The dental organs are an integral part of the masticatory apparatus.
The chewing apparatus of an adult contains 32 dental organs (16 each in the upper and lower jaws).
The dental organ consists of a tooth; the socket and the adjacent jaw, covered with the mucous membrane of the gums; ligamentous apparatus that holds the tooth in the socket; vessels and nerves.
In the tooth there are:
- crown (thickened part protruding into the tooth cavity);
- neck of the tooth (narrowed part adjacent to the crown, surrounded by gum);
- root (part of the tooth located inside the jaw socket).
TOOTH PULP
There is a cavity inside the tooth that resembles the shape of a crown, and at the root of the tooth it continues in the form of a canal. The root canal ends at the apex of the tooth root with an opening. The tooth cavity is filled with loose connective tissue, rich in blood vessels and nerves - pulp. The dental pulp is divided into crown and root parts. The pulp of the tooth crown is represented by loose connective tissue with a delicate network of collagen and precollagen fibers with a large number of cellular elements. In the tooth root pulp, collagen structures are denser, thicker and oriented longitudinally along the neurovascular bundle.
Based on the cellular composition of the pulp, they are divided into: peripheral, subodontoblastic and central layers.
The peripheral layer consists of specialized cells - odontoblasts, which take part in the metabolic processes of enamel and dentin. They are located in several rows.
The odontolast has an elongated pear-shaped shape. It has a peripheral protoplasmic process (or dentine), which runs in the dentinal tubule to the dentinoenamel junction, and short lateral processes that anastomose with neighboring cells in the early stages of differentiation.
The subodontoblastic and central layers consist of small, poorly differentiated stellate cells connected to each other by short processes. The pulp contains many fibroblasts that participate in the formation of a fibrous capsule that limits the focus of inflammation.
In the central layers there are cytoplasmic cells - histiocytes. During inflammation, they acquire the ability to move and phagocytose and are called macrophages.
The blood supply to the pulp is provided by blood vessels that penetrate into it through the opening of the apex of the tooth root and through additional canals from the periodontium. The lymphatic system in the pulp is presented in the form of slits, capillaries, and vessels. The outflow of lymph from the pulp occurs in the submandibular and mental lymph nodes. Arterial trunks accompany veins. The pulp vessels have numerous anastomoses. Through the apical foramen, sensitive pulpy and non-pulse fibers of the trigeminal nerve pass, which innervate the pulp, forming plexuses.
The dental pulp has a trophic, protective and plastic function. The trophic function is carried out due to the developed network of blood and lymphatic vessels; protective - due to histiocytes, plasma cells; plastic is the participation of the pulp in the formation of dentin.
The bulk of the tooth is dentin, which surrounds the tooth cavity. In the area of the tooth crown, dentin is covered with bright white enamel. The dentin of the root is covered with cement.
PERIODONTIUM
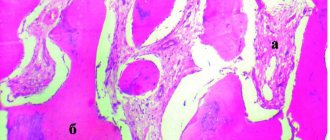
The root of the tooth is held in the socket by connective tissue fibers that make up the root membrane or periodontium.
The periodontium is located in a narrow, slit-like space between the tooth root and the jaw bone. The thickness of the periodontium is 0.15-0.25 mm. With age, as well as from mechanical load, the thickness of the periodontium changes and amounts to 1.2-1.2 mm.
The basis of periodontal connective tissue are bundles of interdental and cemento-alveolar fibers, which are woven, on the one hand, into the compact plate of the alveoli, and on the other hand, into the cementum of the tooth root. In the area of the tooth neck, fibrous fibers have an almost horizontal direction and include numerous collagen fibers, circularly covering the cervical area (circular ligament). The apical periodontium contains more loose connective tissue and cellular elements. Fibrous fibers in the area of the tooth apex are represented by looser, more delicate bundles and are arranged radially; with the help of the fibers, the tooth is suspended and fixed in the bone bed.
The blood supply to the periodontium is abundant and it has a fairly developed lymphatic network. Periodontal vessels form several plexuses (external, middle, capillary) in the root area. Cellular elements are represented by fibroblasts, mast cells, plasma cells, histiocytes, cementoblasts, osteoblasts, and epithelial remnants of the neoplastic epithelium. The main function of the periodontium is support and retention. In addition, the periodontium distributes and regulates pressure on the tooth (shock absorbing), has a plastic function due to cellular elements and a barrier function (due to the unique anatomical structure and resistance to adverse environmental influences). The reflexogenic function of periodontium is also highlighted.
Periodontal ligament diseases
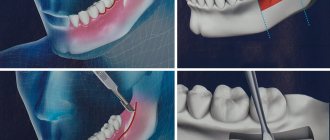
Inflammatory processes can develop in the periodontal ligament caused by trauma (for example, when biting a very hard object), pathogens or medications used in dental treatment and entering the periodontium through the root canal.
- Acute apical or apical periodontitis. Periodontal damage causes an intense tissue response, usually limited to the periodontal ligament. The inflammatory process begins, accompanied by constant increasing pain. Pus accumulates near the root tip, the outflow of which is difficult. Without the intervention of a doctor, the process gets worse and often leads to serious complications.
- Chronic apical periodontitis (apical granuloma). It may be a consequence of the acute form if the pus finds an outflow through the root canal of the tooth. It is also often an independent disease caused by pulp necrosis.
Chronic forms of periodontitis in most cases are asymptomatic and are detected during X-ray examination or during exacerbation.
Kozlov V. I., dental surgeon of the highest category [3]
- Abscess. Exacerbation of the chronic form due to imbalance - for example, a new traumatic effect or a decrease in the body's immunity [3, 4].
The periodontal ligament plays an important role in the gingival tissue complex. The ability of teeth to withstand chewing loads without loosening or falling out depends on it. To maintain a full set of teeth for many years, if you have any problems with periodontal disease, you should immediately contact your dentist.
List of sources:
- Sakharuk N. A., Volkova M. N. Periodontal diseases: clinical picture, diagnosis, prevention and treatment: Educational manual. Vitebsk: VSMU, 2014. // URL: https://elib.vsmu.by/bitstream/123/6947/1/Sakharuk-NA_Bolezni%20periodonta%20klinika%20diagnostika%20profilaktika%20i%20lechenie_2014.pdf (access date 10.12. 2020).
- Samusev R.P., Dmitrienko S.V., Krayushkin A.I. Fundamentals of clinical morphology of teeth. M.: LLC Publishing House "ONICS 21st Century": LLC "World and Education", 2002. // URL: https://iknigi.net/avtor-rudolf-samusev/21113-osnovy-klinicheskoy-morfologii-zubov- uchebnoe-posobie-rudolf-samusev/read/page-17.html (accessed 12/10/2020).
- Expert article on periodontitis by dentist-surgeon V.I. Kozlov // URL: https://probolezny.ru/periodontit/ (access date 12/10/2020).
- Borovsky E.V. Therapeutic dentistry: a textbook for students of medical universities. M.: Medical Information Agency, 2003. // URL: https://www.booksmed.com/stomatologiya/153-terapevticheskaya-stomatologiya-borovskij.html (access date 12/10/2020).
DENTINE
Dentin in its structure resembles coarse-fibrous bone tissue, consisting of a basic substance penetrated by a large number of dentinal tubules. The main substance of dentin consists of collagen fibers, between which there is an amorphous adhesive substance. The outer layer of dentin (with a radial arrangement of fibers) is called mantle; the inner layer with a tangential arrangement of fibers is peripulpar. Dentinal tubules (tubules) have the shape of round, oval tubes. They begin in the tooth cavity, bending in a wave-like manner, pass through the thickness of the dentin and end in flask-shaped swellings in the area of the dentino-enamel junction.
In the lumen of these tubules there are dentinal processes of odontoblasts. Dentin contains 70-72% inorganic substances (mainly phosphate and calcium carbonate), and 28-30% is water and organic matter (proteins, fats and carbohydrates).
Tooth enamel Tooth enamel is the hardest tissue of the human body. In the area of the cusps of the tooth crown there is the thickest layer of enamel; towards the cervical area the thickness of the enamel decreases. Enamel prisms are the main structural formation of enamel. The enamel prism is a faceted cylindrical fiber that begins at the dentinoenamel junction.
It bends in an S-shape, runs radially and ends on the surface of the tooth crown. Enamel prisms are connected into bundles (10-20 each), directed radially from the dentinoenamel junction to the outer surface. The thickness of the prisms is from 3 to 6 microns. Each prism contains thin cytoplasmic fibers that form an organic mesh, in the loops of which crystals of mineral salts are located.
Enamel prisms and interprismatic spaces (in electron microscopic examination) consist of strictly oriented hydroxyapatite crystals arranged in a certain order, the length of which ranges from 50 to 100 nm.
Most of the tooth enamel consists of inorganic matter (95%), organic (1.2%) and water (3.8%). Tooth enamel contains 96.5% mineral salts, of which about 54% are phosphorus and calcium (17% and 37%, respectively), which are represented by hydroxyapatite crystals.
During the development of the follicle, it goes through the following stages:
The relationship between the follicles of molars and the roots of primary teeth is constantly changing.
- At first, they do not reach the roots of the temporary molars, since they have not yet fully formed. During this period, the follicles are rounded, they are surrounded by a layer of cancellous bone substance and a cortical plate.
- Step by step, the follicle moves to the alveolar edge, which occurs against the background of a deficiency of lime in the coronal part. This is clearly visible on x-rays: the roots of baby teeth are completely formed, and the periodontal fissure is visualized throughout its entire length and has clearer contours on the outer surfaces.
- On the inner side, the boundaries of the periodontal fissure are slightly blurred; in the area of bifurcation of the roots, the fissure narrows. The follicles are round and are visualized at the level of the apices of the roots preceding them.
- The neck of the follicle and the root of the permanent tooth begin to form. It lengthens and ends up between the roots of temporary teeth, moving to the border of the alveolar process. The stage is called stabilization , since the resorption of the roots of baby teeth begins.
- As resorption occurs, against the background of follicle growth, the roots and follicles come closer together and remain close to each other for a long time.
- Along with the eruption of a permanent tooth, the resorption of the follicle boundaries is activated and the temporary tooth falls out.
TOOTH CEMENT
The cementum of the tooth covers the root and is divided into primary and secondary. Primary (cell-free) cement is adjacent directly to dentin, covering the lateral surfaces of the tooth root. Secondary (cellular) contains cementocides, covers a layer of primary cement, is localized only in the area of the root apex and on the interroot surfaces of premolars and molars.
The main substance of cement is represented by collagen fibers running in different directions, most of which run in the radial direction. In some pathological conditions, hypercementosis is observed (excessive deposition of layers of cement on the surface of the tooth root). Cement consists of 68% inorganic and 32% organic substances.
Structure
Periodontal cells are divided into:
- fibroblasts;
- osteoblasts;
- cementoblasts;
- osteoclasts;
- macrophages;
- epithelial remains of Malasse.
The intercellular substance is periodontal fibers. They make up the bulk of it. They can be divided into five main groups:
- alveolar;
- oblique;
- apical;
- horizontal;
- interroot.
Interdental fibers are located separately and connect adjacent teeth.
The histology of periodontium is that it consists of cells and intercellular substance.