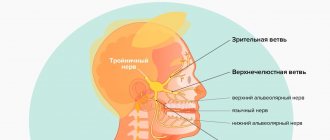
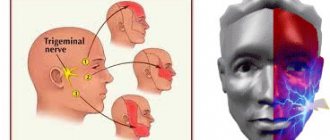
Trigeminal neuropathy is a lesion of the trigeminal system, which is characterized by changes in the interstitial tissue, myelin sheath, axial cylinders and is manifested by pain, paresthesia and sensitivity disorders in the areas of innervation of its main branches. If the mandibular nerve is involved in the pathological process, chewing function is impaired.
Among the etiological factors of trigeminal neuropathy are the following:
- infectious (malaria, viral hepatitis, syphilis, tonsillitis, sinusitis);
- iatrogenic (as a consequence of destructive therapy);
- traumatic;
- ischemic;
- intoxicating.
Most often, neuropathy of individual branches of the trigeminal nerve is determined.
Neuropathy of the inferior alveolar nerve occurs during infectious diseases, diffuse osteomyelitis, dental procedures (introduction of an excess mass of filling material behind the apex of the tooth in the treatment of premolars and molars of the lower jaw, traumatic extraction of teeth, especially the third lower molars, performance of mandibular anesthesia), toxic periodontitis.
Clinic.
The leading symptoms are pain and numbness in the area of the lower jaw, chin, gums and lower lip. An objective examination reveals loss or reduction of all types of sensitivity in the gum area of the lower jaw, lower lip and chin on the affected side. In the acute stage, painful contraction of the jaws (trismus) in combination with paresis of the masticatory muscles can be observed.
In dental practice, sometimes there is acute toxic-traumatic neuropathy of the lower alveolar nerve, the mental one, which occurs when filling material gets into the mandibular canal during the treatment of pulpitis of the first and second premolar on the lower jaw. During canal filling, the patient acutely experiences very intense pain in the lower jaw with numbness of the lower lip and chin. If such a situation arises, emergency measures are taken - decompression of the canal: dexamethasone 8 mg + 5 ml of 2.0% aminophylline solution + 20 ml of 40% glucose solution intravenously. At the same time, diphenhydramine 1 ml intramuscularly and furosemide 40 mg intramuscularly are prescribed. Subsequently, agents are used that improve microhemocirculation (nicotinic acid, pentoxifylline), as well as neuroprotectors (nootropil, cerebrolysin, actovegin), desensitizing drugs (diphenhydramine, suprastin, diazolin).
What is mandibular nerve injury?
By this concept, dentists mean injury to one of the nerves:
- chin;
- lingual;
- alveolar.
Types of injuries include sprain, compression, crushing and rupture - partial or complete. The cause of the stretching is the long-term retraction of the mucoperiosteal flap, which is created by an implant of greater length than necessary. Crush injuries and compression are caused by needle injuries during the administration of anesthesia. Rupture occurs in two cases: when cutting the mucosa or during preparation of the hole for the implant.
Extraoral access
Extraoral anesthesia of the inferior alveolar nerve is carried out by three main methods: submandibular, subzygomatic and retromandibular.
With the submandibular method of anesthesia, the syringe needle is inserted into the skin under the inner surface of the lower edge of the jaw at a distance of 1.5 cm from the angle. The needle moves along the bone at the level of the posterior edge of the branch by 3.5-4 cm. The anesthetic depot of 1 ml created in this way helps to block the inferior alveolar nerve. Blocking the buccal and lingual nerves is achieved by moving the needle an additional 1 cm forward while adding 1 ml of anesthetic. The needle is moved 4 cm in the direction from the lower edge of the jaw, and an anesthetic solution is injected into the tissue at the same time. Additional movement of the needle to the area of the lingual and buccal nerves is due to the need to anesthetize the intervention zone of the three nerve areas.
This method of pain relief is also applicable if the patient’s neck is shorter than usual. The syringe is attached to the needle after it is injected at the level of the mandibular foramen. The thing is that the syringe itself creates a barrier to the movement of the needle to the bone level.
The subzygomatic approach, or Bershe Dubov approach, is characterized by inserting a needle into the skin. The injector is inserted at an angle of 90 degrees to its surface under the lower edge of the zygomatic arch, and a couple of centimeters from the base of the tragus of the auricle. Advancing the needle no deeper than 3-3.5 cm allows you to reach the inner surface of the marginal pterygoid muscle. Two mm of anesthetic substance in this case will be enough. Blocking of the lower alveolar, lingual and buccal nerves occurs after 10 minutes, and complete elimination of the contracture of the lower jaw is observed a little earlier.
The last option for extraoral anesthesia of the inferior alveolar nerve is a puncture of the gland located behind the ears. With this method of access to the site of dental interventions, there is a risk of touching the carotid artery, or even a branch of the facial nerve. Hence the rarity of its use, but it still exists as an anesthesia option.
Causes and prevention of mandibular nerve injuries
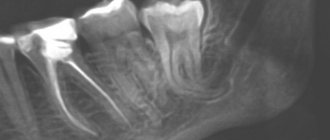
The only cause of such damage is considered to be medical errors. Since in preparation for implantation, X-rays of the jaw are taken, which the doctor must carefully study so that when choosing an implant and a place for it, he does not injure the nerve, the injuries are caused by his unprofessionalism or negligence.
Damage to the mandibular nerve most often occurs when:
- improper administration of anesthesia - needle injury;
- choosing an implant that is too long;
- damage by an instrument - when preparing the site for the implant.
The only way to avoid such an injury is for a doctor to responsibly approach the stage of preparation for surgery, carefully studying the condition and structure of his patient’s jaw. The only way of prevention for the patient is to choose a trusted clinic and a highly qualified doctor. Specialists at the Implantmaster clinic have been able to reduce the number of injuries of this kind to 2%, since they carefully study three-dimensional photographs of a person’s jaw before implantation, and can correctly assess the condition of the bone tissue, the location of nerves and blood vessels, and select the optimal size of the implant.
Basic techniques
On the lower jaw:
• Mandibular
• Buccal nerve anesthesia
• Mental
• according to Go-Gates
• according to Akinosi
On the upper jaw:
• Posterior superior alveolar nerve anesthesia
• Incisal
• Palatal anesthesia
• Infraorbital
• Maxillary nerve
Our team of doctors
Maxillofacial surgeon, Implantologist
Bocharov Maxim Viktorovich
Experience: 11 years
Dental surgeon, Implantologist
Chernov Dmitry Anatolievich
Experience: 29 years
Orthopedist, Neuromuscular dentist
Stepanov Andrey Vasilievich
Experience: 22 years
Endodontist, Therapist
Skalet Yana Alexandrovna
Experience: 22 years
Orthopedic dentist
Tsoi Sergey Konstantinovich
Experience: 19 years
Dentist-orthodontist
Enikeeva Anna Stanislavovna
Experience: 3 years
Symptoms and stages of damage
The symptoms by which this complication can be recognized are as follows:
- numbness of parts of the head - tongue, lips, chin, cheeks, etc.;
- biting lips and tongue;
- choking while eating or drinking;
- profuse salivation.
All this creates a number of inconveniences for the patient: it makes it difficult to eat and talk, disrupts facial expressions, and also prevents men from shaving and women from applying makeup. The severity of this injury is determined by its degree: a minor one goes away on its own or with the help of drug treatment, a severe one leads to irreversible processes of nerve degeneration and is not curable. Damage to the mandibular nerve, the symptoms of which the patient observes, requires immediate consultation with a doctor - only a specialist will be able to determine its extent and provide timely assistance.
Dentists distinguish the following stages of this implantation complication:
- minor - neuropraxia;
- more severe, but partial damage - axonotmesis;
- a serious injury that leads to complete loss of sensitivity - neurotmesis.
Clinical algorithm for determining post-traumatic neuropathy
Trigeminal Neuropathy Assessment Questionnaire
Important! Severe pain experienced during treatment may indicate a possible nerve injury.
- History of the initial onset of pain.
- Development of pain.
- Duration of pain.
- History of regular pain SOCRATES (Site, Onset, Character, Radiation, Associated signs, Timing, Exacerbating and relieving factors, Severity) - Localization, Occurrence (frequency of attacks), Character, Irradiation, Associated symptoms, Duration, Exacerbation and relief factors (what intensifies and relieves pain), severity of pain.
- Psychological screening.
- Functional screening (impact on daily life).
Mechanosensory tests (mapping the affected area)
A protocol for examining the dermatome to assess the extra-oral mechanosensory function of the alveolar branch of the trigeminal nerve.
Dermatomes are segments of skin into which the entire surface of the human body is divided in connection with its innervation by various roots of the spinal cord, in this case the trigeminal nerve.
Figure 7. Dermatomes of the branches of the trigeminal nerve
1. Logging the affected area.
Using surgical forceps, move from the normal to the neuropathic (changed) area, warning the patient that there may be increased sensitivity and/or decreased sensitivity. Mark an area on the patient's face with marker marks and take a photo. Assess the % or area of the extra-oral dermatome that is affected by neuropathy.
2. Recording the assessment of subjective sensation.
Press the surgical forceps or probe firmly (but not painfully) against the patient's arm several times at intervals (5 times per minute), explaining that this is a "normal" subjective rating of function on a scale of 10 out of 10. Press with the same pressure on the unaffected side of the face or tongue and repeat the stimulation, explaining that it should be 10 out of 10. Then remove the forceps or probe and explain that the missing stimulation is 0 out of 10. Only then repeat the same actions in the area of neuropathy that you have already confirmed and marked with markers labels, and ask the patient to report the stimulus level out of a possible 10 (if >10 = hyperesthesia and <10 = hypoesthesia). This test should be repeated in different areas of the neuropathy (lip border, lip skin, chin, tongue, etc.)
3. Recording the light touch assessment
To assess light touch thresholds, it is recommended to use a frayed cotton swab, repeating touches at intervals of 5 times per minute. First on the unaffected side and then repeating on the affected side, ask the patient to report the differences. If the patient is experiencing numbness, then the stimulation will have a reduced threshold for detecting light touch, however, if the patient suffers from hyperesthesia and possible allodynia (pain to touch), then this test can be very uncomfortable and irritating.
Dermatomal Involvement Map Interpretation and Neuropathy Assessment —Does the area of neuropathy correspond to the dermatomal area in which surgery was performed? — Dynamics of the area of the involved extraoral and intraoral area when mapping neuropathic areas (criterion reliability is low)
Important! Localized sensory neuropathy is not always present in patients, but there is almost always an area of abnormal sensation, and the patient's maximum pain is associated with the area of sensory deficit, that is, suffering from a combination of pain, numbness and altered sensation. This is an important diagnostic distinction for sensory neuropathy.
Subjective function
- Is neuropathy hyperesthesia or hypoesthesia?
- Thermal allodynia test is the occurrence of pain when exposed to heat or cold. Thermal allodynia, especially cold allodynia, is a feature in patients with trigeminal nerve damage.
- Thermal hyperalgesia test. Increased pain that occurs after a weak stimulus.
- Test "Direction of movement". The patient closes his eyes, the doctor uses a soft brush to determine the patient's ability to detect both the sensation and the direction of movement of the brush.
- Test for sensitivity to temperature stimuli. A cotton swab with cold test spray and a dental mirror handle heated to 43 - 45 ° C are used to determine the patient's ability to feel cold and heat. Alternatively, test tubes can be filled with hot (43 -45 °C) water and cold water.
There are WHO recommendations regarding which parameters of peripheral sensory consequences should be taken into account to predict the results of microsurgical restoration of a damaged sensory nerve. Zuniga JR and Yates DM adapted the recommendations to trigeminal nerve lesions. More details here: Zuniga JR and Yates DM Factors Determining Outcome After Trigeminal Nerve Surgery for Neuropathic Pain. J Oral Maxillofac Surg 2016 Jul;74(7):1323-9.
Today, a guideline for mandatory X-ray monitoring after endodontic treatment and dental implantation surgery has already been adopted in order to indicate the relationship between the root and the root filling, as well as the proximity of the implant bed and/or the implant itself to the canal of the inferior alveolar nerve. Intraoral dental radiography is considered to be sufficient to detect iatrogenicity, although post-traumatic neuropathy is primarily a clinical diagnosis.
Renton T, Yilmaz Z. Managing iatrogenic trigeminal nerve injury: a case series and review of the literature. Int J Oral Maxillofac Surg 2012 May;41(5):629-637.
Recovery and treatment
In the first case, self-recovery takes approximately 1 month; the help of doctors is not needed, since there is no anatomical damage. Symptoms of the second appear after a while - usually 6-8 weeks, so recovery can be painful and incomplete: it will take more than 2 months. In the third stage of damage to the mandibular nerve, treatment gives results only at the beginning and is performed surgically, since we are talking about degeneration with a violation of integrity. Loss of sensitivity, which is observed in a patient for more than 3 months, indicates a high probability of losing it forever. Damage to the mandibular nerve, the consequences of which is the lack of sensitivity of the nerve for a year, leads to irreversible changes. Only the professionalism and responsibility of the doctor, which is guaranteed by the specialists of our Implantmaster clinic, can protect the patient from such unpleasant injuries.