Types of general anesthesia
Depending on the method of administering drugs for general anesthesia, inhalation and intravenous anesthesia are distinguished.
With inhalation anesthesia, the anesthetic enters the body through the respiratory tract; with intravenous anesthesia, it is injected into the bloodstream. A combined method involving inhalation and intravenous administration of the drug is actively used. To maintain external respiration, an endotracheal tube or laryngeal mask is used. The first method is called intubation anesthesia (or endotracheal), the second - mask. You will not need deeper knowledge about the specifics of an anesthesiologist’s work; it is much more important to understand how to properly prepare for anesthesia.
Good general anesthesia is the result of the consolidated efforts of the anesthesiologist and the patient. Therefore, we recommend that you read the next section very carefully.
Anesthesia today
Today there are three main types of anesthesia - local, general and spinal. For quick interventions and for children, inhalation anesthesia is used - the child inhales an anesthetic inhalation mixture through a mask and falls asleep. Intravenous anesthesia is used for long and difficult operations.
By the way
Epidural anesthesia does not work for 1 in 20 patients, and red-haired people need 20% more anesthetics to stop their pain. In traumatology, regional anesthesia is used - a local anesthetic is injected into the area of the nerve, providing complete anesthesia of the limb. Epidural anesthesia is very popular for facilitating the labor process, since the patient can either remain conscious or doze off under the influence of drugs.
Spinal anesthesia is difficult to control and is rarely used, but the patient is completely switched off and does not feel pain. Anesthesia with preserved consciousness is used only in special cases, most often in neurosurgery, if it is necessary to maintain the patient’s consciousness and communicate with him during the operation. Oral (through the mouth) and rectal (through the anus, using an enema) anesthesia is practically not used today. The intramuscular method of pain relief is also becoming a thing of the past.
Before general anesthesia: preparation
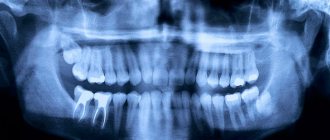
Preparation for surgery under anesthesia has a great influence on the effectiveness and safety of general anesthesia and the course of the postoperative period. You will have to undergo a comprehensive diagnostic examination, including detailed blood tests, coagulogram, and ECG. According to indications, consultations with narrow specialists are prescribed.
The presence of chronic diseases of the respiratory and cardiovascular systems is of great importance. Be sure to tell your doctor about the following diseases:
- bronchial asthma;
- chronic obstructive bronchitis;
- arterial hypertension;
- IHD;
- history of stroke.
Do not under any circumstances hide the fact that you have a history of chronic diseases and acute vascular events (heart attack, stroke). Not only the outcome of the operation, but also your life depends on this! Also provide your doctor with a complete list of medications you take, including “harmless” analgesics for headaches or menstrual pain.
As practice shows, excess weight negatively affects the rate of recovery after operations under general anesthesia. If you are planning plastic surgery in advance, pay attention to weight loss issues. It is advisable to quit smoking in about six months. If you have not done this, stop smoking a week before the operation, but you should not “quit” the day before anesthesia - this may complicate the rehabilitation period.
On the eve of the operation, pay special attention to nutrition and hydration. You should not drink alcohol 24 hours before plastic surgery. On the day before surgery, you should limit yourself to breakfast and lunch. On the day of surgery, eating and drinking is strictly prohibited!
"Frivolous" anesthesia
Many people associate anesthesia exclusively with serious operations, when a person is euthanized and completely anesthetized. However, everyone experiences anesthesia during less significant interventions, for example, in the dentist's office.
Article on the topic
Dental anesthesia, or what you need to tell your dentist about And despite the fact that there are modern safe drugs for local anesthesia, carpule technology is used, when the medicine is already prepared and packaged in syringes at the factory, not everyone has dental anesthesia without complications.
The anesthetic risk group includes 30% of those who came for dental treatment. These are people with cardiovascular diseases, allergies, and endocrine pathologies. The condition of the liver and kidneys plays an important role - you need to tell your doctor about the presence of any of these diseases, or better yet, provide medical documents.
Also vulnerable are the elderly, pregnant women, children and those who are very afraid of dental treatment.
After general anesthesia
Even after a good general anesthesia, in the first hours there is short-term confusion, disorientation in space and time, drowsiness, nausea, and dizziness. As the anesthetic drugs wear off, pain appears in the postoperative wound, but it is successfully relieved by the administration of strong anesthetics.
After general anesthesia with an endotracheal tube, patients complain of pain and sore throat caused by irritation of the mucous membrane of the upper respiratory tract, but this symptom, like nausea, passes very quickly. As a rule, patients feel well 3-4 hours after surgery, and on the second day they leave the clinic and return home.
What questions should you ask before vein removal?
Before you go on the operating table, do not hesitate to ask the doctor anything that concerns you. You must fully understand what the essence of the operation is, what the risks are, how long it will take to recover after surgery, what restrictions phlebectomy imposes, and whether you will be able to fully perform your usual activities. Find out all the details regarding preoperative preparation during the consultation. Usually the doctor issues a special reminder, but it would be useful to clarify.
Tell us about allergies, concomitant diseases, experience of previous operations, medications, vitamins, hormonal contraceptives that you take. All this is important when deciding on the method of treatment and anesthesia.
Indications for general anesthesia
Some cases in practical surgery and dentistry are a direct indication for the use of general anesthesia during therapeutic procedures. However, even if they are available, the use of anesthesia raises many doubts and questions about the general health of the patient, which may have contraindications. To eliminate all risks, the patient undergoes a certain examination of the body, based on the results of which the doctor decides on the advisability of this type of anesthesia.
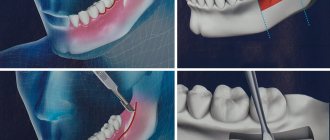
The following types of dental treatment can be performed under sedation or general anesthesia:
- extraction of 3 molars, which are located in the jaw bone in an extremely complex manner, which involves drilling and crushing tooth tissues and roots, which have a complex and tangled structure;
- bone grafting with immediate implantation;
- the need for prosthetics or implantation of several dental units;
- one-stage removal of several teeth;
- elimination and treatment of a large volume of carious lesions on the dental surface;
- injuries of the maxillofacial apparatus, requiring a large scale of restoration work;
- treatment of advanced forms of pulpitis or widespread periodontitis;
- surgeries on the temporomandibular joint;
- a burdened allergy history, which does not allow treatment with local anesthetics;
- the patient has a pronounced gag reflex;
- insurmountable fear of dental procedures, accompanied by characteristic sounds, smells and tactile sensations;
- the patient has severe mental illness (schizophrenia, mental retardation);
- children under 3 years of age, which is due to inadequate patient contact and the presence of a large volume of dental work;
- genetic pathologies (autism, Down syndrome);
- patients with somatic pathologies in a compensated state to prevent exacerbation, for example, hypertension or neurasthenia;
- epilepsy.
In cases of treatment in government institutions with a hospital, you will always be persuaded to undergo treatment under anesthesia followed by hospitalization, since this is strictly regulated by the internal regulations of hospitals.
In paid non-state clinics, all these types of treatment will be carried out only under sedation and without hospitalization, since there is no need to extend the stay and duration of treatment.
The list of indications is quite large, but it may have limitations. Whether it is possible to treat teeth under anesthesia in a particular case will be determined only by an experienced anesthesiologist, who must be on the staff of specialists in a modern dental clinic that provides comfortable and effective service.
When can you eat after a light filling?
Today the most popular filling is light. Almost all dentists prefer it. On the first day after the procedure, the filling is extremely sensitive to any influences, since the material has not yet completely hardened. It is better to eat food after 1-2 hours, but it is undesirable to use foods and drinks containing dye, since the filling material easily absorbs coloring pigments.
What foods should be excluded on the first day after treatment:
- coffee, tea, red wine;
- beet;
- dark berries (blueberries, blueberries);
- various sauces.
Food should not be too hot or cold.
After operation
— To avoid severe swelling and bleeding during the first 24 hours after surgery, it is necessary to apply an ice pack to the cheek on the side of the operation for 15-20 minutes with breaks of 30-40 minutes.
- Rinsing your mouth when bleeding is unacceptable!
— After sinus lift surgery, you should not drink through a straw, blow your nose vigorously, or puff out your cheeks.
- To reduce the likelihood of nosebleeds (after upper jaw surgery) and reduce post-operative swelling, you should sleep with your head elevated (add an extra pillow) for several days after surgery.
— It is not recommended to use tobacco products 1 week before and 2 weeks after surgery.
— It is prohibited to drive a car on the day of surgery with premedication.
- It is not recommended to eat until the anesthetic wears off. In the first days after surgery, it is recommended to eat soft, non-hot foods.
— It is not recommended to drink alcohol, coffee, or strong tea to avoid the negative effects of these drinks on blood circulation and wound healing.
Who gets dental treatment under general anesthesia?
The vast majority of visitors to dental clinics who are recommended to have their teeth treated under general anesthesia are children from 3 to 5 years old. Adults often prefer local anesthesia because they control themselves during the procedure, but they often opt for sedation. However, kids cannot sit still when they see oral treatment tools. Sudden movement of the patient during surgery can, in turn, cause serious harm.
Modern general anesthesia, during which the patient’s teeth are treated, is allowed starting from the 1st year and, subject to basic recommendations, is safe. However, age is not the main indication for general anesthesia, since each case requires an individual approach.
The cardiovascular system
It is difficult to separate the effects of nicotine on the central nervous system and the cardiovascular system, they are so interrelated.
One of the typical manifestations of nicotine stimulation is a pathological increase in cardiac muscle activity due to the effect of nicotine on the conduction system of the heart. This effect consists of increasing the contractile activity of the heart, vascular tone, and blood pressure. The myocardium in such situations consumes more oxygen, and this is precisely the problem - due to insufficient respiratory function.
Nicotine is a tissue poison, and one of its toxic properties is that it disrupts the ratio of calcium and sodium in cells, leading to hyperexcitability of cardiomyocytes (heart cells) with the subsequent occurrence of arrhythmia and ischemic foci.
Oral hygiene
Regardless of the size or number of implants, they must be cared for as if they were regular teeth. Brush and floss your dental implants twice a day. Use special fluffy dental floss (for example, Oral-B superfloss or ultrafloss).
When brushing your teeth, pay special attention to the back teeth and between teeth. Use a soft or medium-hard brush. In addition, use an irrigator for additional deep cleaning of the interdental spaces with water irrigation.
There are special brushes that can be used to clean interdental spaces - dental brushes. Ask your dentist about them - in some cases they are not recommended.
Visit your dental hygienist twice a year; they are the only ones who can clean your implants as thoroughly as necessary. Regular visits to the dentist are very important. Your dentist will check the condition of your gums, jaws and implants.
Smoking is bad for your health and for dental implants, too. To have a good prognosis for the lifespan of your implants, it would be a good idea if you stopped smoking.
Purpose of general anesthesia in dentistry
General anesthesia is a rather complex and highly responsible intervention in the human body, and therefore requires fundamental knowledge and experience of a highly qualified specialist, modern technical and drug support, as well as appropriate hospital conditions.
All dental clinics that plan to conduct any types of treatment under anesthesia must have a license to provide these services. Ideally, general anesthesia should only be used in a hospital setting, with an intensive care unit or ward available in case of any complications.
The task of the anesthesiologist is to provide the following conditions to the patient:
- analgesia;
- amnesia;
- neurovegetative protection;
- the most convenient conditions for performing dental procedures that are invasive and traumatic.
The anesthesiologist's first priority is always maximum patient safety, avoiding complications and preventing the consequences of anesthesia. It should be remembered that general anesthesia is always associated with a certain percentage of risk, although in modern practice it is extremely small.
Respiratory system
Here again, it is very difficult to separate respiratory problems in smokers from the pathology of the cardiovascular system.
Smoking leads to chronic tissue hypoxia, and during surgical interventions it is one of the priority risk factors for such disorders as: deterioration of pulmonary ventilation, widespread reaction to surgical trauma, the appearance of atrial fibrillation and other types of arrhythmias, the development of increased bleeding, disseminated intravascular coagulation syndrome, sympatho-adrenal crisis. A smoker's lungs have a narrowed lumen, which makes intubation difficult and leads to the development of broncho- and laryngospasm. Viscous thick mucus in combination with chronic congestion causes intraoperative and early postoperative complications, especially against the background of intubation anesthesia: respiratory arrest, mechanical blockage of the lumen of the lungs, pneumonia, atelectasis, emphysema. It is during this period that it is important that mucus is easily removed from the lungs using suction or naturally. For this purpose, after extensive surgical interventions, active and passive breathing exercises are prescribed, which are effective in non-smokers or those who have quit smoking. Smokers have to additionally prescribe medications to thin and stimulate the outflow of mucus. For an anesthesiologist, indicating that a patient smokes is an extra headache. This means that you will have to adjust the dose of oxygen, analgesics, and muscle relaxants. It threatens complications in the early postoperative period, for example, early removal of the endotracheal tube can lead to respiratory arrest due to obstruction by thick mucus. It is difficult to keep such patients in bed - in order to get their hands on the coveted cigarette, they are ready to commit serious violations of the regime. And finally, postoperative wounds in smokers heal much worse compared to non-smokers, and the risk of unsuccessful surgery increases by 4-10 times, depending on the intervention.
What tests will you be asked to undergo before vein surgery?
In addition to the mandatory Doppler ultrasound, you will have to undergo tests:
- for blood clotting, group and Rh factor,
- HIV, syphilis and hepatitis,
- blood chemistry,
- general urine analysis.
They also prescribe fluorography and ECG, consultation with an allergist, anesthesiologist and therapist, gynecologist or urologist if the groin area is being operated on. Based on the results of these examinations, the surgeon decides whether the patient is ready for surgery.
Eating
Avoid chewing hard candy, ice, or other hard foods (such as hard chocolate or dry fish) as they may loosen or break the abutment screw.
Avoid foods such as caramel or toffee, as they may stick to the crown and cause the abutment screw to loosen.
Do not open bottles or crack nuts with your teeth for the same reasons.
Wear protective sports mouth guards when participating in sports and avoid direct blows to the face.
Refrain from grinding your teeth. If creaking occurs unintentionally or during sleep (bruxism), notify your dentist and he will make you a thin night guard.
The length of their service depends on the quality and regularity of care for implants.
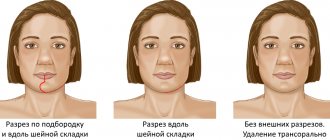
Before and after implantation
Complications after general anesthesia
Modern medications and technical equipment are at the highest level in anesthesiology, but there is always a risk of any complications, which patients should know, doctors should take into account and warn. Each human body is individual and, under certain conditions, unpredictable, so it is difficult to give a 100% guarantee of the successful completion of any surgical operation that was accompanied by general anesthesia.
In the practice of anesthesiologists, the following types of complications are encountered, which, in most cases, are noted during the recovery of consciousness after using a drug for anesthesia:
- dizziness, nausea, vomiting;
- psychomotor agitation and confusion;
- severe headache;
- trembling throughout the body;
- muscle pain (back, neck, limbs);
- severe allergic reactions;
- injury to the tongue, lips or teeth (usually characteristic of endotracheal anesthesia);
- infection of the lower respiratory tract, which occurs due to incorrect tracheal intubation;
- fluctuations in basic vital signs (blood pressure, pulse, saturation).
There is also a rate of severe brain damage and mortality, which necessitates the presence of resuscitation equipment and appropriate medications. Informed patients must make their own decision about whether to treat their teeth under general anesthesia , since the doctor cannot guarantee absolute well-being. The best prevention of these excesses is considered to be thorough preparation of the patient, exclusion of contraindications and compliance with all doctor’s recommendations. Modern anesthesia in dentistry reduces the rate of complications to a minimum.
Important! None of these types of anesthesia are used in our clinic, only sedation.
Important! Establishing, licensing and maintaining a full-fledged anesthesiology department requires huge monthly costs.
People usually criticize and dissuade from performing sedation only in those clinics where Rospotrebnadzor issued a refusal and failed to obtain accreditation for this type of licensing.