- Causes of salivary gland cancer and risk groups
- Symptoms of the disease
- Diagnostic methods
- Classification: types of salivary gland cancer
- Stages of the disease
- Treatment
- Complications and relapses
- Life prognosis at different stages of cancer and prevention
The salivary glands produce saliva, a liquid found in the oral cavity that performs some important functions: wetting the mucous membrane, food, facilitating articulation, swallowing, protecting against pathogenic bacteria, etc. There are two groups of salivary glands:
- Large: sublingual, parotid, submandibular.
- Small ones have a microscopic structure, scattered throughout the oral cavity - there are several hundred of them in total.
Cancer can develop in all of these glands. Most often (in 7 out of 10 cases), benign and malignant tumors arise in the parotid salivary glands. Approximately 1–2 tumors out of ten occur in the submandibular salivary glands; in 50% of cases they are malignant. In rare cases, cancer develops in the sublingual or minor salivary glands.
Causes of salivary gland cancer and risk groups
A normal salivary gland cell becomes cancerous when a certain set of mutations occurs in it. The development of malignant tumors is caused by mutations in oncogenes (genes that activate cell reproduction) or tumor suppressor genes (suppress cell reproduction, “repair” damaged DNA, trigger programmed cell death - apoptosis). In each specific case, it is very difficult to judge the reasons for the mutations that occurred in cells. It is impossible to say why exactly they happened.
There are some risk factors that increase the likelihood of developing a malignant tumor:
- The older a person is, the more changes in his genes accumulate, the higher the likelihood of developing various types of cancer.
- Salivary gland cancer is more common in men than in women.
- Irradiation of the head. For example, this may be a previous course of radiation therapy, exposure to ionizing radiation in the workplace.
- There is evidence that the risk of salivary gland cancer is increased in people who have certain occupational hazards: contact with asbestos, nickel alloy dust, work in enterprises that produce rubber and woodworking.
The role of heredity is currently considered insignificant. Most patients do not have a family history (close relatives who have been diagnosed with the same type of cancer). The role of alcohol and tobacco has not been proven. These unhealthy habits are known to increase the risk of head and neck cancer in general, but no association has been found with salivary gland cancers.
Is a mobile phone dangerous? In one study, researchers found that heavy cell phone users were more likely to have parotid tumors (usually benign). But other studies have not found such a relationship.
CT signs of salivary stone disease
Swelling, enlargement of the parotid and submandibular areas that do not go away after taking pharmaceutical drugs are an indication for radiation diagnostics. Symptoms are caused not only by sialadenitis. Salivary obstruction (sialolithiasis) is determined after CT sialography by the following signs:
- Increase in the size of the damaged organ;
- Maintaining uniformity of structure;
- Dilation of the duct.
Additionally, the radiology doctor will indicate the tissue density. The sign is a differential marker for determining the effectiveness of therapy in order to track dynamics on repeated tomograms.
The information content is increased by using digital subtraction sialography - contrasting (injection of an iodine-containing drug) of the ducts, followed by radiography in two projections. Examination is not common in Russian medicine. It is used by scientific institutions, but European specialists are actively using the analysis capabilities for clinical purposes.
Thin-section SCT of the head and salivary glands with three-dimensional modeling (3D) creates a spatial structure with which doctors determine the intraductal location of the stone.
The use of examination helps to detect adenocarcinoma of the salivary gland - a malignant tumor prone to rapid progression and invasion of nearby tissues. Oncology is more often discovered by chance, as it does not have specific external signs.
Symptoms of the disease
Benign and malignant tumors of the salivary glands present with similar symptoms. One of the main differences is that cancer grows much faster and more often leads to a number of symptoms associated with growth into surrounding tissues and compression of nerves.
You need to visit a doctor if you are bothered by the following symptoms:
- A lump or swelling has appeared in the mouth, cheek, jaw, or neck.
- You have noticed that your face has become asymmetrical.
- I am worried about pain in the mouth, neck, ear, cheek, jaw. It doesn't last long.
- Numbness of part of the face.
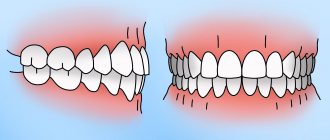
- Weakness in the facial muscles, because of this, half of the face may be “lowered,” which becomes especially noticeable when baring teeth or frowning.
- I can't open my mouth wide.
- Difficulty swallowing.
When to see a doctor
At the first symptoms of salivary gland cancer, you should consult an oncologist. The earlier the disease is diagnosed, the more effective the prescribed course of treatment will be. If you are looking for a highly qualified doctor in Moscow, then contact the oncological JSC "Medicine" (clinic of Academician Roitberg), which is located at 2nd Tverskoy-Yamskaya lane 10 (Mayakovskaya metro station).
The first symptoms of salivary gland cancer:
- bumps or swelling in the neck, cheeks, jaw, ears;
- muscle weakness;
- “drooping” of the face and other signs, which were discussed in more detail above.
Diagnostic methods
During the initial appointment, the oncologist talks with the patient, questions him, trying to find out risk factors, and conducts an examination. The doctor feels the tumor on the face and cervical lymph nodes, evaluates the sensitivity of the face and the work of facial muscles. After this, the patient can be referred for additional consultation to an ENT doctor.
Computed tomography and magnetic resonance imaging help assess the size, shape and location of the tumor, and detect lesions in the lymph nodes and other organs. The current gold standard for searching for distant metastases is PET scanning. If the tumor is located near the jaw, an x-ray is taken. A chest x-ray helps detect metastases in the lungs and evaluate the condition of the lungs and heart before surgical treatment.
The most accurate method for diagnosing salivary gland cancer is a biopsy. During this procedure, the doctor receives a fragment of pathologically altered tissue and sends it to the laboratory for cytological and histological examination.
The most common procedure is fine-needle aspiration biopsy. Tumor tissue is obtained using a hollow needle similar to the one used for injections. If the required amount of tissue cannot be obtained, the doctor performs an incisional biopsy: makes an incision and removes part of the tumor.
If tumor cells are found in the sample, the diagnosis of cancer is virtually certain.
Tomography of the salivary glands CT and MRI for sialadenitis, salivary stone disease, cancer
To identify diseases of the salivary glands (sialoadenitis, Sjogren's syndrome, blockage of the ducts with stones), radiation methods are used - CT, MRI, ultrasound.
The specificity of computed tomography for nosological forms is about 100%, reliability is 98%. The indicators are high for reliable verification of the pathology of the parotid and submandibular glands. Radiation exposure limits the widespread use of the method. A one-time examination does not cause harm, but it is not recommended to scan frequently (except for verification of tumors). MR imaging is good at differentiating changes in glandular structures. Equipment and maintenance costs are high. The devices are installed in large megalopolises, which reduces the accessibility of the study to the population.
CT sialography is used for acute and chronic cases of salivary stone disease, sialoadenitis, mumps, and Sjögren's mumps. The method allows you to correctly make a diagnosis, identify the localization, prevalence, and stage of the pathological process.
Sjögren's syndrome is manifested by damage to body tissues by components of the body's own immune system (antibodies). Initially, the inflammatory process is clinically similar to mumps. The appearance of pseudolymphomas and lymphadenopathy, which are markers for prescribing hormonal treatment, allows one to suspect an advanced process. Therapy reduces the rate of progression.
Classification: types of salivary gland cancer
The salivary glands are made up of different types of cells, any of which can give rise to a malignant tumor. Therefore, there are different types of cancer:
- Mucoepidermoid carcinoma of the salivary gland is the most common type. Most often it is found in the parotid salivary glands, less often in the submandibular and small ones. These tumors are rarely aggressive.
- Adenoid cystic carcinoma is characterized by very slow growth and rare metastasis. However, this malignant tumor can be very difficult to get rid of: it can recur a long time after treatment.
- Adenocarcinoma is a malignant tumor that develops from glandular cells. Different types of adenocarcinomas can occur in the salivary glands: acinic cell carcinoma, low-grade polymorphic adenocarcinoma, basal cell adenocarcinoma, clear cell carcinoma, cystadenocarcinoma, etc.
- Rare types of malignant cancers of the salivary glands include: squamous cell carcinoma, epithelial-myoepithelial carcinoma, anaplastic small cell carcinoma, undifferentiated carcinomas.
Causes of the disease
A number of factors can provoke the manifestation of the disease, which include various influences from the outside world. Any patient can encounter this, even with good oral hygiene.
Main causes of the disease:
- pathogenic microorganisms that have entered the patient’s oral cavity;
- some viral diseases;
- toxic substances contained in food.
Another reason for the formation of salivary gland adenoma is considered to be an addiction to smoking tobacco. Smoke that enters the body contains many carcinogens that damage the glandular epithelium of the salivary glands. As a result, protective mechanisms are activated, which provokes increased cell division, resulting in the formation of an adenoma.
Stages of the disease
Salivary gland cancer, like other malignant tumors, is classified into stages according to the generally accepted TNM system. The letter T in the abbreviation denotes the characteristics of the primary tumor: the size and degree of its growth into surrounding tissues, N - spread to the lymph nodes, M - the presence of distant metastases. Depending on these indicators, the following stages are distinguished during salivary gland cancer:
- Stage 0 is “cancer in situ” (carcinoma in situ). The tumor is located within the layer of cells that form the salivary gland and does not grow into neighboring tissues.
- Stage I is a tumor that is located within the salivary gland and measures no more than 2 cm.
- Stage II - the tumor reaches a size of more than 2 cm, but not more than 4 cm.
- Stage III - a tumor that reaches a size of more than 4 cm and/or spreads into surrounding tissues, or a tumor of any size that has grown into surrounding tissues, has spread to one cervical lymph node on the same side, and the focus in the lymph node is no more than 3 cm and does not extend beyond its borders.
- Stage IV includes substages IVA, IVB or IVC. The first two are characterized by varying degrees of spread of the malignant tumor to the anatomical structures of the head, neck, and lymph nodes. If stage IVC is diagnosed, it means that there are distant metastases.
In addition to stages, there are three degrees of malignancy of salivary gland cancer:
- Grade I - low degree of malignancy. Such tumors are called highly differentiated. Tumor tissue is as similar as possible to normal salivary gland tissue. It grows slowly, and the prognosis for such patients is most favorable.
- Grade II are moderately differentiated tumors. Tumor tissue differs more significantly from normal tissue. This cancer is more aggressive and has a poorer prognosis.
- III degree - poorly differentiated tumors. Cancer cells almost completely lose the features of normal ones. Such tumors behave the most aggressively.
Determining the degree of malignancy helps the doctor predict how the cancer will behave and plan treatment correctly.
Complications
Despite the fact that treatment of salivary gland adenoma does not pose a serious problem, it is important to remember that untimely removal of the tumor can lead to a number of complications. The most serious of them is the transformation of a benign neoplasm into a malignant one. Unlike malignant tumors, salivary gland adenoma can exist asymptomatically, only in some cases causing facial asymmetry. Therefore, if you detect the slightest swelling, you must immediately consult a doctor. Timely removal of the tumor will prevent many very unpleasant problems.
The most common postoperative complications:
- the risk of developing Frey's syndrome (occurs when autonomic nerve fibers are damaged, accompanied by redness and sweating of the operated area of the face);
- a feeling of dry mouth when the gland is completely removed.
Observation and regular consultations with a doctor can reduce all postoperative complications to a minimum.
Treatment
The patient is treated by a team of doctors, which may include: a clinical oncologist, an ENT doctor, an oncologist-surgeon, an oral and maxillofacial surgeon, a chemotherapist, a radiotherapist, etc. The treatment program is determined by the stage of cancer, the histological type of the tumor, its location (which gland is affected) , age, general condition and concomitant diseases of the patient.
Surgery
If the tumor has not grown much into the surrounding tissue, then it is resectable, that is, it can be removed surgically. The surgeon’s task is to excise the tumor while capturing the surrounding tissue so that there are no cancer cells left on the cut line, that is, to ensure a negative resection margin. If tumor cells have spread to the lymph nodes, or a biopsy reveals aggressive cancer, the lymph nodes are also removed.
For parotid salivary gland cancer, surgery presents certain difficulties, because the facial nerve passes through the gland, which controls the work of facial muscles. If the tumor affects only the superficial lobe of the gland, you can remove it separately - perform a superficial parotidectomy. There is no risk of damaging the facial nerve. In some cases, it is necessary to remove the entire gland, and if the tumor has grown into the facial nerve, then it too.
For cancer of the sublingual and submandibular gland, the surgeon removes the gland itself and some of the tissue located around it, including, possibly, bone tissue. In some cases, it is necessary to excise the nerves that control sensitivity, movements in the lower part of the face, in the tongue, and the sense of taste.
For cancer of small glands, the affected gland and part of the surrounding tissue are removed. The extent of the operation depends on the size and location of the tumor.
Radiation therapy
Indications for the use of radiation therapy for malignant tumors of the salivary glands:
- To combat malignant tumors that cannot be removed surgically due to their location or size. Sometimes radiation is supplemented with courses of chemotherapy.
- After surgical treatment. This type of radiation therapy is called adjuvant and is sometimes combined with chemotherapy. Radiation after surgery helps destroy remaining cancer cells and prevent recurrence.
- For advanced cancer. In this case, radiation therapy is aimed at combating pain, difficulty swallowing, bleeding and other symptoms.
Radiation is typically given five days a week for 6–7 weeks. If radiation therapy is used for palliative purposes, the course will be shorter.
Chemotherapy
Chemotherapy is used quite rarely for malignant neoplasms of the salivary glands. Anticancer drugs can reduce the size of the tumor, but are not able to completely destroy it. They are most often prescribed for advanced cancer as palliative treatment or in addition to radiation therapy.
Depending on the type and other characteristics of the cancer, the doctor may prescribe combinations of different chemotherapy drugs: carboplatin, cisplatin, 4-fluorouracil, doxorubicin, paclitaxel, cyclophosphamide, vinorelbine, docetaxel, methotrexate. Chemotherapy for cancer is always given in cycles. The patient is administered the drug, then takes a “break” for several days. The course of treatment may consist of several cycles.
Rehabilitation
After treatment, some problems associated with nerve damage may persist: dysfunction of the facial muscles, speech disorders, swallowing, and cosmetic defects. Some side effects of chemotherapy and radiation therapy go away after treatment is completed, while others persist for a long time. In such cases, rehabilitation courses are indicated. The doctor draws up a rehabilitation treatment program individually, depending on the severity and nature of the disorders.
Where research becomes real-time treatment
The first approach to treatment is the most important. Treatment is the main goal, and is considered as important as quality of life and the functionality of the organs being treated, such as voice, tongue, swallowing, taste and breathing. IEO provides patients with a multidisciplinary team dedicated to diagnosis, treatment and rehabilitation
Innovative and Minimally Invasive Treatments: Over the years, the department has developed various innovative techniques and minimally invasive approaches to improve surgical outcomes in terms of tumor removal and preservation of organ function to expand treatment options for patients with less surgical exposure. Some of these treatments are only available here at IEO.
Surgery : Our head and neck surgeons perform the largest number of operations on malignant tumors each year than any other center in Italy (according to AGENAS). Moreover, for more than 20 years we have been implementing Professor Veronesi’s legacy: that is, we have been using “minimally effective therapy” also for lesions of the head and neck. We were the first in Italy to offer conservative thyroid surgery, thanks to more than 15 years of experience in the field of hemithyroidectomy, even for malignant tumors. We were one of the first to perform endoscopic conservative operations on the larynx, the number of which now exceeds 250 procedures per year, and became pioneers in functional tongue surgery, providing an almost normal quality of life after surgery. Finally, we have been performing very delicate operations on the salivary glands for more than 20 years. It is the only recognized department for head and neck surgery in Italy.
USDAS (Ultrasound Dye Assisted Surgery): The department has developed an original technique using vital dyes under ultrasound guidance to identify recurrent nodules in the thyroid gland, salivary gland and lymph nodes. This method is more effective and reduces the risk of complications.[1]
THE IMPORTANCE OF A MULTIDISCIPLINARY TEAM
The mission of our multidisciplinary team is to diagnose, treat and rehabilitate patients with head and neck tumors and to study these diseases. Our team includes more than thirty oncology professionals with experience in various disciplines such as otorhinolaryngology (ENT), oral and maxillofacial surgery, emergency surgery, plastic and reconstructive surgery, radiotherapy, medical oncology, radiology, pathology, nuclear medicine, nutrition, physiotherapy , endocrinology, dentistry, phoniatrics, speech therapy, psychology and biology.
Integrating different knowledge and skills can address a range of clinical issues, from diagnosis and treatment planning to functional recovery (speech, breathing, swallowing) to achieve the best results in cancer treatment and quality of life. The team works cohesively and meets weekly to discuss cases of patients who have trusted our organization. They develop comprehensive, personalized care plans that address all aspects of treatment and rehabilitation, considering a variety of treatment options and taking into account the needs of individual patients, in accordance with domestic, national and international guidelines.
The team, in close collaboration with the Science and Health Board, monitors treatment outcomes and performance in real time to highlight key issues and identify areas for improvement and development. Multidisciplinary meetings are an opportunity for professional development based on intragroup exchanges, literature findings, and critical reviews and updates of guidelines, as well as diagnostic and therapeutic approaches. Information obtained from critical review of clinical activity, technological innovation, study of the evolution of treatable tumors, and continuous updating is used to identify open questions and propose research studies. Thanks to this approach, clinical research studies and collective research projects have been introduced in collaboration with national and international organizations.
Tumor of the parotid gland
The treatment of choice for a parotid gland tumor is salivary gland surgery (with a few rare exceptions such as lymphoma). Surgery allows, if necessary, to remove the parotid tumor and some surrounding tissue and lateral cervical lymph nodes (which can be the site of metastases). Interventions are sensitive, especially due to the presence of nerve structures in the salivary glands (facial nerve and its branches). Surgical techniques are the most advanced and use magnification (using a microscope and/or magnifying glasses) and reconstruction of the facial nerve if it is damaged during parotid tumor removal. Based on the final histological examination of the parotid tumor, postoperative radiation therapy is prescribed in some cases.
When the facial nerve must be sacrificed (due to parotid tumor infiltration), immediate reconstruction can be performed by transferring one or more donor nerve segments (large auricle, tibia, latissimus dorsi). The donor nerve can be donated because it does not involve significant functional deficit. This method can be performed in patients undergoing postoperative radiation therapy and allows restoration of facial mobility within 4-12 months. If for any reason immediate reconstruction cannot be performed, the patient may choose to undergo various types of delayed reconstruction.
Access to the most innovative treatments: Immunotherapy is one of the most promising non-surgical treatments and works to enhance the patient's immune response to the tumor. Adrotherapy (radiation therapy with protons or carbon ions) is a popular treatment for many salivary gland tumors or tumors located in sensitive anatomical locations or difficult to remove surgically.
Distant metastases of head and neck cancer
Distant metastasis is defined as tumor spreading to other organs. Lung, liver, and bone are the most common sites for hematogenous metastases of head and neck squamous cell carcinoma. The incidence of distant metastasis in head and neck squamous cell carcinoma is low for the general head and neck squamous cell carcinoma population, typically below 5% in the sample. Patients with head and neck squamous cell carcinoma with distant metastases are generally candidates for palliative treatment scenarios only, as no systemic therapy currently has curative potential in patients with head and neck squamous cell carcinoma with distant metastases. Consequently, extensive locoregional therapy is usually considered futile in these patients. We are particularly focused on collaborating with CNAO, National Center for Oncological Hadrontherapy) for a phase II clinical trial on radiation therapy using protons (hadron therapy) for locally advanced tumors of the cervicofacial region.
[1] Giugliano G, DE Fiori E, Proh M, Chulam Celestino T, Grosso E, Cattaneo A, Gibelli B, Massaro M, Ansarin M. Ultrasound dye-assisted surgery (USDAS): a promising diagnostic and therapeutic tool for the treatment of cancer recurrences in the neck. Acta Otorhinolaryngol Ital. 2011 Aug;31(4):222-7
Complications and relapses
Even if the treatment is successful and the examination results show no signs of the presence of cancer cells in the patient’s body, a relapse may occur in the future. Therefore, you need to regularly see an oncologist, come for examinations, undergo various studies and take tests.
Typically, the doctor prescribes examinations once every few months for several years, then less frequently.
- If cancer recurs, treatment options may vary:
- If the tumor can be removed, surgery is performed followed by a course of radiation therapy.
- If the tumor cannot be removed surgically, the doctor prescribes radiation therapy in combination with chemotherapy.
- If there are distant metastases, chemotherapy becomes the main treatment method. Radiation therapy and surgery can be used to control some symptoms.
With advanced cancer with metastases, achieving remission becomes extremely unlikely. In this case, treatment will be aimed at slowing the progression of cancer, combating symptoms, and prolonging the patient’s life.
Euroonco doctors undertake cancer treatment at any stage. For us there are no hopeless patients. You can always help, and we know how to do it correctly, we have all the necessary technologies, the latest generation drugs.
How to make an appointment with a specialist in oncology
The oncology department employs highly qualified specialists. You can make an appointment with an oncologist using a special form on the website. It is also possible to get an appointment with a specialist by calling: +.
You can make an appointment for a consultation or carry out a full diagnosis if you suspect cancer. Modern equipment and the professionalism of our doctors allow us to accurately diagnose and begin the most effective, rapid treatment that will give the best results.
The clinic is located in the very center of Moscow at the address: 2nd Tverskoy-Yamskaya lane 10 (Mayakovskaya metro station).
Symptoms
Symptoms depend on the nature of the tumor; in most cases, it becomes noticeable only in the later stages. One of the first signs is constant drying of the oral mucosa and excessive salivation.
As the tumor grows and becomes more noticeable, it can be felt through the outside of the cheek or with the tongue inside the mouth. Malignant formation can be round or oval, with a dense consistency. When pressing, a slight pain is felt.
If the cancer reaches the nerve endings, the mobility of the face on the side of the tumor is limited, and a feeling of numbness appears. In later stages, paralysis of the facial muscles develops.
Other symptoms:
- headache;
- pain and heaviness in the ear (signs resemble purulent otitis media);
- decreased hearing quality;
- facial muscle spasms.