Candidiasis provokes eczema, changes in stool, and headaches. Candidiasis greatly suppresses the immune system and this makes it very dangerous.
The disease caused by fungi of the genus Candida is one of the most common lesions of the lower genital tract in girls. According to the luminaries of domestic pediatric gynecology, Candida fungi are found in more than half of the cases of chronic recurrent vulvovaginitis in preschool girls and in 24-25% of adolescents with inflammatory diseases of the genital organs (M.N. Kuznetsova, 1998; Yu.A. Gurkin, 2000).
Fungi of the genus Candida are permanent representatives of the human microflora. But under certain conditions (decreased immunity, dysbacteriosis, impaired lipid and salt metabolism), yeast-like fungi acquire vegetative (growing) forms.
Fungi of the genus Candida can infect mucous membranes, skin, legs, and internal organs.
Candidiasis provokes eczema, changes in stool, and headaches. Candidiasis greatly suppresses the immune system and this makes it very dangerous.
Diagnosis and treatment of thrush at the Yauza Clinical Hospital
Diagnostics
Diagnosis of vaginal candidiasis begins with interviewing the patient.
Some gynecological (bacterial vaginosis, inflammatory processes in the female reproductive system) and concomitant diseases (diabetes mellitus, candidiasis and intestinal dysbiosis, etc.) are important. It is not uncommon for thrush to develop after long-term use of antibiotics, hormones, or immunosuppressants. Upon examination, a characteristic clinical picture is revealed - a white coating on the inflamed mucous membrane of the genital organs, copious, curdled discharge. Examination of a vaginal smear reveals fungal flora. If necessary, a culture is carried out to determine the type of fungus and its sensitivity to antifungal drugs (cultural analysis). Among additional studies, examination for sexually transmitted infections, diabetes mellitus and diagnosis of intestinal microflora may be recommended. Make an appointment with a gynecologist
Treatment
How to cure thrush?
General and local antimycotic therapy Gynecologists at the Yauza Clinical Hospital provide effective treatment for thrush in women. Today there are many medications to combat candidiasis: oral medications, creams, vaginal tablets, suppositories for thrush. Among the most popular drugs for vaginal candidiasis are flucostat, fluconazole (oral tablets), clotrimazole (vaginal tablets or cream), pimafucin (suppositories) and many other drugs. Your doctor should choose the optimal treatment regimen for you.
Reducing the role of predisposing factors To avoid relapses, it is necessary to identify and eliminate factors contributing to the disease. If possible, stop taking glucocorticosteroids and cytostatics. For diabetes mellitus, adjust blood glucose levels with medication. Restore normal microflora in the intestines. In addition, you need to take antibiotics with caution. Exacerbation/recurrence of thrush after or during a course of antibiotic therapy is common. Therefore, taking antibiotics must be combined with taking antifungals and probiotics. It is necessary to maintain personal hygiene, maintain immunity, and avoid stressful situations.
Sexual life with thrush Many people are interested in whether it is possible to be sexually active with thrush and its treatment? You can protect yourself with a condom. To achieve good results, it is often recommended to undergo treatment of vaginal candidiasis together with your sexual partner.
Sexual infection in children
In recent decades, the importance of the problem of protecting the reproductive health of children and adolescents has increased. Social processes such as environmental deterioration, urbanization, uncontrolled use of drugs, in particular antibiotics, have a negative impact on the development of the child’s reproductive system, its resistance to infectious environmental factors, and the state of local immunity of the genital tract. All this leads to the spread of inflammatory diseases of the genitals in children.
The issues of treatment and rehabilitation of patients with inflammatory diseases of the external genitalia are relevant, since relapses and chronicity of inflammatory processes worsen the prognosis for generative function, which, in turn, is a social and economic problem.
The division of urogenital inflammatory diseases into specific and nonspecific has now become very arbitrary. Research in recent years has shown that, along with gonococci, trichomonas, chlamydia and other pathogens, opportunistic aerobic microorganisms are found in patients, and the etiological factor is a microbial association with its unique biological properties. At modern stages, urogenital inflammatory diseases in many cases lose their initially inherent specificity of clinical course. Cases of detection of mixed infections have become more frequent, and in microbial associations the pathogenicity of each microbe increases [2, 6, 12, 14]. Diagnosis becomes difficult, complications and relapses of the disease may develop, and the clinical course of the infection changes.
It is traditional to distinguish sexually transmitted diseases (syphilis, gonorrhea, trichomoniasis, chancroid, donovanosis, lymphogranulomatosis venereum) and sexually transmitted infections (diseases) (hepatitis, HIV, chlamydia, human papillomavirus infection, etc.). However, this division is gradually losing its significance, and at the moment all these diseases are united under the term “sexually transmitted infections” (STIs).
The incidence of STIs has been progressing in recent years both among children and adolescents. In 2002, the proportion of patients in the age group under 18 years old was: patients with gonorrhea - 6.8%, trichomoniasis - 2.3%, chlamydia - 3.4% of the number of cases [6]. These indicators may be somewhat underestimated due to the presence of commercial medical institutions that do not carry out statistical records of morbidity, as well as the prevalence of self-medication, especially in the adolescent population. There is a trend toward “rejuvenation” of STIs.
The main routes of infection of children with STIs are [6, 12]:
- transplacental (HIV, viral hepatitis B and C, syphilis, papillomavirus infection);
- perinatal (HIV, viral hepatitis B and C, syphilis, gonococcal, trichomonas, chlamydial and human papillomavirus infections);
- transmission of infection during breastfeeding (HIV; for viral hepatitis B and C, syphilis, the risk of infection is not clear enough);
- direct contact:
– autoinoculation (herpetic and human papillomavirus infections);- through household items;
– sexual contact (all STIs);
– transfusion (HIV, hepatitis).
Most foreign researchers place infection with STI pathogens during close household contacts or during autoinoculation in last place in terms of prevalence and regard such cases as casuistic (with the exception of herpes simplex viruses and human papillomavirus) [6, 11].
According to domestic researchers, the possibility of infection in these cases cannot be excluded, and according to the publications of some authors, infection of children through household contact is quite widespread (0.7% for gonorrhea, 26.1% for trichomoniasis, 66.1% for chlamydia ) [4].
Previously, sexual transmission of STIs was more common among adolescents (14–18 years old), but now the number of cases of sexual transmission of infection has increased in the group of children under 12 years of age. According to various researchers, from 7.5 to 70% of the total number of diseases of the lower genitourinary tract in children are classified as STIs, while the prevalence of STIs in children with a history of sexual intercourse varies within the following limits: gonorrhea - from 0 to 26.3 %, chlamydia - from 3.9 to 17%, trichomoniasis - from 0 to 19.2%, syphilis - from 0 to 5.6%. The difference in rates is due to the fact that the incidence of STIs varies widely both in different regions and in populations within the same region.
According to social surveys conducted among children and adolescents, about 15% of girls and 22% of boys noted the presence of sexual intercourse in their lives, while 50% of them indicated that the first sexual intercourse was committed before the age of 15, and in 5% of girls and 2% of boys it occurred before the age of 12 years.
Given the psychological and physiological immaturity of the child’s body, any form of sexual contact with a child is sexual abuse. In our country, the problem of sexual violence against children has always received little attention. In a survey of Moscow and St. Petersburg schoolchildren conducted in 1993, 24% of girls and 11% of boys indicated a history of sexual coercion. Data from a sociological survey conducted in 21 countries of the world indicate that from 7 to 36% of women and from 3 to 29% of men become victims of sexual violence under the age of 18 [5, 11].
Cases of sexual violence in the family present a separate problem. Children aged 5–10 years, both boys and girls, are most often targets of violence. According to various authors, about 50% of all cases of sexual violence occur in the family. Domestic violence, as a rule, is long-term (occurs over many years), leads to chronic trauma for the child and greatly increases the risk of infection with STIs.
Counseling of a child suspected of having an STI should be carried out by specialists who have the skills to examine the child and obtain the clinical material necessary for the study. Of great importance is the study of medical and social history, carried out with the consent of the child’s parents or persons representing his interests.
However, the causes of inflammation of the urogenital area are diverse; they can be of an infectious or non-infectious nature, occurring primarily or secondary. In this regard, the examination of children should be comprehensive: clarification of medical history, general status, identification of concomitant diseases that may be the cause of inflammation of the urogenital tract. If an STI is suspected in a child, laboratory diagnostics must necessarily include the isolation of a pure culture, which allows for a correct diagnosis to be established [1, 4, 6, 7, 11].
Vulvitis and vulvovaginitis
Inflammation of the external genitalia can be primary or secondary. Primary vulvitis occurs due to errors in child care, injuries, diabetes mellitus, helminthiasis, urinary incontinence, and furunculosis.
In girls, the frequency of primary vulvitis is associated with imperfect endocrine and immunological processes, as well as anatomical and physiological characteristics of the genital organs (delicate skin, a large number of vestibular glands).
Secondary vulvitis occurs as a result of inflammatory processes in the internal genital organs (colpitis). In childhood, the development of vaginitis is promoted by ovarian hypofunction [10, 13].
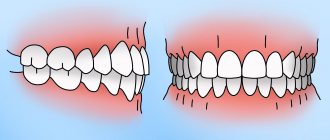
The clinical picture of vulvitis depends on the severity of the process. When the process is active, the tissues of the vulva become swollen, and there is hyperemia of the labia majora and minora. Often all these symptoms are diffuse in nature, not only the vulva is affected, but also the inguinal folds, and the inguinal lymph nodes become enlarged. Patients complain of itching in the vulva and purulent discharge from the genital tract. Watery discharge of a yellowish-green color occurs when affected by E. coli. With staphylococcal infection, the discharge is thick, yellow-white.
Therapy for nonspecific vulvitis should be comprehensive. The external genitalia are treated with disinfectant solutions 5-6 times a day (2% oil solution of chlorophyllipt; 0.5% dioxidine solution; chamomile, string, calendula). Desensitizing (fenistil, elidel) and sedative therapy (valerian) is mandatory [5, 10 13].
Vulvovaginitis most often develops in girls aged 3–8 years. This is due to the fact that their epithelium does not contain glycogen, the mucosa is loose, tender, vulnerable, and the vaginal secretion has an alkaline reaction. Vulvovaginitis accounts for 65% of all diseases of the genital organs in childhood. Its occurrence is facilitated by dysfunction of the genital organs, common infectious diseases, endocrine disorders, helminthiasis, and ingestion of foreign bodies [10, 13].
Clinical manifestations depend on the severity of the process, but they can be very similar to those of vulvitis.
Treatment is aimed at eliminating the cause of the disease. Sanitation of foci of infection, treatment of helminthiasis, extragenital diseases, and endocrine disorders are necessary. Vulvovaginitis in girls, caused by a foreign body entering the vagina, proceeds violently and is accompanied by copious purulent discharge from the genital tract.
Local treatment of vulvovaginitis is similar to the treatment of vulvitis, but douching of the vagina with solutions of furatsilin, octenisept, dioxidine is added to the therapy, followed by the introduction of antibiotics into the vagina in the form of sticks based on cocoa butter.
It is also recommended to take vitamin preparations (Vitrum, Unicap), Duphalac (10-20 ml once a day) or bifidumbacterin (10 doses per day) [5, 10-13].
Gonococcal infection
The causative agent of gonococcal infection is the gram-negative diplococcus N. gonorrhoeae. Gonorrhea is a sexually transmitted disease that can affect both boys and girls, but among girls, gonorrheal infection is 10–15 times more common. The factor determining the development of the gonococcal process in children is considered to be favorable morphofunctional physiological conditions for the life of the infection in their genitourinary organs. Children aged 3–12 years are most often affected [4, 6, 14].
The frequency of infection with gonococci in girls depends on age, chronological fluctuations in immunity and hormonal state. Gonorrhea is rare in newborns due to passive maternal immunity and the presence of maternal estrogenic hormones.
At the age of 2–3 years, passive protective maternal antibodies are depleted, and the level of estrogen saturation decreases. During this period, the condition of the mucous membrane of the external genitalia and vagina changes. In the cells of the cylindrical epithelium, the glycogen content decreases, the activity of diastase decreases, the vaginal discharge acquires an alkaline or neutral reaction, the Dederlein rods disappear, which break down glycogen to lactate and thereby cause an acidic reaction, and the pathological microbial flora is activated.
In subsequent years of life, due to the activation of the function of the endocrine glands, the level of glycogen in the epithelial cells increases, the pH becomes acidic, and the population of Dederlein rods is restored, displacing pathogenic flora.
Gonorrhea in childhood has a number of features, the main ones being the multifocal nature of the lesion and the possibility of developing a disseminated process. With multifocal lesions in girls, in 100% of cases the vagina is involved in the process, in 60% - the urethra, in 0.5% - the rectum. Damage to the mucous membranes occurs immediately after contact with gonococci, and subjective complaints and objective symptoms of the disease appear after the incubation period (from 1–3 days to 2–3 weeks). The clinical picture of gonorrhea in girls is sometimes characterized by a torpid, recurrent course, and in some cases it is asymptomatic. However, the most typical is the acute onset of the disease, which is characterized by copious purulent discharge, diffuse hyperemia of the external genitalia, perineum, skin of the inner thighs, and perianal folds. Girls complain of pain when urinating, tenesmus. The discharge is purulent, thick, greenish in color, sticks to the mucous membrane, and when it dries, leaves crusts on the skin.
Ascending gonorrhea is rare, but the possibility of its development must be remembered, especially in the presence of cervicitis. The disease is facilitated by the absence of a barrier in girls in the form of a closed internal pharynx; the folds of the cervical canal do not end at the internal pharynx, as in adult women, but continue into the uterine cavity, and the endometrium is affected. Primary gonorrheal endocervicitis in the “neutral period” (the period of sexual calm from 2.5–3 years before the onset of puberty) in the absence or poor development of glandular tissue is rare. More often, secondary development of endocervicitis occurs during the chronic course of gonorrhea in girls aged 8–10 years and older. Its course is usually torpid and sluggish. Often the cervical mucosa is affected in girls of puberty, in whom, however, bartholinitis practically does not occur.
Gonorrhea in boys occurs in almost the same way as in adult men, but less acutely and with fewer complications, since the prostate gland and seminal vesicles are underdeveloped before puberty, and the glandular apparatus of the urethra is underdeveloped. Patients feel pain and pain when urinating, purulent discharge from the urethra, and dysuria. The lips of the external opening of the urethra are swollen and hyperemic. Palpation of the urethra may be painful. Hyperemia and swelling can spread to the skin of the glans penis and foreskin. Purulent yellowish-greenish discharge flows freely from the urethra. Due to the secretions, maceration of the inner layer of the foreskin can develop. Erosion may form on the head of the penis. Balanitis and balanoposthitis are possible. On the skin of the penis and adjacent areas, erosions become covered with crusts. In addition, hyperemia of the skin of the penis and areas close to it, as well as the perianal area, may be observed.
Traditionally, the diagnosis of gonorrhea is established on the basis of obtaining a pure culture of gonococcus in clinical material from the patient and determining saccharolytic properties. Fermentation of carbohydrates makes it possible to differentiate gonococcus from other gram-negative microorganisms, most often meningococcus and catarrhal micrococcus, which are often present in the urogenital tract of children.
Non-culture tests for gonorrhea, including Gram stain, DNA probes or ELISA, should not be used without culture [4, 7]. Specimens from the vagina, urethra, pharynx, or rectum should be tested on selective media to identify gonococci. All suspected materials from an outbreak of N. gonorrhoeae must be accurately identified, at least by tests based on various principles (biochemical and serological properties of the pathogen). With an appropriate clinical picture, the detection of gonococci in Gram-stained smears or the presence of a large number of red blood cells in smears, even in the absence of flora, allows one to suspect gonorrhea.
A child with gonorrhea is hospitalized. Treatment of gonorrhea in childhood should be comprehensive (antibiotic therapy, restorative therapy aimed at restoring immune status).
In children, benzylpenicillin remains the drug of choice (course dose 4.2–6.8 million units). The drug is administered in single doses of 50–200 thousand units, depending on age, with an interval of 4 hours around the clock. The course lasts 5–7 days. Ceftriaxone is also used at a dose of 125 mg intramuscularly once for a body weight of less than 45 kg [1, 6]. During the entire period of antibiotic therapy, bed rest is prescribed with a daily change of linen.
The follow-up period is 5 months. During this time, children are not allowed into kindergartens; attendance at school is allowed immediately after completion of treatment and receipt of negative results of repeated bacteriological tests: three provocations and three cultures with an interval of 10 days.
In case of a torpid and long-term course of the disease, the observation period is extended to 1.5–2 months with repeated bacteriological and cultural studies.
It should be remembered that gonorrhea causes an exacerbation of existing genitourinary tract infections. In this case, the clinical picture of the disease can change significantly. For example, trichomonas infection reduces the activity of gonococcus and “masks” the clinical manifestations of gonorrhea, while the combination of gonococcus and ureaplasma leads to greater activation of both pathogens. With such microbial associations, the processes of diagnosis and treatment become more complicated, which, in turn, contributes to the chronicity of the process. In any case, when an association of STI pathogens is identified, other infections are treated first, and then gonorrhea.
Urogenital trichomoniasis
The causative agent of the disease is the parasite Tr. vaginalis. Outside the human body, Trichomonas quickly lose their viability and die from drying out in a few seconds. In undiluted vaginal mucus and on underwear, Trichomonas remain alive until it dries (3–5 hours). Trichomoniasis in children is rarely observed, and mainly in teenage girls who have experience of sexual activity [14]. Family variants are possible (if someone is already sick), as well as infection of newborns from sick mothers during passage through the birth canal, which is relatively rare; in this case, vulvovaginitis and urethritis develop without specific symptoms. Due to the peculiarities of the vaginal epithelium and vaginal flora in newborn girls, vaginal trichomoniasis can be cured spontaneously. However, parasites sometimes persist in the urethra of girls for a long time (from 3 to 9 months). In children before puberty, urogenital trichomoniasis is rarely observed.
On average, it accounts for from 0.8 to 3.8% of cases [1, 4, 6].
Clinically, trichomonas vulvovaginitis is manifested by profuse liquid foamy discharge - from whitish to greenish in color. The disease is accompanied by severe itching of the vulva, possible admixture of blood in the discharge and the formation of erosions not only on the mucous membrane of the urogenital area, but also on the inner surface of the thighs.
None of the existing methods ensures the detection of trichomonas in all cases of the disease, therefore the key to successful diagnosis of trichomoniasis is a combination of various techniques (microscopy of stained and native preparations and cultures). Serological diagnostic methods have not received practical application, as they give a high percentage of false-positive results due to the presence of several trichomonas serovars, a low level of immune response and long-term persistence of positive serological reactions in those cured of trichomoniasis. The diagnosis of trichomoniasis is necessarily confirmed by the detection of the pathogen by direct microscopy of pathological material, as well as by culture on artificial nutrient media (cultural examination), which significantly increases the reliability of diagnosis, especially in children [1, 4, 12].
For the treatment of trichomoniasis, children are prescribed metronidazole per os: at the age of 1 to 5 years, 1/3 of a tablet containing 250 mg, 2-3 times a day; 6–10 years - 0.125 g 2 times a day; 11–15 years - 0.25 g 2 times a day for 7 days.
Cure of genitourinary trichomoniasis is established 7–10 days after completion of treatment using microscopic and cultural methods of examination [1]. Control examinations of recovered children are carried out monthly for 3 months.
Urogenital candidiasis
This is a lesion of the genitourinary organs by yeast-like fungi of the genus Candida. The predominant species is C. albicans, less commonly the cause of the disease is C. tropicales, C. krusei. C. albicans has the most pronounced pathogenic properties among the causative agents of candidiasis.
Urogenital candidiasis in children develops in the presence of exogenous and/or endogenous risk factors.
Factors contributing to the manifestation of the pathogenic and invasive properties of fungi of the genus Candida include congenital and acquired immunodeficiency conditions, general infections and intoxications, endocrinopathies, disruption of the internal environment and the normal microbial “landscape” of the mucous membranes [12].
Diagnosis of urogenital candidiasis in children is based on data from clinical, microscopic and cultural studies.
Clinical forms of candidiasis that are treated in venereology clinics refer to superficial lesions and are usually limited to the genital area. In children, urogenital candidiasis is detected less frequently than in adults, and usually occurs in the form of urethritis, balanoposthitis, vulvovaginitis and cystitis. The dominant complaints are itching, burning in the anogenital area, vaginal discharge in the form of white cheesy masses, and a cheesy coating on the genital mucosa. There is hyperemia of the skin and mucous membranes of the affected areas. Recurrent urogenital candidiasis practically does not occur in children [4, 6, 12].
The clinical diagnosis of candidiasis must be confirmed by identifying fungi of the genus Candida in preparations from pathological material using direct microscopy. Microscopic examination allows not only to determine the presence of fungi of the genus Candida with a predominance of vegetative forms (mycelium and budding yeast cells), but also to assess the composition of the microflora (pathogenic and opportunistic microorganisms).
Cultural testing, in turn, makes it possible not only to identify the pathogen, but also to assess sensitivity to drugs. A titer of fungal colonies in an amount of more than 103 CFU/ml is diagnostically significant. The detection of fungi in the absence of symptoms of the disease is not an indication for treatment, since they can periodically be detected in healthy people [1, 4, 5].
The tactics for managing children with urogenital candidiasis, according to the recommendations, include the prescription of pimafucin, which for vaginitis is applied in a dose of 0.5–1.0 ml of the drug 1 time per day until the symptoms disappear. Oral forms are used 0.5 tablets 2-4 times a day. Ketoconazole in tablets of 0.2 g is used orally with meals 2 times a day at the rate of 4–8 mg/kg body weight, and for body weights over 30 kg it is used in the same doses as for adults. Fluconazole is prescribed to children over 1 year of age at a rate of 1–2 mg/kg body weight per day.
The criteria for cure of urogenital candidiasis are the disappearance of clinical manifestations of the disease and negative results of microbiological examination. The observation period is set individually, depending on the duration, nature of clinical manifestations, and the prevalence of urogenital candidiasis [1, 12].
Urogenital chlamydia
Inflammatory diseases of the genitourinary organs of chlamydial etiology in children today do not attract due attention from doctors. However, urogenital chlamydia in children is more common than other STIs. The causative agent of the infection is Chlamydia trachomatis. The incubation period is 10–14 days. Clinically, chlamydial infection can occur in a variety of ways. Currently associated with Chlamydia trachomatis:
- diseases of the reproductive and urinary tract (vulvovaginitis, urethritis, cystitis, pyelitis, pyelonephritis);
- diseases of the respiratory tract and ENT organs (sinusitis, otitis, bronchitis and pneumonia);
- conjunctivitis;
- arthritis;
- Reiter's syndrome;
- diseases of the gastrointestinal tract (diarrhea);
- diseases of the cardiovascular system (myocardial damage).
Such a variety of clinical forms of chlamydial infection deserves close attention from doctors of many specialties [9].
Newborns can become infected perinatally. According to WHO, 60–70% of children born to mothers suffering from chlamydial infection are infected. For older children, the main routes of infection are household and sexual.
Initially, chlamydial infection affects the mucous membranes (eyes, oropharynx, urogenital tract, rectum). In newborns, Chlamydia trachomatis infection is often recognized based on symptoms of conjunctivitis and causes ophthalmia. Chlamydia trachomatis is the most common cause of subacute pneumonia, not accompanied by a rise in temperature and developing in the 1st–3rd month of a child’s life. In children aged 3–6 years, chlamydia most often occurs in the form of asymptomatic infections of the oropharynx, urogenital tract and rectum [11].
Urogenital chlamydia in sexually active adolescents also occurs without significant clinical manifestations. The most consistent symptom in girls is congestive hyperemia of the vulvar ring. The discharge is usually scanty, mucous, itching and burning during urination are mild. The asymptomatic or low-symptomatic course of chlamydia increases the risk of developing an ascending infection, which in children is already quite high due to the age-related characteristics of the body and the lack of natural protection factors for the urogenital tract. Ascending chlamydial infection can lead to the development of complications in the form of various inflammatory diseases of the upper genital tract (endometritis, salpingitis, tubo-ovarian abscess and pelvic peritonitis, as well as any combinations thereof) [4].
Testing for the presence of chlamydia, even in the absence of symptoms of the disease, is recommended for individuals at risk: sexually active adolescents; infants born to mothers who have not undergone treatment for chlamydial infection; children whose parents are infected [8].
There are the following methods for detecting chlamydia: immunofluorescence, enzyme immunoassay, serological, cultural and DNA diagnostics. Early detection of chlamydia is an important prerequisite for preventing possible complications. For rapid diagnosis of chlamydia, it is preferable to use the method of direct immunofluorescence with monoclonal antibodies. In this case, it is not free discharge that is subject to examination, but scraping of epithelial cells. If the test results are positive in childhood, a culture method for detecting Chlamydia trachomatis must be used to confirm the diagnosis.
For the treatment of children with urogenital chlamydia, erythromycin is used at a dose of 50 mg/kg body weight, divided into four oral doses over 10–14 days (for body weight less than 45 kg). For children weighing more than 45 kg, but under 8 years of age, erythromycin is used according to regimens developed for the treatment of adults. In children
For 8 years and older, azithromycin or doxycycline is used in adult dosages.
To ensure that the patient has been cured of urogenital chlamydia, a study should be carried out taking into account the diagnostic method [1]. Cultural examination is carried out no earlier than 2–3 weeks after the end of therapy. The criteria for cure of urogenital chlamydia are negative culture results and the absence of clinical symptoms of the disease.
Mycoplasmosis
Urogenital mycoplasmosis currently occupies a significant place among sexually transmitted diseases. In newborns, colonization of the genital tract with mycoplasmas occurs during childbirth. This infection is most often latent, asymptomatic, and often worsens under various stressful situations.
Clinical manifestations are erased. As a rule, patients report periodic, mild, spontaneous itching in the vulvar area. Against this background, mucous discharge from the genital tract appears.
Diagnosis of mycoplasmosis is based on culture diagnostic data [3, 13, 14].
The difficulty of treating the disease in childhood is due to the fact that tetracyclines and erythromycin are not used in pediatric practice. Treatment is carried out with the mandatory use of immunostimulating therapy (cycloferon), macrolides, cephalosporins in age-specific dosages.
Human papillomavirus infection
The incubation period for human papillomavirus infection ranges from 1 to 9 months, averaging 3 months. Genital condylomas have the appearance of single or multiple small papillary formations of pale pink color on a short stalk.
During the initial period of formation of genital warts, there are often no symptoms, and only when they grow rapidly do patients seek help from a doctor. The main clinical manifestation is itching.
Depending on the location and size of condylomas, there are several treatment methods. If condylomas are located in the area of the vulva or anorectal folds, they can be removed with the drug Solkovagin. This method is applicable for single condylomas. In case of a widespread, extensive process, its draining nature, the use of laser therapy is preferable. Also an important direction in the treatment of this pathology is the use of antiviral drugs and immunostimulating therapy [3, 10, 13, 14].
Thus, sexually transmitted infections are a serious problem in childhood. The high frequency of detection of acute inflammatory diseases of the external genital organs in children (both girls and boys), the great social significance of the consequences of these diseases for the gestational period - all this determines the need for increased attention to these patients on the part of doctors of various specialties (pediatricians, dermatovenerologists, gynecologists, urologists, etc.), as well as complex diagnostics and treatment of children with this pathology, allocating them to a special dispensary group.
Literature
- Borisenko K.K. Diagnosis, treatment and prevention of sexually transmitted diseases: Methodological materials. 3rd ed. M.: Association SANAM, 1998. 134 p.
- Vasiliev M. M. Diagnosis, clinical picture and therapy of gonorrheal infection // Russian Medical Journal. 1998. T. 6. No. 15. P. 994–998.
- Ivanov O. L. Skin and venereal diseases (handbook). M.: Medicine, 1997. 352 p.
- Kisina V.I. Urogenital sexually transmitted infections in children: clinical aspects of diagnosis and treatment // Attending Physician. 2004. No. 5.
- Kisina V. I., Mirzabekova M. A., Stepanova M. A., Vakhnina T. E., Kolikova G. G. Microbiological characteristics of vulvovaginal candidiasis in patients with sexually transmitted infections: Proceedings of the 4th symposium “New in dermatovenerology, andrology, gynecology: science and practice” // Bulletin of postgraduate medical education (special issue). 1999. P. 23.
- Kokolina V. N. Gynecology of childhood. - M.: Medpraktika, 2003. 268 p.
- Lipova E. V., Borovik V. Z. Problems of diagnosing gonorrhea in children: Proceedings of the 3rd symposium “New in dermatovenereology, andrology, gynecology: science and practice” // Bulletin of postgraduate medical education (special issue). 1998. C . 23.
- Malova I. O. Vaginal discharge in girls: etiology, clinical picture, diagnosis, treatment. Media/consilium. 2004.
- Molochkov V. A., Gosteva I. V., Goncharova L. I. The role of chlamydial infection in the development of chronic inflammatory diseases in children: Abstracts of the conference in memory of A. L. Mashkilleyson. M., 1997. P. 55.
- Pathology of the vagina and cervix/Ed. V. I. Krasnopolsky. M.: Medicine, 1997. pp. 68–146.
- Guidelines for the treatment of sexually transmitted diseases. US Centers for Disease Control and Prevention, 2002. M.: Sanam, 2003. 72 p.
- Skripkin Yu. K., Mordovtsev V. N. Skin and venereal diseases. M.: Medicine, 1999. T. 1. 880 p.
- Standard principles of examination and treatment of children and adolescents with gynecological diseases and disorders of sexual development / Ed. Academician of the Russian Academy of Medical Sciences, prof. V. I. Kulakova, prof. E. V. Uvarova. M.: Triada - X, 2004. pp. 50–56.
- Shaposhnikov O. K. Venereal diseases. M.: Medicine, 1991. 544 p.
O. A. Sokolova T. M. Logacheva T. G. Dyadik A. V. Malkoch, Candidate of Medical Sciences, City Clinical Hospital No. 14 named after. V. G. Korolenko, Russian Children's Clinical Hospital, Russian State Medical University, Moscow
Thrush during pregnancy
The development of vaginal candidiasis during pregnancy is dangerous for the expectant mother and the fetus. There is an increasing threat of the development of inflammatory processes during pregnancy, postpartum complications, and infection of the fetus, which can lead to fungal infection of its organs and even death. It is possible that the baby may become infected during childbirth. Treatment of thrush in pregnant women is complicated by the ban on taking antifungal drugs orally. Local treatment with vaginal tablets and suppositories is acceptable (Pimafucin is considered the safest among them during pregnancy). All the more important is the observance of personal hygiene rules, as well as protection from stress, proper nutrition with sufficient vitamins, walks, healthy sleep, which help strengthen the natural immune defense. If signs of thrush appear in a pregnant woman, she should immediately contact an obstetrician-gynecologist in order to carry out timely, adequate treatment and avoid complications.
For diagnosis and successful treatment of vaginal candidiasis, come to the Clinical Hospital on Yauza. You can see
prices for services Make an appointment
Causes of the disease
The main reasons for the development of urethritis in children are:
1. Reduced immune defense of the body.
2. Medical procedures:
- urethral smear;
- cystoscopy - examination of the bladder using a special device in the body of which a camera is mounted;
- catheterization - insertion of a special tube (catheter) into the bladder for rinsing, administering medications, and removing urine.
3. Hypothermia.
4. Poor nutrition (irritation and inflammation of the urethra occurs as a result of abuse of sour, spicy, salty, pickled foods).
5. Failure to comply with intimate hygiene rules.
6. Infectious and inflammatory pathologies of the genitourinary system:
- pyelonephritis (inflammation of the kidneys, usually caused by a bacterial infection);
- cystitis (inflammation of the bladder);
- inflammation of the external genitalia in girls;
- balanoposthitis (inflammation of the glans penis), prostatitis (inflammation of the prostate gland) in boys.
7. Congenital anomalies of the development of the urinary system.