Changing the color of tooth enamel is an alarming signal that cannot be ignored. Dark spots can be associated not only with the consumption of coloring foods and drinks, but also with the development of various pathological processes. If the tooth has turned black at the root, you should contact your dentist as soon as possible. Do not wait for pain and other symptoms to appear, as they indicate extensive damage to hard tissues or inflammation of the dental nerve. It is easier to treat any disease in the early stages, so do not delay visiting a doctor.
Chromogenic components (food, drinks, other products)
The food we eat and other substances we use contain coloring agents (coffee, tea, cola, wine, tobacco, etc.) that can cause yellow, brown or bright orange spots to appear on the skin. teeth In most cases, the discoloration of teeth is generalized, which means that stains tend to form with equal success both on the entire surface of the tooth and in individual areas. If stains appear, it is better to make an appointment with an inexpensive dentist near your place of residence.
Possible reasons
Has the tooth turned black near the root? There may be several reasons for this.
- Tartar. One of the most common problems. It is a hard brown coating. It is formed from food debris and soft plaque, which harden under the influence of saliva. Violation of the rules of oral hygiene is the main cause of the appearance of tartar. Most often it forms around the neck of the tooth. It can also be subgingival - adjacent to the root and covered by the gum.
- Cervical caries. Dark spots at the root of the tooth may turn out to be carious cavities. They appear due to demineralization of enamel and destruction of dentin by pathogenic bacteria. As a rule, dental caries is preceded by tartar. The risk of developing the disease increases with insufficient oral hygiene, decreased immunity, and lack of calcium, phosphorus and vitamin D in the body.
- Dying of the pulp. Blackening of the tooth can also be a consequence of necrosis of the cells of the neurovascular bundle. Pulpitis occurs due to deep caries, burns during tooth treatment before prosthetics, or trauma. Pulp necrosis is manifested by prolonged pain when eating hot food and mechanical impact on the diseased tooth, but is often asymptomatic.
- Fluorosis. Darkening of teeth may be due to excess fluoride entering the body. This microelement is necessary for strong bones and teeth, but if the permissible concentration is exceeded, it leads to the development of fluorosis. This disease provokes destructive changes in the enamel and the formation of dark spots and stripes on the teeth.
Tooth decay
In the early stages of tooth decay, white spots or spots appear on the tooth enamel. The affected areas lose their natural shine and become dull. A thorough examination reveals the presence of damage to the enamel. If the process of tooth decay progresses, the affected area becomes brown or black, it is necessary to diagnose dental treatment. The damage is initially noticeable as a small dark spot or spots that gradually increase in size (over several months to several years) and often lead to actual tooth decay.
What symptoms indicate the appearance of a granuloma on the root of a tooth?
Over a long period of time, granuloma on the root of a tooth can develop asymptomatically, and this makes diagnosing the disease in the early stages of development extremely difficult. However, some signs may be present during the initial phases of granulomatosis.
Among them:
- The appearance of dental hypersensitivity to external irritants: hot/cold, sweet/sour foods;
- Bursting sensations in the gum next to the tooth, on the root of which a granuloma has formed;
- A slight aching pain, most often occurring when biting;
- Change in color of the enamel of a diseased tooth.
If you observe similar signs in yourself, it’s time to contact your dentist to diagnose and begin treatment for granuloma! Our advanced dentistry clinic in Moscow, Firadent, uses modern diagnostic techniques and innovative equipment to help identify complex dental diseases in the early stages and carry out effective treatment!
Chronic apical granuloma of the tooth will sooner or later go into the acute phase of development, in which the disease acquires clear signs:
- Acute pain that intensifies when biting and chewing food;
- Feels as if the tooth has become larger or is growing;
- Swelling of the gums and cheeks.
If you ignore these symptoms and do not consult a doctor to remove the dental granuloma, the intensity of the pain will increase, the swelling of the gums and swelling of the face will increase, purulent discharge may begin from the gums, a severe migraine, general weakness, and high temperature may appear. There is no need to try to endure such symptoms - seek professional dental help immediately!
How to treat tooth root granuloma in dentistry: all modern methods of treatment/removal of granulomas
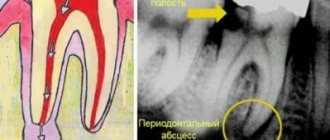
What to do if you notice symptoms of granuloma? Of course, seek help from a dentist, because granulomatosis cannot be treated at home: neither antibiotics nor folk remedies will help. Treatment will begin with diagnostics, during which radiography or radiovisiography is performed. If you have a granuloma, the image will show a darkening at the root of the diseased tooth. Diagnostics will allow you to determine the shape of the granuloma (apical or periapical), assess the stage of development of the tumor, and choose the most effective treatment method for granulomatosis.
Treatment for granuloma can be:
- 1. Conservative (medication).
- 2. Surgical, involving the removal of tooth root granuloma.
We will consider all these methods and their features in detail below.
Black spots on baby teeth
Black spots on baby teeth appear if:
- The mother had some dental diseases while carrying the fetus.
- Lack of water in a child’s body contributes to the development of pathogenic bacteria that cause the appearance of black spots on the enamel.
- Excess iron in the child's body.
- Presence of caries in the initial stage.
IMPORTANT! A child as young as one year old can also have blackened teeth!
Some mothers believe that it is not worth paying special attention to baby teeth, because they will change anyway. This is a misconception, because diseased baby teeth can provoke the appearance of the same disease, only on permanent teeth. Bacteria that existed on primary teeth can migrate to permanent teeth once they begin to erupt.
A diseased tooth is a source of constant infection, which spreads through the circulatory system to the internal organs, so a child with untreated milk teeth often suffers from inflammatory diseases.
Tooth decay, which is one of the main causes of stain formation. Initially, the black color appears at the border of caries cavities, and then spreads to the entire tooth. Often spots appear on the site of old fillings.
Treatment of dental granuloma –
Treatment for dental granuloma is usually only therapeutic. Treatment consists of mechanical treatment of the root canals, in most cases - temporary filling of the root canals with special medicinal pastes based on calcium hydroxide, after which after 2-3 weeks it will be possible to permanently fill the root canals with gutta-percha, as well as put a permanent filling. Below we will talk in more detail about how exactly this treatment is carried out.
Surgical treatment of tooth root granuloma may be required only in a few cases. For example, the operation of resection of the root apex may be indicated - 1) if the root canals are obstructed, 2) if it is impossible to unseal previously poorly filled root canals in order to treat the source of inflammation at the root apex, 3) if there is an artificial crown on the tooth, 4) if in A pin is installed in the root canal, an attempt to remove it may lead to a fracture of the tooth root.
Therapeutic treatment strategy –
- If the root canals have not been previously filled, it is necessary to drill out all carious tissues and old fillings, after which mechanical treatment of the root canals is carried out. After their expansion and antiseptic treatment, the strategy for further treatment may depend on the size of the granuloma.
If the tooth granuloma is small in size (up to 2-3 mm), then the root canal of such a tooth can, in principle, be filled immediately. If the size of the granuloma is from 3 to 5 mm, then a special therapeutic material based on calcium hydroxide is left in the root canals, which will allow the granuloma to shrink or even disappear completely.Temporary canal filling is carried out for a short period of time (on average 2-3 weeks). After this period, a control X-ray is taken, and if the granuloma has disappeared or decreased, the root canals are filled on a permanent basis, and a permanent filling is placed on the tooth. Algorithm for the therapeutic treatment of granulomas more than 3 mm in diameter, cystogranulomas and cysts (detailed descriptions appear when opening the photo) –
- If the root canals in this tooth are sealed (Fig. 7-11) - in this case, the root canals must first be unsealed, and then the treatment sequence corresponds to the previous option.
If such a tooth has an artificial crown, then usually they are first removed and the tooth is treated. And it must be said that in this case the crown will have to be made again. If you do not want to spend money on replacing the crown and filling the root canals, then in principle it is possible to do without it. A surgical root resection operation will help you with this, which means that through a small incision in the gum, the apex of the root with the unfilled part of the root canal and with a granuloma attached to the apex of the root will be cut off from the root.
Emergency care for purulent inflammation -
If you have a dental granuloma, then an exacerbation of the chronic process can lead to the development of purulent inflammation.
If the pus is localized inside the granuloma, then relief from acute pain is possible only after opening the tooth and unsealing the root canals, which will allow the pus to be released through them. How the outflow of pus occurs through the root canals - see video 1 below. But if there is significant swelling of the gums or cheeks, which indicates the release of pus under the periosteum or mucous membrane of the oral cavity, an incision will be required to release the pus. How to make a gum incision - see video 2.
Important: in some cases, a tooth with granulomas may need to be removed (for example, when the tooth crown is severely damaged and cannot be restored). In this case, it is very important that when removing a tooth, the dental surgeon must remove the granuloma from the tooth socket. We have already said above that in most cases they are tightly attached to the apex of the root, and therefore come out along with the tooth. However, in some cases, the granuloma remains in the socket, and then inflammation of the socket of the extracted tooth occurs (alveolitis).
What does a granuloma look like when scraped out of a socket after tooth extraction?
Treatment of dental granuloma with antibiotics -
It is impossible to treat dental granuloma with antibiotics. They can be prescribed only in case of exacerbation of the process (if purulent inflammation occurs) - in parallel with dental treatment carried out by the dentist. The fact is that it is impossible to sanitize infected root canals by simply taking antibiotics, which means the source of infection and inflammation will not disappear. By taking antibiotics, you can only achieve a temporary subsidence of the inflammatory process, but the granuloma itself will not even decrease in size. We hope that our article was useful to you!
Sources:
1. Dental education of the author of the article, 2. Based on personal experience as a dentist, 3. National Library of Medicine (USA), 4. “Therapeutic dentistry: Textbook” (Borovsky E.), 5. “Practical therapeutic dentistry” ( Nikolaev A.).
What to do if large or small spots appear on your teeth?
Any changes in the color or structure of tooth enamel are a reason to be wary and seek advice from a dentist. Only a doctor, after diagnosis, will be able to accurately answer the question: is a blackhead a symptom of caries? Or the darkening occurred for another reason.
If a stain on the front teeth occurs as a result of a bruise, the dentist will remove the affected tissue, process and fill the canals, and, if necessary, recommend installing veneers or endo-whitening (lightening the tooth from the inside).
If the cause of dark spots is poor hygiene or poor plaque removal, professional cleaning using ultrasound or laser will help solve the problem. These methods are good at removing plaque and tartar from the enamel surface and returning the teeth to their natural shade.
If food coloring is the cause of teeth staining, professional hygiene combined with a subsequent whitening procedure can help.
Unfortunately, dark spots on teeth are caries in the vast majority of cases, and the carious process at any stage requires immediate treatment.
Causes and features of caries in the spot stage
According to Miller's chemical-parasitic theory, dental caries in the stain stage and at deeper stages develops with the participation of microorganisms. Bacteria contribute to the production of lactic acid and the destruction of inorganic components of enamel under its influence. The process of carious changes in the hardest tooth tissue is triggered by a certain type of bacteria, or rather by the products of their vital activity. Tooth enamel is unique in that it is, in theory, indestructible, since it does not contain constantly renewed cells. The extraordinary strength of this body tissue is also evidenced by the remains found by archaeologists with skulls in which teeth were preserved.
But microorganisms can still destroy tooth enamel. The main role in this destructive activity belongs to the bacterium Streptococcus mutans, which lives in the oral cavity and forms part of its microbiota. The mentioned microorganism is considered opportunistic, that is, activated under certain conditions. These include frequent and excessive consumption of sugar and other carbohydrates that can be fermented.
When sweet food enters the oral cavity, the number of cariogenic bacteria rapidly increases, and as a result, the balance of microflora changes in favor of pathogenic microorganisms. When sugar is fermented by these bacteria, the amount of acid increases, which leaches calcium and other minerals from the enamel. As a result of such exposure, the surface of the affected area undergoes characteristic changes.
Types and classification
Depending on the location of the defect formation, caries in the spot stage is divided into types:
- Fissure. The discolored area is located on the chewing surface of a molar or premolar.
- Contact. Changes are detected on the lateral parts of the tooth, which are in contact with each other.
- Cervical. The stain is found in the area bordering the gum.
The form of the disease can also be different. Progressive caries develops quickly and after a short time passes into the superficial stage. The intermittent form is characterized by periodic exacerbations and attenuation of the pathological process. Suspended caries spots can persist for years without moving to the next stage.
Treatment methods for initial caries
In most cases, treatment of caries in the spot stage is carried out without drilling. For this purpose, in particular, remineralizing therapy or deep fluoridation of enamel can be used.
When the chewing surface of a molar or premolar is damaged, the doctor often suggests invasive fissure sealing, that is, sealing the enlarged natural grooves with a sealant.
If the stain has acquired a dark shade, it is sanded or prepared, then the defect is filled.
One of the modern technologies for treating caries in the spot stage is the Icon technique. When using it, the affected tooth surface is treated with a flowing material that penetrates the enamel, fills its pores and neutralizes bacteria.
Why does the enamel color change?
Blackheads occur for many reasons, of which dentists identify the main ones:
- Presence of plaque if not cleaned regularly with a toothbrush.
- Hereditary factor.
- The presence of sealed teeth treated with metal fillings.
- Smoking and alcohol abuse.
- Long-term wearing of braces.
- Poor cleaning of dental canals due to caries.
- Erasure of enamel.
- Use of tetracycline antibiotics for treatment.