Author of the article:
Soldatova Lyudmila Nikolaevna
Candidate of Medical Sciences, Professor of the Department of Clinical Dentistry of the St. Petersburg Medical and Social Institute, Chief Physician of the Alfa-Dent Dental Clinic, St. Petersburg
Periodontium is connective tissue located in the gap-like space between the cementum of the tooth root and the alveolar plate. Its inflammation (periodontitis) is one of the most severe and dangerous dental diseases. It often occurs as a result of deep caries of one or more teeth - in this case, the infection most often penetrates the connective tissue through holes in the roots. Other routes of infection are also possible - for example, through the blood in the presence of other inflammatory processes in the body, through gum tissue in case of periodontitis, etc. In addition, periodontitis can occur as a result of a reaction to the effects of certain medications during previous dental treatment. Dental injuries can also serve as a starting point for the development of an inflammatory response.
The periodontium contains a large number of blood vessels and nerve endings, and also performs the most important functions, creating support for the teeth and serving as a shock absorber during chewing. Therefore, its inflammation in most cases is accompanied not only by severe pain, but also by the danger of losing teeth. Periodontitis can become chronic with periodic exacerbations. The symptoms and treatment tactics of periodontitis largely depend on the form of the disease:
- Acute periodontitis
Obviously expressed inflammatory symptoms: swelling and redness of the gums, acute pain, swelling of the tissues in the area of the affected tooth. Occurs for the first time. As a rule, the acute form is not accompanied by destruction of bone tissue in the upper part of the root. - Chronic
May be asymptomatic or with minor manifestations - periodically occurring mild aching pain, soreness of the teeth or gums when biting. When favorable conditions for microorganisms arise, an exacerbation occurs, during which the symptoms become more pronounced. Also, in the chronic course of periodontitis, an x-ray usually reveals the presence of an abscess (accumulation of pus) in the area of the root apex. In the photographs, the abscess looks like a small clearing. A long course of the disease can also lead to the destruction of bone tissue in close proximity to the source of the inflammatory process.
Indications for treatment of periodontitis
There are two main ways to treat periodontitis: conservative and surgical. Each of them has its own indications and contraindications.
According to modern dental standards, a doctor should give preference to conservative methods. They are indicated for both acute and chronic periodontitis, including the appearance of cysts and granulomas, loose teeth, and increasing inflammation.
However, orthograde treatment cannot be used in all cases. Indications for surgical intervention are:
- obstruction of the tooth root canals;
- the presence of a stump tab or pin that cannot be removed without damaging the roots;
- multiple perihilar cysts or cysts growing into the maxillary sinus;
- wide affected area (over 10 millimeters);
- perforation of the tooth cavity or root wall;
- ineffectiveness of conservative treatment methods.
Important!
When we talk about periodontitis, we often mean apical (also known as periapical or apical) periodontitis - that is, inflammation at the apex of the tooth root. The cause of this disease is endodontic problems. Another type of periodontitis, marginal, affects the gums in the cervical area of the tooth, but it already belongs to the field of periodontology. This material is devoted to the treatment of apical periodontitis only.
Answers to popular questions
How long can it take to treat periodontitis?
Treatment of inflammation of periodontal tissues is a very long process. On average, 3–5 visits to the dentist may be needed (depending on the clinical case). The entire process sometimes takes several months.
Why is periodontitis dangerous?
The danger of the disease lies in its consequences. If inflammation is not treated, the following may develop: 1. periapical abscess; 2. diffuse purulent inflammation of the subcutaneous tissue (phlegmon); 3. fistula in the gum; 4. destruction of the jaw bones (osteomyelitis); 5. blood poisoning; 6. unit falling out of the hole, etc.
How can I tell if I have chronic periodontitis?
The following alarming signs may indicate the chronicity of the process: • wave-like appearance of aching pain; • the appearance of a fistula opening on the gum with purulent discharge; • increasing the sensitivity of the segment when chewing. At the first suspicion of the presence of a pathology, consult a doctor and undergo diagnostics.
Treatment methods for dental periodontitis
| Conservative treatment | Surgery |
Therapeutic:
Physiotherapeutic:
Conservative treatment of periodontitis is accompanied by the use of antibiotics. | Surgical treatment:
|
Important!
The probability of successful conservative treatment of periodontitis is 70 - 90%
Why does periodontitis occur?
The most common causes of periodontitis are the following:
- caries in an advanced stage, which was not subjected to timely treatment;
- pulpitis in an advanced stage, lack of modern treatment;
- falls or blows to the jaw;
- poor-quality root canal treatment in the past;
- an inflammatory process that develops under the crown.
At risk of periodontitis is any patient who does not seek help from the clinic in time for caries. The problem often “pops up” in patients who do not attach importance to pain, and ordinary caries over time transforms into a more global pathology of the periodontium and canals.
Stages of periodontitis treatment
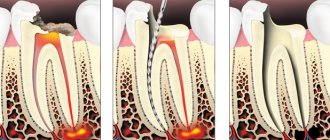
The number of visits to the clinic for the treatment of periodontitis depends on the stage of the disease (acute periodontitis, chronic, chronic in the acute stage) and the chosen technique. Often, therapy is carried out in several stages and requires at least 2 - 3 visits to the attending physician, since it is not recommended to install a permanent filling until the inflammation is completely removed.
- Preparation for treatment: diagnosis using an x-ray, anesthesia injection.
- Drilling a tooth to access canals, removing a nerve, or removing an old filling.
- If necessary, expand channels.
- Antiseptic treatment of canals, application of medications, physiotherapeutic procedures.
- Installation of a temporary filling.
- Removal of the temporary filling, antiseptic treatment of the canals (this stage is repeated until the source of inflammation is completely eliminated; sometimes this may take several months).
- Installation of a permanent filling, control x-ray.
In parallel, the patient is prescribed antibacterial and anti-inflammatory therapy, as well as home rinses with disinfectant solutions.
Treatment quality criterion
High-quality, effective treatment of periodontitis requires pinpoint precision when working in tooth canals that have a complex shape and individual anatomical features. Obturation (sealing) of canals is based on the principle of “three pillars”: the canal must be sealed to its entire length, along all micro-branches, without pores and air cavities. This requires high qualifications and extensive experience of the attending physician, as well as the use of modern equipment - endomotors, apex locators, files, dental microscope. Modern endodontic treatment is a high-tech medical procedure and is based on new medical, technological and ergonomic principles, which obliges clinics to be equipped with modern equipment, and doctors to regularly improve their level of professional competence.
Features of the treatment of periodontitis with fistula
Odontogenic fistula is one of the complications of periodontitis, mainly granulating. It consists of holes in the mucous membrane, which are formed due to the proliferation of granulations and destruction of the tissues surrounding the tooth. In severe cases, a fistula can appear not only in the gum, but also in the cheek, and even on the skin of the face. Purulent contents are released through the hole, which appears due to the inflammatory process in the periodontium.
On the one hand, the formation of a fistula facilitates the course of the disease, since inflammatory products are eliminated through it (which means that the patient most likely will not suffer from severe pain). On the other hand, non-intervention over time can lead to tooth loss.
You can get rid of a fistula only by eliminating its cause - damage to periodontal tissue. Treatment follows a standard scheme: mechanical treatment of the canals, disinfection and thorough filling. Due to the outflow of pus through the fistulous tract, treatment is most often successful and takes less time. After creating suitable conditions, the fistula goes away on its own, but in severe cases, surgical removal of overgrown granulations may be necessary.
Periodontitis: definition, etiology, symptoms
Periodontitis is a disease characterized by inflammation of the complex of tissues surrounding the tooth and holding it in the socket. Based on etiology, there are several types of periodontitis. Infectious periodontitis is the most common (90% of all cases) and occurs due to the irritating effect on the periodontium of the infectious-toxic contents of the root canals. As a rule, the cause of this is caries or pulpitis, in some cases – poor-quality root canal treatment. The process of disease development begins with the entry of microbes into the tooth canal, where they undergo natural selection in the harshest conditions of a closed anaerobic space. The strongest bacteria, surviving, form a special class, which is collectively called “odontogenic microflora”. It differs from the dental microflora of the oral cavity in its unique vitality and extremely aggressive effect of its metabolic products on surrounding tissues. Gradually, in the apical and apicolateral zones or, less commonly, in the bifurcation zone, the process of destruction of bone tissue begins. If there are epithelial elements in the above areas, they become involved in the odontogenic inflammatory focus and begin to grow, forming a granuloma. Next, the granuloma develops and enters the so-called transitional stage - cyst-granuloma and then “grows” into a cyst. Depending on a number of factors, such as the activity of pathogenic microflora, the strength of the immune system, characteristics of the chewing load, the frequency of stressful conditions, living conditions and others, an odontogenic cyst can be a source of constant discomfort or not bother the patient at all. An “asymptomatic” cyst can grow to enormous sizes, causing many dental pathologies and even jaw deformation due to the involvement of a large number of teeth in the growth process. It is extremely rare that the infection enters the periodontium through the blood or lymph flow. In such cases, the disease is called retrograde periodontitis. Traumatic periodontitis is the result of an injury - domestic or sports, when the patient receives a severe bruise, or iatrogenic, that is, caused by the actions of a doctor (for example, an accidental endodontic injury, a piece of an endodontic instrument left in the canal, a filling with the filling material extending beyond the apex of the root, an over-inflated filling or crown, causing permanent microtrauma). With acute trauma, acute periodontitis develops, characterized by visible injury to soft tissues, hemorrhage, and the appearance of tooth mobility. With chronic trauma, changes in the periodontium occur gradually. Drug-induced or toxic periodontitis is most often a complication of the treatment of pulpitis, when drugs containing arsenic, sodium hydrochloride, resorcinol-formalin mixtures, aseptic solutions, and some filling materials cause irritation, necrotization and inflammation of the periodontium. In some cases, toxic periodontitis may be caused not by drugs, but by decay products of the pulp, which has undergone necrotic damage due to poor-quality filling during caries. Symptoms of periodontitis may vary depending on the stage of the disease and the location of the inflammation. Thus, a pulsating, constantly increasing localized pain occurs when biting, closing teeth, and even when touching them. Eating food and fluids often becomes difficult and may sometimes be accompanied by a fever. Patients often note that the tooth feels like it has “grown” and there is a feeling of fullness. Symptoms also include swelling of the gums, gumboil, and fistula. At the same time, periodontitis at its various stages may be asymptomatic or accompanied by some discomfort in the area of the diseased tooth. Types of periodontitis according to the clinical picture of the disease Periodontitis is a complex, serious disease that medical science has carefully studied for several decades. In the process of searching for effective methods of its treatment, various species classifications were developed, which made it possible to recognize and treat periodontitis in its most diverse manifestations. Today, the most authoritative is the International Classification of Diseases ICD-10, adopted by WHO, where periodontitis is located in section K04 - diseases of the pulp and periapical tissues. But, according to dentists, a more detailed description of all stages of periodontitis is presented in the International Classification of Dental Diseases ICD-C-3 based on ICD-10, but which has some differences with the accepted Classification. Thus, according to these classifications, several types of periodontitis are distinguished: K04.4 Acute apical periodontitis of pulpal origin Acute apical periodontitis NOS*. This is a “classic” type of disease with a clearly defined etiology and clinical symptoms: swelling, tissue infiltration, inflammation, which can be serous - this stage lasts 1-2 days, is characterized by constant pain, especially with pressure on the tooth; serous-purulent - duration about 2 weeks, swelling of soft tissues, hyperemic mucosa, tooth mobility is observed; purulent-necrotic with the formation of an abscess. K04.5 Chronic apical periodontitis (Apical or periapical granuloma. Apical periodontitis NOS* .
This stage of the disease is the outcome of the acute stage and means that the source of infection has been present for a long time - from several weeks to several months. At this stage, the patient feels almost no pain. In the tooth cavity in the area of the root apex, granulation tissue growth is observed. Under favorable conditions, this tissue encapsulates, forming a granuloma, which can be sterile or infected. It is not connected to the alveolus, but with its fibers passes directly into the periodontium, causing excessive formation of cement at the root apex or, on the contrary, promoting bone resorption. Hardening of the formation and disappearance of the source of inflammation is considered a favorable outcome, which becomes possible as a result of high-quality treatment and filling of the canals. An unfavorable outcome in the absence of treatment is a complication in the form of subcutaneous odontogenic granuloma.
K04.6 Periapical abscess with cavity Tooth (dental) abscess with cavity. Dentoalveolar abscess with cavity. Previously, this code corresponded to Periapical abscess with fistula , which was divided into:
K04.60 Fistula communicating with the maxillary sinus.
K04.61 Fistula communicating with the nasal cavity.
K04.62 Fistula communicating with the oral cavity.
K04.63 Fistula communicating with the skin.
K04.69 Periapical abscess with fistula, unspecified. This stage of periodontitis is characterized by the absence of pain, as there is an outflow of infectious-toxic contents (exudate) from the periodontal area into the root canal of the tooth, and then into the oral cavity. Another option may be the penetration of purulent contents through the fistula into the oral cavity, maxillary sinus, nasal cavity, and skin. Granulation tissue grows, fills the fistula tract 4. K04.7 Periapical abscess without cavity Dental abscess NOS. Dentoalveolar abscess NOS. Periapical abscess NOS. This code in ICD-C-3 corresponds to Periapical abscess without fistula , which was characterized by the fact that the absence of a fistula increased the amount of exudative content in the periodontal area, which caused severe pain, increased swelling and ultimately the formation of an abscess 5. K04.9 Other and unspecified diseases of the pulp and periapical tissues 6.
Treatment of chronic forms of periodontitis
There are three types of chronic periodontitis: fibrous, granulating and granulomatous.
- In fibrous periodontitis, the tissues surrounding the apex of the tooth are replaced by fibrous tissue. The patient usually does not feel pain, and the disease can only be determined by an x-ray.
- Granulating periodontitis is characterized by the growth of granulation tissue: the process of bone resorption (resorption) starts, fistulous tracts are formed, through which inflammatory products are separated. As the granulations expand, the patient begins to experience periodic aching pain.
- Granulomatous periodontitis is accompanied by the appearance of a granuloma - a neoplasm at the root apex. It is a chamber of connective tissue filled with granulations. If the disease is not treated, the growth of granuloma can even lead to a jaw fracture.
Treatment of chronic periodontitis is often carried out using conservative treatment methods. According to modern standards, doctors, as a rule, do not carry out separate treatment for granulomas, cysts and fistula tracts: if the canals are disinfected and properly sealed, the neoplasms will disappear on their own. In advanced cases, surgical intervention is permissible.
Complications
Periodontitis is dangerous due to rapidly developing serious complications, so it is extremely important to immediately consult a dentist at the first symptoms. The initial form of acute periodontitis very quickly, within a few days, turns into a purulent form, and then into an abscess. At the stage of chronic periodontitis, fistula tracts are formed, which cause suffering to the patient and significantly increase the treatment period.
In addition, we must not forget that periodontitis destroys the bone tissue surrounding the tooth, and is also a chronic odontogenic inflammatory focus, therefore it significantly reduces the patient’s immune status and contributes to the complication of various somatic diseases. In addition, Swedish scientists from Orebro University recently discovered and proved the effect of periodontitis on the cardiovascular system. The reason for this influence is the activity of the bacterium Porphyromonas gingivalis, which is a common pathogen of periodontitis. This bacterium disrupts the functioning of the gene responsible for controlling inflammation in the coronary arteries, contributing to the occurrence of atherosclerosis and heart attacks 8.
Features of the treatment of periodontitis in the acute stage
Exacerbation of periodontitis goes through two phases: intoxication and exudation (appearance of discharge). As the disease progresses, the patient first experiences aching and episodic pain, and then constant throbbing and tearing pain, so treatment cannot be delayed.
Acute periodontitis can be serous or purulent. In the second case, purulent exudate accumulates in the apical part of the tooth root, and the main task for the doctor is to remove it. Sometimes this is enough to clean the tooth cavity and treat the canals, but in severe cases it may be necessary to cut the periosteum for drainage.
Permanent canal filling
Permanent canal filling in the treatment of periodontitis is performed during the third visit to the dental office. Before proceeding with any manipulations, the specialist sends the patient for a control x-ray. The image will help determine the effectiveness of periodontitis treatment. If the percentage of bone tissue destruction has decreased significantly, permanent filling of the canals is performed.
The procedure begins with the removal of the temporary filling from the crown of the tooth, and then the canals are freed from the previously placed composite. The doctor will carry out an antiseptic rinse and then fill them to the apical part of the root with a composite. Upon completion of the work, the patient is given another x-ray to monitor the quality of the filling performed. Gutta-percha must be tightly packed into the canals to the very apex of the root, otherwise there is a high risk of relapse of periodontitis.
A couple of days later, the patient comes to the doctor for the fourth time and during this visit the crown part of the tooth is restored with a permanent filling to restore its aesthetics and functionality.
Treatment of periodontitis at home
Periodontitis cannot be cured at home, since the disease is caused by bacteria that colonize the dental canals. The only way to get rid of them is to carry out antiseptic treatment and sealing of the canals, and this can only be done by a doctor, but by waiting for a visit to the clinic, you can alleviate the symptoms and reduce pain.
Disinfectants that do not irritate the mucous membranes can be used for rinsing 4 - 5 times a day. Doctors also recommend rinsing with a solution of salt and soda, including after treatment, to relieve swelling and reduce inflammation. Non-steroidal anti-inflammatory drugs are suitable for pain relief. All this will help relieve symptoms, but is not a cure.
You may experience pain after periodontitis treatment. Normally, they last 3–5 days and gradually fade away. If the pain does not subside or returns with renewed vigor, re-therapy is necessary.
Temporary and permanent root canal filling
After the operation to remove pus for acute periodontitis, 3-4 days should pass, and then the patient visits the clinic again. During the second appointment, the doctor performs the following manipulations:
1. Thoroughly rinses the canal cavities with antibacterial solutions, and then puts an antiseptic in them.
2. Places a temporary filling on the tooth.
The patient is sent home, but is warned: at the slightest sign of pain, he should immediately seek professional dental care.
Permanent filling of the canals is carried out during the third visit. The treatment procedure can be carried out in the absence of complaints from the patient about any discomfort, as well as in the complete absence of pus in the canal cavities. The canals are filled with gutta-percha composite to the upper root zone. Restoration of the aesthetics and functionality of the tooth is done on a subsequent visit, and at this point the course of periodontitis treatment is considered complete.