Child's nose, nasal mucosa in children
The nose of a young child is relatively small, the nasal passages are narrow, and the lower nasal passage is absent. The nasal mucosa is delicate, relatively dry, and rich in blood vessels. Due to the narrowness of the nasal passages and the abundant blood supply to their mucous membrane, even minor inflammation causes difficulty breathing through the nose in young children. Breathing through the mouth is impossible in children in the first six months of life, since the large tongue pushes back the epiglottis. The exit from the nose, the choanae, is especially narrow in young children, which is often the cause of long-term disruption of nasal breathing in them.
Paranasal sinuses in children
The paranasal sinuses in young children are very poorly developed or completely absent. As the facial bones (upper jaw) increase in size and teeth erupt, the length and width of the nasal passages and the volume of the paranasal sinuses increase. By the age of 2 years, the frontal sinus appears, and the maxillary cavity increases in volume. By the age of 4, the lower nasal passage appears. These features explain the rarity of diseases such as sinusitis, frontal sinusitis, ethmoiditis in early childhood. Consultations with a pediatric ENT specialist at the Markushka clinic.
Causes of hypertrophy
In the human body, tonsils or tonsils perform a protective function. This organ is located at the intersection of the nasal canals of the pharynx, directly at the base of the tongue. From the outer part of the neck, the tonsils are palpable, especially if they have increased significantly in size. The main function they perform is to prevent the entry of bacteria and infections along with food, water and air.
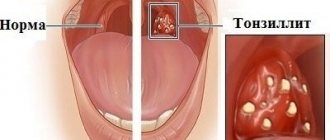
If the number of pathogens that enter the pharynx is excessive and the lymphoid tissue cannot cope with its main function, then its inflammation occurs, as a result of which it becomes the causative agent of the pathological process, as it progresses, the tonsils enlarge. When this organ is enlarged in a child, experts call this disease chronic tonsillitis or its acute form. Another name for this disease is sore throat .
An increase in the size of a child's tonsils can be considered as a sign of a decrease in the protective properties of the immune system, as well as dysfunction of the filtering organ, which accumulates microorganisms and gradually becomes inflamed.
In young children, the inhaled air is poorly warmed
Due to the insufficient development of cavernous tissue in young children, the inhaled air is poorly warmed up; therefore, children should not be taken outside at temperatures below -10 degrees. C. Cavernous tissue develops well by the age of 8-9 years, this explains the relative rarity of nosebleeds in children of the 1st year of life. A wide nasolacrimal duct with underdeveloped valves contributes to the transfer of inflammation from the nose to the mucous membrane of the eyes (examination by a pediatric ophthalmologist at the Markushka clinic). Passing through the nose, atmospheric air is warmed, moistened and purified. Every 10 minutes, a new layer of mucus passes through the nasopharynx, which contains bactericidal substances (lysozyme, complement, etc.), secretory immunoglobulin A.
Treatment of tonsillitis
The methods of therapy directly depend on the nature of the infection and the form of the disease.
So, for bacterial tonsillitis, the patient is prescribed a course of antibiotics, for the viral form of the disease - anti-inflammatory drugs, for fungal - antifungal drugs. The name and dosage of the drug is selected exclusively by the doctor. Excessive independence of parents can lead to irreversible consequences. To eliminate the unpleasant symptoms accompanying tonsillitis, the patient may be prescribed the following medications:
- antipyretic drugs in the form of syrup, tablets or suppositories;
- rinsing with antiseptic solutions;
- local anesthetic and anti-inflammatory sprays, lozenges;
- washing the lacunae of the palatine tonsils (carried out with a special syringe under the supervision of a specialist).
In addition, physiotherapeutic procedures have proven themselves well in the treatment of sore throat and chronic tonsillitis:
- electrotherapy;
- phonophoresis;
- phototherapy;
- laser therapy;
- Ural Federal District, etc.
If the parents of a sick child seek medical help too late, and the disease has become irreversible, and conservative methods have not brought the expected result, surgical treatment (tonsillectomy) may be required.
Tonsils, adenoids in a child, children
By the age of 4-10 years, the tonsils are already well developed, and their hypertrophy can easily occur. During puberty, the tonsils begin to undergo reverse development.
The tonsils are like a filter for microbes, but with frequent inflammatory processes, a focus of chronic infection can form in them, causing general intoxication and sensitization of the body.
The proliferation of adenoids (nasopharyngeal tonsil) is most pronounced in children with constitutional abnormalities, in particular with lymphatic-hypoplastic diathesis. If the adenoids are significantly enlarged (degree 1.5-2), they are removed, since nasal breathing is impaired in children (children breathe with an open mouth - the air is not purified and warmed through the nose, and therefore they often suffer from colds), the shape of the face changes (adenoid face), children become distracted (mouth breathing distracts attention), and their academic performance deteriorates. When breathing through the mouth, posture is also disturbed; adenoids contribute to the formation of malocclusion. Treatment of adenoids - homeopathic pediatrician, Markushka clinic.
Resection of the palatine tonsils (tonsillotomy) in children
Hypertrophied palatine tonsils, as well as adenoids, can cause breathing problems, snoring and even sleep apnea (stopping breathing) during sleep. A child’s tonsils often become a source of inflammation during a cold or sore throat. If a child gets sick up to seven times in a year, especially with sore throat, which is dangerous with serious complications, an otolaryngologist may advise solving the problem surgically. Today, tonsillotomy is performed using several methods: surgically, using a laser, or by freezing the tissue (cryodestruction of the tonsils).
Larynx in children
The larynx in young children has a funnel-shaped shape (later - cylindrical) and is located slightly higher than in adults (at the level of the 4th cervical vertebra in a child and the 6th cervical vertebra in an adult). The larynx is relatively longer and narrower than in adults; its cartilages are very pliable. The false vocal cords and mucous membrane are delicate, rich in blood and lymphatic vessels, elastic tissue is poorly developed. The glottis in children is narrow. Young children's vocal cords are shorter than older children's, which is why they have a high-pitched voice. From the age of 12, boys' vocal cords become longer than girls'. These features of the larynx explain the easy development of stenotic phenomena in children, even with moderate inflammatory changes in the mucous membrane of the larynx.
The increased neuromuscular excitability of a small child is also of great importance. Hoarseness, often observed in young children after a cry, often depends not on inflammatory phenomena, but on the weakness of the easily fatigued muscles of the vocal cords.
Symptoms of tonsillitis
The manifestations of tonsillitis directly depend on the form of the disease. Thus, chronic tonsillitis is characterized by mild pain in the throat, discomfort when swallowing, the appearance of bad breath, and a low-grade fever (temperature in the range of 37-37.9 ° C). The acute form of tonsillitis has a greater number of characteristic symptoms. The presence of a disease in a child is indicated by the following manifestations:
- intense pain in the throat, aggravated by swallowing, eating, talking;
- partial or complete loss of voice, hoarseness;
- swelling and hyperemia of the tonsils;
- a sudden increase in body temperature to 39-40°C, which lasts about a week;
- general weakness;
- chills;
- body aches;
- enlarged lymph nodes.
The occurrence of any of these symptoms is a serious reason to contact a qualified otolaryngologist.
Trachea in a child, children
The trachea in newborns is funnel-shaped, its lumen is narrow, the posterior wall has a wider fibrous part, the walls are more pliable, the cartilage is soft and easily compressed. Its mucous membrane is delicate, rich in blood vessels and dry due to insufficient development of the mucous glands, elastic tissue is poorly developed. The secretion of the glands provides a layer of mucus on the surface of the trachea 5 microns thick, the speed of which is 10-15 mm/min (provided by cilia). The growth of the trachea occurs in parallel with the growth of the body, most intensively in the 1st year of life and during puberty. The structural features of the trachea in children lead to the easy occurrence of stenotic phenomena during inflammatory processes; frequent isolated lesions (tracheitis), combined with damage to the larynx (laryngotracheitis) or bronchi (tracheobronchitis) are determined. In addition, due to the mobility of the trachea, its displacement may occur during a unilateral process (exudate, tumor).
Bronchi in a child, children
The bronchi are quite well formed at birth. The growth of the bronchi is intense in the 1st year of life and during puberty. Their mucous membrane is richly vascularized, covered with a layer of mucus, which moves at a speed of 3-10 mm/min, in the bronchioles it is slower - 2-3 mm/min. The right bronchus is like a continuation of the trachea; it is shorter and wider than the left. This explains the frequent entry of a foreign body into the right main bronchus. The bronchi are narrow, their cartilage is soft. Muscle and elastic fibers in children of the 1st year of life are not yet sufficiently developed. The tenderness of the bronchial mucosa and the narrowness of their lumen explain the frequent occurrence of bronchiolitis with complete or partial obstruction syndrome in young children.
Lungs in children, child
The lungs of newborns weigh about 50 g by 6 months. their mass doubles, triples by the age of 12, increases 10 times by the age of 12, and 20 times by the age of 20. The pulmonary fissures are poorly expressed.
In newborns, the lung tissue is less airy, with abundant development of blood vessels and connective tissue in the septa of the acini and an insufficient amount of elastic tissue. The latter circumstance explains the relatively easy occurrence of emphysema in various pulmonary diseases.
The formation of the lung structure in children depends on the development of the bronchi
The formation of the lung structure occurs depending on the development of the bronchi. After the trachea divides into the right and left main bronchi, each of them is divided into lobar bronchi, which approach each lobe of the lung. Then the lobar bronchi are divided into segmental bronchi. Each segment has independent ventilation, a terminal artery and intersegmental septa made of elastic connective tissue.
The segmental structure of the lungs is already well expressed in newborns. There are 10 segments in the right lung, 9 in the left. The upper left and right lobes are divided into three segments - 1, 2 and 3rd, the middle right lobe - into two segments - 4th and 5th. In the left lung, the middle lobe corresponds to the lingular lobe, which also consists of two segments - the 4th and 5th. The lower lobe of the right lung is divided into five segments - 6, 7, 8, 9 and 10th, and the left lung - into four segments - 6, 8, 9 and 10th. In children, the pneumonic process is most often localized in certain segments (6, 2, 10, 4, 5), which is associated with the characteristics of aeration, the drainage function of the bronchi, the evacuation of secretions from them and possible infection.
External respiration , that is, the exchange of gases between atmospheric air and the blood of the capillaries of the lungs, is carried out through simple diffusion of gases through the alveolar-capillary membrane due to the difference in the partial pressure of oxygen in the inspired air and venous blood flowing through the pulmonary artery into the lungs from the right ventricle. Compared to adults, young children have pronounced differences in external respiration due to the development of acini, numerous anastomoses between the bronchial and pulmonary arteries, and capillaries.
Signs of a sore throat
The first symptoms of throat diseases are pain and other discomfort. The child will begin to complain of discomfort when swallowing and speaking. You may experience a cough, runny nose, difficulty breathing, fever, or chills. Upon examination, parents may notice:
- redness and swelling of the posterior wall of the pharynx and soft palate;
- tonsillitis;
- the presence of small bubbles, after breaking through which ulcers form;
- presence of mucus or pus;
- the formation of caseous plugs - white balls on the back surface of the larynx that interfere with swallowing.
A red throat and enlarged tonsils indicate the development of a sore throat or other infectious disease (for more details, see the article: treatment of a red throat in an infant)
READ ALSO: photo of a sore throat in the mouth of children
Depending on the type of pathology, the symptoms will vary. A red throat can indicate both a common acute respiratory infection and serious pathologies that require qualified help.
READ IN DETAIL: How to treat a red throat in a child?
Depth of breathing in children
The depth of breathing in children is much less than in adults. This is explained by the small mass of the lungs and the structural features of the chest. The chest in children of the 1st year of life seems to be in a state of inhalation due to the fact that its anteroposterior size is approximately equal to the lateral size, the ribs extend from the spine almost at a right angle. This determines the diaphragmatic nature of breathing at this age. A full stomach and bloated intestines limit the mobility of the chest. With age, it gradually moves from the inspiratory position to the normal one, which is a prerequisite for the development of thoracic breathing.
How to treat?
In children, therapy for enlarged tonsils differs from that used for adults. The doctor prescribes specific medications for the child. Mostly, the specialist prescribes macrolides, since when taking penicillin-type drugs, a child’s body may experience an allergic reaction. On an individual basis, the doctor selects the dose , as well as the course of treatment, which, after the onset of remission, must in no case be interrupted.
In addition to medications, additional therapy should include, as Dr. Komarovsky agrees, rinsing procedures and inhalations, for which herbal decoctions or infusions should be used. It is also recommended to irrigate diseased tissues with children's antiseptics.
When tonsillitis occurs in a chronic form, then in this case children with this disease are registered. During periods of exacerbation - in spring and autumn, preventive therapy is carried out in full accordance with the individual program selected by the doctor. In order to ensure regulation of the size of the lymphoid gland, the doctor prescribes treatment methods that have a gentle effect on the inflamed tissue.
If a specialist observes a deterioration in the child’s immune system, rheumatism develops, or heart disease occurs in addition to disruption of the vascular system, then surgery is recommended. This measure is carried out mainly to ensure that the child does not lag behind in his development and does not experience a decline in mental abilities .
Conservative methods
Traditional therapeutic methods of treatment used for inflamed tonsils include the following:
- antibacterial methods, which are based on taking drugs with an immunostimulating effect. They also include rinsing and lubricating enlarged tonsils with antiseptic drugs,
- physiotherapeutic procedures with ultrasound, laser, as well as the use of other energy sources for therapeutic effects on the inflamed organ,
- vitamin therapy.
Oxygen requirements in children are significantly higher than in adults
The oxygen requirement in children is much higher than in adults. Thus, in children of the 1st year of life, the need for oxygen per 1 kg of body weight is about 8 ml/min, in adults - 4.5 ml/min. The shallow nature of breathing in children is compensated by a high breathing frequency (in a newborn - 40-60 breaths per 1 minute, at the age of 1 year - 30-35, 5 years - 25, 10 years - 20, in adults - 16-18 breaths per 1 min.), with the participation of most of the lungs in breathing. Due to the higher frequency, the minute volume of breathing per 1 kg of body weight is twice as high in young children as in adults. The vital capacity of the lungs, that is, the amount of air (in milliliters) maximally exhaled after maximal inhalation, is significantly lower in children compared to adults.
Thus, the anatomical and functional features of the respiratory system in children create the preconditions for milder breathing disorders than in adults.