, development of pain after implantation. After microsurgical correction is performed, a number of factors influence the success of it: the waiting time after implantation, the type and volume of the lesion, the degree of vascularization of the affected area, the experience of the surgeon, the method of harvesting and preparing the graft, the presence of tension in the repair area, the age and general health of the patient.
In fact, microsurgical restoration of the branches of the lingual and inferior alveolar nerves is possible. However, the success rate of such manipulations is very variable - on average, researchers indicate only 50-59.4% effectiveness of such treatment, and in only two studies the results of the intervention reached levels of 81.7% and 63.1%. In all the studies conducted, the number of subjects is quite small, so it is methodologically impossible to compare the final results of such studies. However, 50-60% of patients after microsurgical correction show signs of improvement in neurological impairment. Ziccardi and Zuniga warn that patients with severe sensorineural impairment should be informed that full rehabilitation is virtually impossible. Also, many researchers indicate that the effectiveness of microsurgical procedures in cases of treatment of anesthesia, dysesthesia and spontaneous pain is exaggerated. To summarize, microsurgical correction can help individual patients, but the level of predictability of the results of such treatment is ambiguous. Thus, the best treatment for neurosensory disorders associated with implantation is their prevention.
Conclusion
A common dilemma in clinical practice is: if an implant is successfully osseointegrated but causes mild paresthesia without pain, what should be done with it? After all, explantation may not always help resolve symptoms, and retention of the implant in the bone with actual nerve damage can trigger the development of neuroma. The latter is formed as a result of excessive healing of the area of the damaged nerve and hyperplasia of adjacent tissues, and very often requires subsequent surgical removal. The decision to choose a possible treatment method should be made together with the patient after a thorough discussion of all possible options, and before starting rehabilitation, the patient must formally confirm his consent by filling out a special written form.
Authors: Gary Greenstein, DDS, MS Joseph R. Carpentieri, DDS John Cavallaro, DDS
Helping the patient with numbness after implantation
During a consultation regarding the loss or disappearance of sensitivity after installation of an implant, the dentist first of all finds out the cause. To do this, a diagnostic study is carried out, which makes it possible to determine the type and degree of damage to the nerve fibers. Then a set of therapeutic measures is prescribed.
If therapy begins at an early stage of development of disorders, sensitivity can be restored more quickly. The rehabilitation program for each patient is drawn up individually, with the participation of a dentist, neurologist and physiotherapist.
Treatment usually includes medications and physiotherapeutic procedures, such as acupressure, acupuncture, electrophoresis, and ultraphonophoresis.
Causes of paresthesia
Jaw numbness after wisdom teeth removal is a fairly common complication. It is due to the location of the “eights”. Their roots are located next to the jaw nerves, so during surgery the latter are often damaged, which leads to loss of sensitivity. Most often, paresthesia occurs:
- with long curved roots of the removed dental unit,
- severe bleeding during surgery,
- damage to the alveolar process.
Patients at increased risk of paresthesia after surgery include:
- over 30 years old,
- with a history of nerve ending injuries,
- endocrine diseases,
- neuralgia.
How to treat numb gums
If the patient's gums are numb, it is necessary to begin treatment early. The problem requires an integrated approach, since it is important to establish the cause of its occurrence.
The medications that are most often used if the gums are numb include:
- ► Antibacterial drugs. To eliminate pathogenic microflora in dentistry, Amoxiclav or Clindamycin are used. Preference is given to tablet or injection forms of release. The average duration of treatment is 7-14 days.
- ► Local antiseptics. They are used in the form of an ointment, gel or rinse solution.
- ► Non-steroidal anti-inflammatory drugs. The drugs reduce pain and tissue swelling. Nonsteroidal anti-inflammatory drugs are often taken for two weeks. The doctor selects medications individually.
- ► Traditional methods. A decoction of chamomile or calendula has a pronounced anti-inflammatory effect, which restores tissue sensitivity if the gums are numb. However, traditional methods can only be used on the recommendation of a dentist.
If there is no effect from the drug therapy, surgical intervention is prescribed, which is aimed at removing purulent masses or the implant. This will improve the patient's condition and prevent the spread of infection to other organs and tissues.
At the recovery stage, when the gums become numb, physiotherapeutic procedures are used:
- ► laser therapy
- ► dynamic current treatment
- ► UHF therapy
- ► electrophoresis
Complications after local anesthesia
The human factor plays a big role in dental procedures. Often, the inexperience or carelessness of a specialist leads to serious consequences.
General complications that arise during local anesthesia in dentistry can be of different nature:
- Discomfort at the needle insertion site. This is due to the drug being administered too quickly or too slowly.
- Hematoma at the injection site. The occurrence and growth of a hematoma indicates problems with blood vessels or an incorrect choice of the needle insertion site.
- Allergic reactions. Despite the fact that reactions to drugs are determined before anesthesia, cases of severe allergies to the composition of the anesthesia are not uncommon, especially if it consists of two or more components.
- Inflammation of the gums, development of infection. This case suggests that several mistakes were made during the procedure, as a result of which bacteria entered unprotected tissue and caused inflammation.
- Numbness of the facial muscles. The symptom is often complicated to the point of paresis, lack of control over facial expressions, inability to close lips, and sagging areas of the face.
Why does my upper lip go numb?
Physiological and cosmetic reasons
The appearance of the symptom is provoked by eating too cold or too hot food.
Numbness can also be a consequence of previous irritation of the upper lip from pepper or hot spices. At the same time, similar sensations are observed on the tongue and oral mucosa. The symptoms quickly disappear after stopping contact with the product. At sub-zero temperatures, strong winds, and high humidity, lips easily become chapped and crusty. Crusts impair the perception of tactile stimuli by nerve receptors, so their formation is accompanied by a feeling of numbness, which is complemented by a feeling of tightness due to a decrease in the elasticity of the skin, and the appearance of cracks.
In women, a decrease in lip sensitivity can be explained by individual intolerance to cosmetics (lipstick, lip gloss). Local itching, burning, and signs of skin irritation are possible. In some cases, the symptom is caused by an incorrect tattooing procedure or errors in lip care in the first days after manipulation.
Dental pathologies
One of the most common causes of numbness in the upper lip is diseases of the teeth and gums. The symptom is especially noticeable in severe inflammatory processes, accompanied by severe swelling of the oral mucosa and soft tissues of the face. It is provoked by gumboil, periodontitis, and gingivitis. In addition, numbness of the lip is observed after dental procedures performed under local anesthesia.
Trigeminal nerve injury
Isolated numbness of the upper lip rarely develops and is caused by trauma to the small branches of the n. maxillaris for bruises and open wounds of this anatomical area. A more common sensory disorder, simultaneously covering the upper part of the cheek, the side surface of the face, the outer corner of the eye, and the lower eyelid, is caused by damage to the trunk n. maxillaris, which is the second branch of the trigeminal nerve. It is found in fractures of the upper jaw, zygomatic bone, and compression by tumors.
Numbness of the upper lip
Migraine with aura
In patients with migraine with aura, an attack of cephalgia may be preceded by a transient loss of sensitivity in the hand, spreading to half the face and upper lip. Subsequently, the attack proceeds as usual. There is a throbbing or pressing pain in half of the head, nausea, slight dizziness, high sensitivity to bright light, loud sounds.
Cerebrovascular disorders
Numbness of the upper lip and other parts of the face and body is part of the clinical picture of a transient stroke or stroke. The symptom occurs against the background of headache, weakness, nausea, vomiting, vegetative-vascular manifestations (trembling, sweating, hot flashes), short-term disturbance of consciousness. Hemiparesis, decreased strength of certain muscle groups or one limb, facial asymmetry, and speech impairment are possible.
Hypoglycemia
Numbness of the lip is sometimes detected in patients suffering from severe diabetes mellitus; it develops as a result of severe hypoglycemia when using too high doses of insulin or poor diet. Combined with pallor, sweating, tachycardia, hand tremors. There are feelings of fear, excitement, followed by drowsiness, confusion, and fainting. Without help, coma is possible.
Quincke's edema
Numbness is caused by rapidly increasing swelling of the eyelids, cheeks, upper and lower lips. Quincke's edema forms against the background of an acute allergic reaction upon contact with pollen, animal hair, food, and other allergens. May be a consequence of pseudo-allergy. The condition develops suddenly within a few minutes, less often – hours. Hypoesthesia is often combined with skin itching, lacrimation, the appearance of copious nasal discharge, and difficulty breathing.
Herpes zoster
The cause of the pathology is the virus that persists in the body and causes chickenpox. Shingles symptoms may appear many years or even decades after the viral infection. The upper lip, as well as other parts of the face, become numb due to trigeminal neuritis. Typically, simultaneous involvement of the intercostal nerves, a rash along the affected nerve trunks.
Multiple sclerosis
The disease often manifests itself as weakness in the legs, combined with sensitivity disorders. Numbness and paresthesia are detected in the face, upper lip, torso, and limbs. There is a high probability of developing optic neuritis with reversible vision loss. Subsequently, with multiple sclerosis, paresis, symptoms of cerebellar damage, pyramidal disorders, and dysfunction of the pelvic organs are observed.
Pernicious anemia
The disease is caused by a disorder of hematopoiesis due to a deficiency of vitamin B-12. Manifested by weakness, tachycardia, dizziness, pale skin, puffiness of the face. Possible hypoesthesia of the upper lip, other areas of the face or limbs, and gait changes associated with neurological disorders. A characteristic sign of pernicious anemia is a “lacquered tongue.”
Neuroses
Loss of sensation in various parts of the body most often occurs in patients with hysterical neurosis. The patients’ complaints do not fit into the picture of a specific somatic pathology and are distinguished by pretentiousness and unusualness. Numbness of the upper lip is also sometimes seen in people with anxiety disorders. It may be part of the clinical picture of a panic attack or occur when the level of anxiety increases.