- Surgical department
Surgical department » - Maxillofacial Surgery
Maxillofacial Surgery "
- Jaw osteotomy
Malocclusion is a violation of the process of chewing food and swallowing it, a negative effect on the speech apparatus, as well as an aesthetic defect. With malocclusions, the upper and lower jaws can be enlarged or reduced in size, pushed forward or positioned posterior to the normal position, shifted to the side or tilted, turning clockwise or counterclockwise. In this case, the closure of the teeth is disrupted to one degree or another, they change the angle of inclination, turn around, run into each other (crowding) or diverge with the formation of cracks (treme).
What are the dangers of malocclusion?
- Violation of dental contacts makes it difficult to chew food and provokes the development of diseases of the gastrointestinal tract.
- Severe malocclusions so limit the possibilities of normal nutrition that they are a reason for deferment from the army.
- Changing the angles of inclination of the teeth affects the distribution of the load during chewing, leads to overload of the periodontium, the development of gum inflammation and, ultimately, earlier tooth loss.
- Teeth crowding, combined with misalignment, affects the natural cleaning of teeth, further leading to the development of gum disease and an increased likelihood of tooth enamel destruction. If tooth loss has already occurred, then violations of the jaw relationships can create difficulties in prosthetics.
- Malocclusion leads to a change in the trajectory of jaw movement during chewing: the temporomandibular joints are overloaded, and dysfunction of the temporomandibular joints develops.
- Some types of malocclusion are anatomical prerequisites for narrowing the airways, for the appearance of snoring and such a serious condition as sleep apnea.
3D planning – full diagnostics as a guarantee of results
To plan how the proportions of the face will change after orthodontic treatment and surgery itself, photography, computed tomography, and the creation of plaster and STL models are carried out. Based on computer processing of diagnostic data, specialists determine the maxillofacial parameters required for the correct functioning of the temporomandibular joint, correct contact between teeth and harmonization of facial features, select the optimal management tactics, manufacture orthodontic structures and plan the course of the operation.
Jaw osteotomy surgery
Historically, the first operations were performed on the lower jaw. And the surgeon’s task was precisely to restore normal jaw relationships. But today operations on the lower jaw alone account for no more than 10% of operations performed. Because the surgeon’s tasks have changed: now it is not only the correction of the bite, but also the improvement of facial aesthetics.
Double-jaw osteotomy is an operation on the lower and upper jaw simultaneously, which allows you to achieve aesthetically favorable proportions of the face both in front and in profile, eliminate asymmetry, and make the smile brighter by eliminating dark corridors - shading of the lateral teeth of the upper jaw. We can say that surgery on one jaw is only a correction of functionality, on two – functionality and aesthetics.
Indications for the operation:
- violation of the closure of the dentition, which cannot be corrected orthodontically;
- pronounced facial disproportions that have aesthetic significance.
Contraindications:
- unpreparedness of the dentition for surgery (insufficient orthopedic or orthodontic preparation);
- diseases of internal organs that prevent surgery or anesthesia.
Modern modification of osteotomy technique
Deficiency of bone tissue height in the posterior areas of the upper jaw occurs quite often in the clinical practice of a dentist, making it difficult to perform a dental implantation procedure. The combined trephine-osteotomy method was developed specifically to optimize the process of restoring the vertical parameters of the residual ridge, while minimizing the invasiveness and traumatic nature of the manipulation compared to the classical approach of forming a lateral window during sinus lift. The authors of this article propose a new modification of iatrogenic intervention, which will make the surgical procedure more effective by creating adequate conditions for the installation of sufficiently long dental implants.
The clinical cases presented below describe in detail the modified sinus lift algorithm, which increases the overall effectiveness of rehabilitation of patients with bone deficiency in the posterior areas of the upper jaw.
Approaches to augmentation of the maxillary sinus floor
The success of dental implantation is determined by a number of factors, including the quantity and quality of bone tissue, the distribution of occlusal loads, and the characteristics of the anatomical structure of the jaws. After the extraction procedure, in the first six months, the processes of bone tissue resorption begin to progress, the vertical and horizontal parameters of the residual ridge are significantly reduced, thereby limiting the possibilities for adequate installation of titanium infrastructures.
According to Lil, it is the deficiency of bone crest height that is the main reason for the lack of implant success in the posterior maxilla, while several previous studies have pointed to the dominant role of bone type 4 as the main unfavorable condition for predicting long-term rehabilitation prognosis.
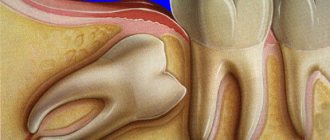
The lack of functional load due to the loss of teeth provokes bone resorption in the area of the bottom of the maxillary sinus, due to which the parameters of pneumatization of the sinus increase significantly. Thus, to install implants in such cases, it is first necessary to reconstruct the alveolar ridge in the area of the floor of the maxillary sinus (often through a lateral approach), and only then can subsequent implantation proceed.
Fugazzotto, in turn, developed an alternative approach to performing a sinus lift, combining the principles of trepanation and osteotomy. If the height of the residual ridge in the posterior part of the upper jaw is 4-5 mm, then in order to reduce the parameters of trauma during the manipulation, only a trephine is used. In addition, this technique eliminates the need for autogenous bone and also reduces the risk of perforation of the Schneiderian membrane with a 2-mm twist drill, the use of which is not included in this approach. Fugazzotto proved that the iatrogenic intervention algorithm he proposed ensures 100% efficiency of manipulation, compared to the implementation of a surgical procedure according to the classical protocol through the lateral window, which is 97.3% effective. This technique is also advisable to use to prepare multiple implantation sites when implementing a standard protocol is not possible.
Bone sites in the maxillary molar region show a 96-97.8% implantation success rate over a three-year period, but Kolerman et al demonstrated a 100% success rate for intraosseous screw placement using a modified approach, thereby proving its effectiveness and clinical feasibility. At the same time, the adapted algorithm for performing osteotomy is suitable both for the preparation of a single site and for the simultaneous installation of several implants. Fugazzotto previously developed a technique for the immediate installation of implants 8.5 mm long in the area of the bottom of the maxillary sinus, but when implementing the technique proposed by the authors of the article, the possible length of the screws can be increased, since it has been proven that intraosseous elements of 10 millimeters or more ensure 93.4% of implantation success , while 8 mm - only 88.9%, of course, under the same conditions for performing a sinus lift.
Surgical technique
To preoperatively assess the height of the residual ridge, appropriate measurements are taken on the radiographic image. Then a palatal incision is made in the edentulous area; if the procedure is performed immediately after extraction of the upper molars, then the incision is made in the area of their palatal root. This helps in the future to adapt the coating membrane as efficiently as possible.
On the buccal side, releasing vertical incisions are made, after which full-tissue flaps are separated with additional separation of periosteal tissues to improve tissue mobilization parameters.
A calibrated trephine drill is used to create a kind of socket, which is often formed through the bone of the interradicular septum. The created socket should be at least 2 mm less than the bucco-palatal width of the ridge, providing a remaining 1 mm of bone tissue on each side. The upper limit of the osteotomy at this stage should not reach the bottom of the maxillary sinus by at least 1 mm. To achieve good contact with the alveolar ridge, the trephine is first used in reverse mode to collect bone, and then in normal mode: actually, for cutting the bed. The maximum osteotomy speed is 1200 rpm. After completion of the osteotomy, there should be some gap between the lateral walls and the formed socket, while in the apical part there should be contact with the bottom of the maxillary sinus.
Next, a calibrated osteotome corresponding to the diameter of the trephine is used. With a slight movement of the hand and without excessive pressure, the previously prepared bed is deepened by approximately 1 mm. If the results of CBCT revealed a thick Schneiderian membrane, the depth of the osteotomy can be even slightly increased using a chisel, observing maximum care when performing such a manipulation.
After achieving the required vertical parameters in the problem area of future implantation, the bed is packed with allograft material and covered with a resorbable membrane. If it is impossible to achieve primary closure, a dense polytetrafluoroethylene membrane can be installed instead of a resorbable one. Once the membrane has been stabilized, the mucoperiosteal flaps are positioned and the intervention area is sutured to achieve wound healing by primary intention. Regarding membrane stability: we have found that in small areas it can be achieved through the adhesion of a fibrin clot, and in case of long defects, fixing screws can additionally be used. The wound healing period ranges from 3 to 6 months.
During repeated intervention, the installation of implants is carried out either in parallel with the internal sinus lift, or through the usual algorithm for preparing the implantation bed. To achieve adequate primary stability parameters, it is recommended to use a conical implant design, especially in thin areas of bone, or with type 4 bone density.
The following clinical cases describe practical examples of the use of the proposed modified technique for osteotomy of implant sites.
Clinical case 1
A 62-year-old man with a medical history presented to the Graduate Department of Periodontology at Rutgers University in Newark, New Jersey, for restoration of an edentulous area on the left side of the mandible. During clinical and radiological diagnostics (photo 1), it was found that the prognosis of the 12th tooth was unfavorable, and the maxillary sinus in the area of 14 was excessively pneumatized.
Photo 1. Clinical case 1: radiograph before intervention.
Due to the inadequate anatomy of the roots of the 15th tooth, the use of conventional fixed structures was contraindicated; therefore, the option of prosthetics based on dental implants installed in the area of the 12th and 14th teeth remained. The implementation of the immediate implantation procedure was not possible due to the presence of a periapical lesion in the area of the 12th tooth. Preparation of the implantation site using a modified bed formation technique has been proposed as most suitable in the area of the 14th tooth. After local anesthesia (2% lidocaine, 1:100,000 epinephrine), palatal crestal and intrasulcular incisions were made, after which the complete mucoperiosteal flap was separated in the buccal direction. A trephine drill 2 mm smaller than the buccopalatal width of the molar socket was used to form the socket, after which the apical border of the socket was moved slightly apically using an osteotome of similar diameter (Figure 2).
Photo 2. View after separation of the full flap: sufficient bone width allows the formation of an adequate bed, which is subsequently filled with allograft material, on top of which a membrane is subsequently installed.
The surgical site was filled with mineralized cortical allograft and covered with a resorbable membrane, after which it was carefully sutured with 4.0 Vicryl sutures (Johnson & Johnson) without excessive tension on the sutures. The extraction of the 12th tooth was carried out during the same visit, after which a thorough revision of the socket was provided and it was filled with a bone substitute to optimize the process of bone tissue formation. Radiographs were taken immediately after the surgical procedure (Figure 3) and 4 months after the initial procedure. After some time, two conical implants (4 & 5 mm x 11.5 mm) (photo 4), made of commercially pure titanium with a rough surface (Biomet 3i), were installed in the area of the first premolar and molar of the upper jaw.
Photo 3. X-ray after performing a sinus lift in the area of the 14th tooth.
Photo 4. View of the intervention area after 4 months, installation of two 11.5 mm implants.
In the postoperative period, the patient was prescribed amoxicillin 500 mg three times a day for 7 days after surgery, as well as ibuprofen 600 mg as needed. To maintain an adequate level of oral hygiene, it was also recommended to use 0.12% chlorhexidine gluconate solution (Peridex, 3M ESPE) as a rinse twice a day for 10 days, as well as avoid hard foods and brush teeth gently for subsequent periods. 2 weeks. The sutures were removed 14 days after surgery, and no complications were observed in the postoperative period. During the first month, the patient was re-examined every two weeks, and in the next two months - once every 30 days. Four months after implantation, a three-unit metal-ceramic screw prosthesis was placed, which demonstrated excellent clinical and radiological stability one year after fixation (Figure 5).
Photo 5. Fixation of a prosthetic element of 3 units.
A schematic representation of the stages of surgical technique is shown in photos 13-18.
Photo 13. Determination of the vertical parameters of the residual ridge on a radiograph using a template.
Photo 14. Preparation of the bed using a trephine at a speed of 1200 rpm, not reaching 1 mm to the Schneiderian membrane.
Photo 15. Remnants of bone remain in the area of the implantation bed. If the sinus floor is uneven, piezosurgical attachments can be used to optimize the procedure.
Photo 16. Disposition of the bone crust for raising the Schneiderian membrane using an osteom (the diameter of the latter corresponds to the diameter of the previously used trephine).
Photo 17. To optimize the apical displacement of the sinus floor, crushed bone is additionally used.
Photo 18. Depending on the achieved ridge height, the procedure is either modified or implants are installed according to the usual protocol.
Clinical case 2
A 58-year-old healthy man presented to the Graduate Department of Periodontology at Rutgers University in Newark, New Jersey for restoration of a right maxillary molar (Figure 6).
Photo 6. Clinical case 2: radiograph of the 3rd tooth.
Clinical and radiographic examinations helped to detect a recurrent area of carious lesions under the existing prosthesis; therefore, the prognosis of the tooth in terms of therapeutic treatment was unfavorable. To preserve the integrity of the dentition, it was proposed to carry out an implantation procedure followed by orthopedic rehabilitation. After performing local anesthesia with a 2% lidocaine solution with an epinephrine concentration of 1:100,000, the molar was segmented and removed in a minimally traumatic manner. After extraction, an area of buccal digestion was discovered, although the integrity and volume of the interradicular bone tissue remained quite acceptable. To assess the extent of the defect, vertical releasing incisions were made on the buccal side of the jaw. A trephine drill was used to form the socket, and an osteotome of the same diameter was used to deepen it without damaging the sinus (photo 7).
Photo 7. After molar removal, the implantation bed was prepared through the interradicular bone tissue.
The prepared bed was filled with mineralized cortical allograft and covered with a resorbable membrane in such a way as to also isolate the area of the buccal defect. The flap was positioned and the surgical site was sutured using 4.0 Vicryl sutures to achieve primary wound closure without excessive tension. Radiographs were taken immediately after the surgical procedure (Figure 8).
Photo 8. X-ray after iatrogenic intervention.
In the postoperative period, the patient was prescribed amoxicillin 500 mg three times a day for 7 days after surgery, as well as ibuprofen 600 mg as needed. To maintain an adequate level of oral hygiene, it was also recommended to use 0.12% chlorhexidine gluconate solution (Peridex, 3M ESPE) as a rinse twice a day for 10 days, as well as avoid hard foods and brush teeth gently for subsequent periods. 2 weeks. The sutures were removed 14 days after surgery, and no complications were observed in the postoperative period. During the first month, the patient was re-examined every two weeks, and in the next two months - once every 30 days. No complications from the maxillary sinus were recorded. Four months after the initial intervention, a conical dental implant 5 mm x 11.5 mm was installed (photo 9), onto which a screw metal-ceramic crown was fixed six months later. One year after installation of the superstructure, the implant remained clinically and radiologically stable (Figure 10).
Photo 9. Installation of a dental implant.
Photo 10. View of the final restoration 1 year after surgical manipulation.
Discussion
A sinus lift is inherently an iatrogenic intervention aimed at restoring the vertical parameters of the residual ridge in the distal areas of the upper jaw. And although the classic approach through the formation of a lateral window is quite effective, there are also some disadvantages of this method: it is more invasive, and the technique of its implementation depends on the presence of teeth in the problem area. There are also risks associated with the possibility of perforation of the mucosa at the bottom of the maxillary sinus, and, even despite the professional skills of the doctor, the percentage of postoperative complications remains quite high. Therefore, the development of a less invasive technique for performing this procedure is highly advisable. The technique of forming a kind of nest using a trephine and osteom is not only less traumatic, but also safer, which is ensured by the replanting of an autogenous component in the area of the bottom of the maxillary sinus. In principle, the procedure is technically simple to perform and helps save the overall working time of the dental surgeon. In addition, the proposed modification of the surgical approach can be used when implanting single areas, in the area of periodontologically compromised molars, when the presence of lateral teeth complicates the standard procedure through the lateral window, and immediately after the removal of problem teeth, as well as when preparing an implantation bed for several titanium teeth at once intraosseous units.
Anatomical limitations associated with an uneven floor of the maxillary sinus or a thick Schneiderian membrane can be successfully circumvented by combining the proposed reconstruction algorithm with a piezosurgical approach (photos 11 - 12). In addition, unlike the traditional Summers technique, our innovative approach allows for the preparation of several implant sites at once during one clinical visit, minimizing invasiveness and duration of manipulation.
Photo 11. Combination of a modified technique with piezosurgery for apical reposition of the bottom of the implantation bed.
Photo 12. View of the implantation bed for installing several implants after implementing a modified approach together with piezosurgery.
conclusions
The technique of forming an implantation bed through trephine-osteotomy preparation of the jaw area has previously been described in the literature as one that helps optimize the process of immediate implantation in the distal areas of the upper jaw.
Fugazzotto’s publications describe how, using a similar technique, it is effectively possible to place 8.5 mm implants in the area of the bottom of the maxillary sinus, but today the modification of the method has reached the point that it can be used to install implants even longer than 8.5 mm without fear postoperative complications.
In addition, the use of longer intraosseous elements has been shown to increase the overall success rate of the rehabilitation procedure for edentulous patients, both in the restoration of single and longer defects.
In conclusion, it can be summarized that the proposed approach not only saves overall treatment time and is less invasive, but also helps to more optimally achieve the proper conditions for the placement of long implants in the posterior areas of the maxilla.
Authors: Anna M. Brunetti, DMD, MDS Howard Drew, DMD Andrew Sullivan, DDS Joel Pascuzzi, DMD Emil Cappetta, DMD
Stages of treatment
Today, the method of combined treatment of malocclusions, when the orthodontist begins work first, is considered generally accepted in the world.
1) Orthodontic stage
The orthodontist places braces on both jaws and begins to move the teeth so that they take the correct position in relation to the jaws. In this case, a temporary deterioration in the closure of teeth occurs. It takes about nine months to prepare. After this, the surgical stage is performed.
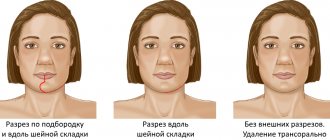
2) Surgical stage
The operation is performed under general anesthesia. The intervention is performed via intraoral access, which allows it to avoid leaving scars. In accordance with the treatment plan, cuts are made on the upper and lower jaws, the fragments are mobilized and installed in the most functionally and aesthetically advantageous position. Next, the jaws are fixed with titanium miniplates, which are invisible to the body, do not ring at the airport and do not interfere with MRI. They usually remain in the body for life without causing any consequences. In rare cases, surgery may be performed before orthodontic treatment begins.
Rehabilitation after osteotomy
Let's consider the recovery period after surgery using the example of corrective osteotomy.
The patient is in the hospital under the supervision of doctors for 3 to 7 days. At this time, regular treatment of the surgical wound is carried out, painkillers, antibiotics and anti-thromboembolism drugs are given. It is important to start getting up as early as possible and not to lie around.
After discharge, the patient must continue taking the prescribed medications at home. On the 10-14th day, the sutures are removed. Next, rehabilitation is indicated - the use of crutches for up to 6-12 weeks, regular visits to the doctor for examinations. Heavy physical activity will be allowed only 6-8 months after the operation. Sometimes installed metal structures are removed after 1-2 years.
Potential complications of orthognathic surgery
Detailed computer planning of the intervention and long-term preparation help to almost completely minimize the risk of complications.
After surgery, patients often note temporary numbness of the lips, which, however, has a rather positive effect, since it allows one to avoid pain. Otherwise, any operation carries possible risks, the avoidance of which depends on the professionalism of maxillofacial surgeons and the competent work of orthodontists. Therefore, choose only proven options!
3D planning of orthognathic surgery
Before
Photo of a face
Photo of a face
Performing an optical scan of the dentition. Optical model of dentition
Performing an optical scan of the dentition. Optical model of dentition
Orientation of the head in space according to the skin
Combining jaw scans with computed tomography
Orientation of the skull in space
3D cephalometric analysis
Stages |
Jaw osteotomies
Moving the Jaws and Creating a Template
Template for operation
When is orthognathic surgery not indicated?
The bite can be changed surgically only when the jaw bones are fully mature - that is, only in adults.
Contraindications to surgery are life-threatening conditions or chronic diseases in the stage of decompensation: cardiovascular, endocrine (diabetes mellitus), oncological (especially tumors in the facial area), as well as disorders in the blood coagulation system, some mental illnesses.
Often patients come to us who have a correct bite and harmonious features, but still require surgery and improvement of existing data. Orthognathic surgery, which has truly transformative properties, works, however, only in the presence of real, and not fictitious, problems, and still has limited capabilities, in some ways superior, but also in some ways inferior to plastic surgery.
Installation
Installation of plates for a jaw fracture using the open method is carried out in 4 stages:
- a soft tissue incision is made to visualize and connect the fragments;
- connecting bone fragments using a plate;
- fixation of bone elements with glue, staples, quick-hardening plastics used in modern surgery;
- suturing.
The main difficulty of open surgery is trauma. The doctor works with the area in which the nerve endings and salivary glands are located, which creates the risk of damage to them, and therefore determines high requirements for the qualifications of the specialist.
A safer and less traumatic method is ultrasonic osteosynthesis of the jaw. It not only reduces the risk of complications during fixation, but also reduces the time for fracture healing.
Plates for jaw fracture
The use of plates after a jaw fracture is justified when a conservative treatment method either does not give the desired result (correct reposition and high-quality fusion of bone parts) or cannot be used initially (complex injury). The decision to perform an operation is made by the doctor after examining the patient (examination if treatment methods other than surgery have already been used).
The advantage of bone osteosynthesis is that when plates are installed to connect fragments, the lesion site is well supplied with blood. This ensures fairly rapid fusion - in just a few weeks - while restoring the bone itself (integrity) and its anatomically correct structure.