Fast Facts About General Anesthesia
Here are some key points about general anesthesia. More detailed and supporting information can be found in the main article.
- The anesthesiologist usually administers a general anesthetic before surgery
- There are some risks associated with the use of general anesthetics, but they are relatively safe when used correctly
- Very rarely, a patient may experience unintentional awakening during surgery
- Side effects of general anesthesia may include dizziness and nausea
- The mechanisms by which anesthesia works are still only partially understood.
General anesthetics cause reversible loss of consciousness and analgesia necessary for surgery . The mechanism of action of anesthetics is not fully understood. There are several theories about this.
General anesthesia is essentially a medically induced coma, not sleep. Anesthetic drugs make the patient indifferent and turn off consciousness .
They are usually administered intravenously or by inhalation . Under anesthesia, the patient does not feel pain and may also experience amnesia.
The drugs will be administered by an anesthesiologist, who will also monitor the patient's vital signs during the procedure.
In this article, we'll look at a number of topics, including the possible side effects of general anesthesia, the risks involved, and some theories about how they work.
How long does dental anesthesia last?
On average, the freezing effect lasts 1-2 hours. However, its duration depends on the drug used: for example, injections with Novocaine anesthetize for no more than half an hour, Bupivacaine acts for at least 2 hours. Modern clinics mainly use anesthetics containing Articaine, which freezes tissue for up to 3 hours.
The infiltration anesthesia on the upper jaw will wear off in 45 minutes at most. This is due to the structure of the maxillary bone, which is looser and better supplied with blood.
Freezing after tooth extraction will last longer if the anesthetic contains a vasoconstrictor - a substance that constricts blood vessels and prolongs pain relief.
Story
General anesthetics have been widely used in surgery since 1842, when Crawford Long prescribed diethyl ether to a patient and performed the first painless operation.
On October 16, 1846, American dentist and surgeon Thomas Morton first administered ether anesthesia to a patient to remove a submandibular tumor.
In Russia, the first operation under anesthesia was performed on February 7, 1847 by Pirogov’s friend at the professorial institute, Fyodor Inozemtsev.
Pirogov himself performed the operation using anesthesia a week later. Over the course of a year, 690 operations were performed under anesthesia in 13 cities of Russia, 300 of which were performed by Pirogov!
Soon he took part in military operations in the Caucasus. Here, for the first time in the history of medicine, he began to operate on the wounded with ether anesthesia. In total, the great surgeon performed about 10,000 operations under ether anesthesia.
After operation
When to get up after surgery? The general rule is as early as possible! Don't linger! But of course, with the doctor's permission. Lying for a long time is fraught with the development of hypostatic pneumonia, acute thrombosis of the veins of the lower extremities, bedsores on the back, sacrum, and heels.
A case is described: a young patient, 23 years old, practically healthy, after a routine uncomplicated appendectomy, lay on his bed and did not want to get up (he was in pain, you see). On the third day I finally got up. Result: pulmonary embolism - instant death.
When can I return to normal work after anesthesia? After general anesthesia, after just two days, a person can perform normal work, work with complex mechanisms that require concentration, and drive a car! But the operating surgeons discharge the patient after 7-8 days, when the stitches are removed and the wound has healed. You can drink after anesthesia when your reflexes are restored and there is no nausea or vomiting.
We also recommend reading: Deep anesthesia: is there a great risk for pregnant women?
You can eat it the next day, the diet is gentle: you can’t eat spicy, salty, fried, canned food, sausages, or alcohol. The Pevzner diet is usually followed.
Side effects
Nausea is a common side effect of general anesthesia.
There are a number of potential side effects of anesthesia.
Some people may experience none, others several. None of the side effects are particularly long-lasting and usually occur immediately after anesthesia.
Side effects of general anesthesia include:
- temporary confusion and memory loss, although this is more common in older people
- dizziness
- difficulty urinating
- bruising or soreness from the IV
- nausea and vomiting
- trembling and chills
- sore throat due to breathing tube
Anesthesiology in dentistry
And a little more about outpatient anesthesiology and anesthesiology in dentistry, in particular. It is anesthesia (central anesthesia) that is used extremely rarely in modern outpatient dentistry and this is, as a rule, unjustified - like shooting sparrows from a cannon. The optimal option at the moment is to carry out sedation with simultaneous monitoring of the patient’s condition - monitoring. This enhances local anesthesia and reduces the amount of anesthetic required to achieve the effect. There are no contraindications to this method for people who have walked to the dentist’s office. According to his own feelings, the patient sleeps in the same way as during anesthesia, but wakes up quickly, is oriented and is able to move around on his own.
Risks
In general, general anesthesia is safe. Even very sick patients can be safely anesthetized. The surgical procedure itself involves much greater risk.
Modern general anesthesia is an incredibly safe procedure.
However, older adults and those undergoing lengthy procedures are most at risk for complications . These findings may include postoperative confusion , heart attack, pneumonia, and stroke.
Some specific conditions increase the risk for a patient undergoing general anesthesia, for example:
- obstructive sleep apnea, a condition in which people stop breathing while sleeping
- seizures
- existing heart, kidney or lung disease
- high blood pressure
- alcoholism
- smoking
- previous negative reactions to anesthesia
- medications that may increase bleeding - aspirin, warfarin , for example
- drug allergy
- diabetes
- obesity or overweight
Anesthesia for rhinoplasty
When performing rhinoplasty, it is important that the surgical procedure is as painless as possible.
The Dr. Alexander Markushin Rhinoplasty Center uses only modern, proven anesthesia methods.
The plastic surgeon planning the operation, after a careful examination, obtaining laboratory results, choosing a technique, and the anesthesiologist determine what type of anesthesia will be used for rhinoplasty.
Important!!!
The method of anesthesia for a specific operation is chosen by the attending physician and anesthesiologist, having familiarized themselves in detail with the test results, the presence of chronic diseases or possible allergic reactions.
Types of anesthesia used for rhinoplasty
Depending on the complexity of the upcoming operation and the individual characteristics of the patient’s body, the type of anesthesia is selected.
In total, three main methods of pain relief are used during nasal surgery.
- Endotracheal anesthesia.
- Local anesthesia.
- Intravenous method of pain relief.
Each technique has its own strengths and weaknesses, which makes it possible to combine them in case of emergency with other types of anesthesia.
Local anesthesia for rhinoplasty
The technique is used for minor operations designed to slightly correct the relief or shape of the nose. In addition, it is always used as an adjunct to general anesthesia, as well as independently if there are medical contraindications to general anesthesia.
Correction of the tip of the nose, removal or straightening of the hump can be performed under local anesthesia.
The tissues exposed to the surgeon are infiltrated with local anesthetics.
Deep infiltration blocks the passage of signals along nerve fibers, making the operation painless.
However, there are no restrictions for tactile or temperature impulses.
Important to remember!!!
Injections of lidocaine, marcaine or xylocaine are mainly used. Before this, an allergic reaction test may be performed to ensure that there is no allergy to the medications used. Otherwise, anaphylactic shock may occur.
For the following contraindications, local anesthesia should not be used:
- increased psychomotor excitability of the patient;
- negative reaction of the body to the use of a local drug;
- any type of mental disorder;
- chronic diseases of the cardiovascular or respiratory system during exacerbation.
For some patients, local anesthesia is not an option because it is difficult to watch the doctor cut facial tissue during surgery. Even a mentally stable person finds it difficult to remain calm without moving when he watches his nose get cut. Therefore, in common practice, a small amount of sedatives is administered during rhinoplasty under local anesthesia.
General anesthesia during nasal surgery
A plastic surgeon and an anesthesiologist choose general anesthesia for a complex, multifaceted operation or correction of serious defects received in an accident, during sports competitions, with burns of a large surface of the face, etc. The good thing about this method is that the patient is unconscious during anesthesia and does not feel any pain.
Before such operations, it is imperative to consult an experienced anesthesiologist so that problems do not arise during the surgeon’s work and after recovery from anesthesia. The patient must strictly follow all the doctor’s recommendations for rhinoplasty to be perfect.
Premedication
For some people, going under anesthesia is scarier than the surgery itself. To help such a patient, sedatives, antihistamines, and a tranquilizer can be administered intravenously half an hour before rhinoplasty. The dosage and time are prescribed by the anesthesiologist.
The patient must strictly follow the instructions received. Here it is important to maintain exact proportions, taking into account body weight and individual characteristics of the body. The drugs will not only calm you down, they will reduce the secretory function of biological fluids by the glands. This is very important during nose surgery.
Preoperative nutrition
A special diet will prepare the body for the upcoming stress. It is best if you have a full meal the day before rhinoplasty, and six to eight hours before you can have a small snack. Drinks can be consumed 6 hours before surgery.
During general anesthesia, this is an important precaution because vomiting can throw food debris into the lungs. A patient under general anesthesia cannot control internal processes because the muscles are relaxed and the sphincters are not able to delay the movement of juices from the stomach and intestines. Hydrochloric acid entering the lungs from the stomach can be fatal. Therefore, strict adherence to nutritional rules before surgery is an important part of patient preparation.
Intravenous anesthesia for rhinoplasty
The drugs are injected into a vein to quickly block the areas of the brain responsible for the perception of pain impulses. The calculation of the required amount of the drug is performed only by a highly qualified anesthesiologist, taking into account the concentration of the drug based on the patient’s weight.
The main advantage of intravenous anesthesia is the immediate effect of drugs. At the same time, the plastic surgeon must remember that the effect of anesthesia is strictly limited in time. It is necessary to carefully monitor how sensitivity changes so that, if necessary, administer another dose.
During the entire operation and after it, the patient is in the clinic under round-the-clock supervision of an anesthesiologist, who is ready to provide assistance in the event of any conditions that threaten the life and health of the patient.
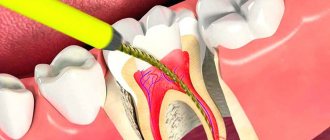
Endotracheal anesthesia for rhinoplasty
Complex anesthesia with prolonged action is ideal for complex, lengthy operations.
- At the first stage, the patient is given special medications intravenously.
- Then he is intubated (a special tube is inserted into the trachea) to ensure an uninterrupted supply of the required amount of air.
The procedure itself resembles a complex operation and is therefore performed only by qualified, specially trained personnel.
The main advantages of this method of anesthesia include:
- the possibility of free flow of oxygen into the lungs, necessary for the normal functioning of the body;
- getting the medicine exactly into the trachea allows you to select the required dose as accurately as possible;
- the maximum permissible level of oxygen in the blood can be accurately maintained to avoid pulmonary or heart failure;
- gastric juice will definitely not get into the lung tissue;
- a completely immobilized, unconscious patient allows the plastic surgeon to perform any manipulations without fear.
This anesthesia technique is ideal for rhinoplasty operations. The patient's condition is constantly monitored. If necessary, emergency measures can be taken immediately.
However, there are a number of contraindications for which endotracheal anesthesia is not used.
- Chronic diseases of the lungs, bronchi or tuberculosis in any form.
- Hemorrhagic diathesis.
- Acute inflammatory processes in the lungs or bronchi.
Important!!!
The presence of any neoplasms on the tissue of the soft palate or near the root of the tongue requires the use of a tracheostomy to avoid possible pathologies.
What complications can you encounter after anesthesia?
Regardless of the chosen method of anesthesia, each person’s body reacts individually to interference in its work. Therefore, you should be prepared for minor complications in order to immediately eliminate the negative consequences.
Possible complications are:
- A sharp drop in body temperature.
- If the dose of the medicine is incorrectly chosen, interruptions in the functioning of the heart may occur.
- If stomach contents reflux into the lungs, resuscitation should begin immediately.
- The onset of profuse vomiting, provoked by the action of medications.
- Damage to peripheral nerve endings.
- Injury to soft tissues of the respiratory tract during intubation.
The doctor reacts instantly to any negative consequences of anesthesia, so the risk of serious complications is minimal.
Dr. Alexander Aleksandrovich Markushin has performed thousands of operations of varying complexity with consistently high results.
Modern medicine provides almost one hundred percent guarantees that there will be no negative effects on the body after anesthesia.
Most often, myths circulating among people are born from tales that came from the last century, when painkillers were not so perfect.
Having followed all the doctor’s instructions to prepare for the operation, you don’t have to worry that there will be serious difficulties in recovering from anesthesia. A qualified anesthesiologist is always present at each operation in order to immediately correct the work if necessary.
Individual work with each patient eliminates even minimal danger.
Unintentional intraoperative awakening
This refers to rare cases where patients report remaining conscious during surgery, long after the anesthetic should have taken effect . Some patients are aware of the procedure itself, and some may even feel pain.
Unintentional intraoperative awakening is incredibly rare, affecting approximately 1 in every 19,000 patients under general anesthesia.
Because of the muscle relaxants used at the same time as anesthesia, patients are unable to let their surgeon or anesthesiologist know that they still know what is happening.
Unintentional intraoperative awakening is more likely during emergency surgery.
Patients who experience unintentional intraoperative awakening may suffer from long-term psychological problems. Most often, awareness is short-lived and only sounds, and occurs before or at the very end of the procedure.
According to a recent large-scale study of this phenomenon, patients experienced involuntary twitching , stabbing pain, pain, paralysis and suffocation, among other sensations.
Because unintentional intraoperative awakening is rare, it is unclear exactly why it occurs.
Horror stories about anesthesia
No one will ask a traumatologist about gynecological diseases. However, questions about anesthesiology are asked to doctors of any specialty, who, as a rule, understand it no more than other ordinary people - anesthesiology is a very specific subject. Once I came across this: a patient came for tooth extraction under anesthesia, paid for the extraction and anesthesia, but refused the anesthesia, because a relative (therapist) said that EVERYONE dies from anesthesia.
Patients who undergo operations under general anesthesia write with pleasure in various forums how afraid they are of “general anesthesia,” and a chorus of well-wishers echoes them: “yes, yes, anesthesia is like dying a little,” “anesthesia has a lot of contraindications,” “maybe allergic shock!” It seems that you can do without anesthesia and there is no need to monitor the patient’s somatic condition during the most complex and traumatic interventions. At the same time, no one writes that pain has a very, very strong effect on health, that not everything can be tolerated, that a surgeon is a person who only performs an operation, and an anesthesiologist is precisely the specialist who cares for the patient.
Types
There are three main types of anesthesia . General anesthesia is just one of them.
Local anesthesia is another option. It is done before minor surgeries such as toenail removal. This reduces pain in small, focused areas of the body, but the person receiving treatment remains conscious.
Regional anesthesia is another type. It numbs the entire part of the body - the lower half, for example, during childbirth. There are two main forms of regional anesthesia: spinal anesthesia and epidural anesthesia.
Spinal anesthesia is used for operations on the lower extremities and abdomen. The anesthetic is injected through a special very thin needle into the intervertebral space of the lumbar region . Epidural anesthesia is used for long-term pain relief. Can be used for operations on the chest, abdomen, and lower extremities. During an epidural, a thin plastic catheter is inserted through which a local anesthetic is injected. Pain relief can last as long as needed.
What to do if the numbness does not go away?
There is no need to be afraid of prolonged tissue numbness; after a couple of hours, sensitivity will definitely return. If numbness in your teeth, tongue, jaw, or nose after anesthesia does not go away by the end of the day, you should call your doctor and report the situation. In rare cases, complications of anesthesia occur in the form of paresis and paresthesia - disruption of tissue innervation. They appear when a nerve is accidentally injured by a needle. In this case, you need to visit a doctor who will prescribe treatment for the pathology. When the anesthesia of the tooth wears off, discomfort and unpleasant sensations may appear.
In most cases, tissue anesthesia passes without a trace, so if there are indications for anesthesia, there is no need to be afraid to perform it. If you have had an unpleasant experience with pain relief or need emergency treatment under anesthesia, you should simply tell your dentist about it. The doctor will definitely take into account your wishes and will be able to control the amount of the drug and the duration of its action.
Local vs General
There are a number of reasons why general anesthesia may be chosen over local anesthesia.
This choice depends on age, health and personal preference.
The main reasons for choosing general anesthesia are:
- The procedure will likely take a long time.
- There is a possibility of significant blood loss.
- This may affect breathing, for example during breast surgery.
- The procedure will make the patient feel uncomfortable.
- It is difficult for the patient to maintain a forced position during surgery.
The purpose of general anesthesia is to induce:
- pain relief or elimination of the natural response to pain
- amnesia or memory loss
- immobility or elimination of motor reflexes
- dream
- relaxation of skeletal muscles
However, the use of general anesthesia poses a higher risk of complications than local anesthesia. If the surgery is minor, then the patient is offered local anesthesia, especially if he has a condition such as sleep apnea or other risk factors.
What is general anesthesia?
What is general anesthesia or, as Russian language “experts” say, “general anesthesia”? If you don’t go into details, but highlight the most important thing for the patient, then general anesthesia is anesthesia performed by an anesthesiologist. The patient does not necessarily have to sleep during general anesthesia. Sometimes a nap is enough—medically induced calm and indifference to the outside world. This condition is called sedation. Sometimes, due to such serious sedation (sedation), the patient falls asleep on his own, but at the right moment wakes up - at the doctor’s command he performs simple actions (open his mouth, turn his head, raise a limb, etc.).
Preoperative assessment
Before undergoing general anesthesia, patients should undergo a preoperative assessment to determine the most appropriate medications, their amount and combination.
Some of the factors that should be examined in the preoperative assessment include:
- body mass index (BMI)
- disease history
- age
- medications taken
- time before anesthesia
- alcohol or drug use
- use of pharmaceuticals
- examination of the oral cavity, teeth and respiratory tract
- cervical spine mobility study
It is important that you answer these questions accurately. For example, if a history of alcohol or drug use is not mentioned, insufficient anesthesia may be given, which could lead to dangerously high blood pressure or unintentional intraoperative awakening.
Methods used in dental practice
How long it takes for the anesthesia effect to disappear depends directly on the method of anesthesia used. The sensitivity of tissues is restored most quickly when using an application. The doctor applies a special gel to the area of upcoming manipulations, which “freezes” for about fifteen minutes.
If the anesthetic medication was administered using a syringe and needle, the area will remain numb for up to one to three hours. The exact time is determined by the location of the treated area, the dose and type of drug.
Stages
The Gödel classification, developed by Arthur Ernest Gödel in 1937, describes four stages of anesthesia. Modern anesthetics and updated methods of drug have improved the speed of onset of anesthesia , overall safety and recovery, but the four stages remain essentially the same:
General anesthesia is similar to a comatose state and different from sleep.
Stage 1 or induction . This phase occurs between the administration of the drug and loss of consciousness. The patient moves from analgesia without amnesia to analgesia with amnesia.
Stage 2, or arousal stage . The period after loss of consciousness, characterized by agitated and delirious activity. Breathing and heart rate become erratic, and nausea, dilated pupils, and holding your breath may occur.
Due to irregular breathing and the risk of vomiting, there is a danger of suffocation. Modern fast-acting drugs are aimed at limiting the time spent on the 2nd stage of anesthesia.
Stage 3 or surgical anesthesia : muscles relax, vomiting stops, breathing is suppressed. Eye movements slow and then stop. The patient is ready for surgery
Stage 4, or overdose : if too much anesthetic has been administered, then depression of the brain stem occurs . This leads to respiratory and cardiovascular collapse.
The anesthesiologist's priority is to get the patient to stage 3 anesthesia as quickly as possible and keep him there throughout the operation.
Is it possible to die from anesthesia?
The mortality rate from sedation does not exist, and from anesthesia it is so low that the mortality rate from local anesthesia exceeds it. Addiction to drugs and alcohol is not a contraindication for dental treatment under sedation, although it complicates the anesthesiologist’s task. And, finally, another professional saying: “It’s not the anesthesia that’s scary, it’s the anesthetizer that’s scary.” And an incompetent person giving advice.
Author: anesthesiologist-resuscitator Kokhan Arkady Mironovich
Tooth freezing while breastfeeding
Some mothers are afraid to visit dentists while breastfeeding, thinking that anesthetics through milk can have a negative effect on their children. However, there is practically no reason for this.
Neither the anesthetic itself nor the accompanying possible toxic substances are reflected in the milk, because they act only on a certain area of the jaw and are not introduced into the blood.
But in order to further reduce the likelihood of negative effects of drugs on babies, dentists recommend feeding them before visiting the doctor, and also preparing in advance the required amount of milk for the next feeding of the baby. Thus, the toxic substance will not have the opportunity to enter the child’s body.
Category Miscellaneous Published by Mister dentist