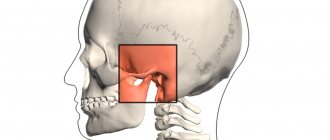
The human jaw joint is quite complex, because we can move the jaw back and forth, left and right, and even in a circle. This process involves not only the articular fossa and the head of the lower jaw, but also the meniscus, capsule and ligaments of the joint. Therefore, arthrosis of the jaw joint leads to a whole complex of disorders associated with degeneration and destruction of articular cartilage. These include digestive diseases (due to insufficient production of saliva and poor quality of chewing food), accelerated tooth wear, problems with vision and hearing, frequent migraines, slurred speech, as well as psychological problems (depression and others).
Let's figure out what arthrosis of the jaw joint is, whether it can be avoided and how to treat it correctly.
What is arthrosis of the TMJ
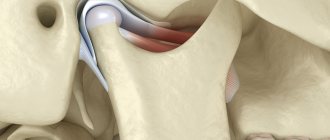
Arthrosis of the TMJ is a disease that destroys the components that form the joint (Greek arthron joint, suffix oz - destruction). First, the articular cartilage is destroyed, then the following occurs in the articular elements:
- proliferation (tissue growth);
- calcification (calcium redistribution) and ossification of cartilage;
- hyperplastic (proliferation) and destructive (destruction) processes in the epiphyseal parts of bones (these are the rounded ends of the bones - the head and fossa);
- reactive-inflammatory (from the word “response”) changes in the synovial membrane;
- fibrosis (overgrowth of connective tissue) with hardening of the joint capsule, which affects nearby muscles, tendons and ligaments.
With the destruction of cartilage, its shock-absorbing functions are reduced, and impacts are transmitted directly to the bone. Patients involuntarily increase the destruction by reacting emotionally to events - they clench their teeth, not daring to say too much, with a “stony” face and tense muscles, compressed blood vessels and stress hormones, they face the blows of fate. The amount of nutrients decreases, the TMJ would be happy to recover - but there is no building material. Instead, the epiphyseal sections of the bone are flattened under pressure, and bone growths appear on them.
Then the joint enlarges, compressing the nerve endings located nearby. The pain radiates to the ear, back of the head, and teeth. When the jaw moves, a specific clicking sound appears (occlusion-articulation syndrome).
ICD codes M.19. 0 (1, 2, 8 – last digit changes)
Causes of arthrosis of the temporomandibular joint
Arthrosis can be triggered by a one-time injury (compression, blow, bruise), as a result of which cracks and erosions appear on the articular surfaces. The disease is caused by a fracture of the condyle and condylar process if the fusion is incorrect.
Other reasons:
- prolonged stress;
- consequence of acute traumatic arthritis;
- birth trauma (arthrosis develops due to improper application of forceps);
- underdevelopment of the jaw (microgenia);
- sudden removal of molars (accident, fight);
- errors during dental prosthetics;
- impaired coordination of muscle contractions during dislocation and subsequent sharp (jerky, zigzag, circular) movements of the jaw;
- complete absence of teeth;
- deep bite;
- introduction of drugs into the joint cavity (for example, hydrocortisone, glucose solutions, novocaine).
Structure of the TMJ
Etiological factors of arthrosis (without which the disease does not develop):
- infections;
- metabolic disease;
- injuries;
- atherosclerosis of the terminal branches of blood vessels;
- prolonged spastic contraction of the lateral pterygoid muscle (responsible for moving the jaw forward and to the side).
Even children are diagnosed with TMJ arthrosis. In newborns, the disease develops as a result of birth trauma. Dysfunction in the joint due to various malocclusions is observed in 40% of children from 4 to 14 years old, but in only 1% x-rays reveal coracoid (myogenic) arthrosis.
During menopause, the likelihood of developing arthrosis due to endocrine disorders increases. With age, it is possible to develop senile, i.e. invaluable arthrosis, when cartilage tissue cannot recover, dries out and collapses.
At risk are people whose professional activities involve inadequate load on the joint (violinists), or those suffering from spasms of the masticatory muscles (bruxism).
Causes and prevention of arthrosis of the facial jaw
Based on the reasons for their occurrence, it is customary to distinguish between primary and secondary arthrosis of the jaw. The first are typical for older people (50-60 years and older) and are not associated with pathologies of the joints or dentofacial apparatus. The latter occur against the background of other disorders - for example, injury, infection, metabolic disease.
Let us consider the causes of arthrosis of the jaw joint in more detail:
- infectious disease (acute or chronic, for example, tonsillitis);
- sports or household injury (dislocation or subluxation of the jaw joint, bruise, jaw fracture);
- systematic overload (for example, when crunching nuts or intense exercise in the gym);
- dental diseases (absence of a tooth or part of it, “gentle” chewing on one side due to a dental problem);
- bruxism (unconscious grinding of teeth, usually during sleep), stress, high mental stress, mental disorders and nervous tics;
- diseases of the cardiovascular system;
- endocrine and metabolic diseases (gout, diabetes, hormonal imbalance);
- congenital anomalies of the dentofacial apparatus (including malocclusion), in which the load is distributed incorrectly;
- genetic diseases of muscle and cartilage tissue (scapulohumeral-facial muscular dystrophy, collagenopathies, as well as systemic lupus erythematosus and other autoimmune diseases);
- age-related changes (both senile and hormonal - for example, with menopause).
Often, arthrosis of the facial jaw (or temporomandibular joint - TMJ) begins due to a violation of occlusion - i.e., contact of teeth and functions of the masticatory muscles (with loss of a tooth, tumor or inflammation of the muscle muscles, lesions of the facial and trigeminal nerves). Therefore, in order to prevent arthrosis of the jaw joint, it is important to promptly replace chewing teeth with prosthetics, eliminate inflammation of the gums and dental pulp, and also treat under-erupted wisdom teeth. Do not ignore innervation disorders and muscle injuries due to stroke, surgery or incorrectly selected dentures.
Regardless of the causes, arthrosis of the jaw joint remains a chronic disease that requires lifelong monitoring and inevitably progresses.
Symptoms of TMJ arthrosis
Information about arthrosis of the temporomandibular joint on the Internet is 50% far-fetched descriptions of arthrosis of large joints, 30% is outdated data and obvious nonsense. And only 20% is true. Alas, texts are written by people without medical education, copying not from special educational literature or monographs, but from each other. Therefore, trust only trusted sources, and treat your health where there are no such ignorant things on the clinic websites.
First signs
A person may assume that he has arthrosis of the jaw when, after visiting doctors and following their recommendations, pain in the back of the head, ear, when chewing, hearing loss on one side, clicking, etc. does not go away.
Due to the structural features of the joint, the body manages to turn on the compensatory mechanism, so there is no long-term aching pain; due to the medications taken, it successfully disappears for a while.
Obvious symptoms
There are only 2 obvious symptoms (but it is also impossible to say 100% that this is arthrosis):
- displacement of the jaw to the side;
- pain when chewing.
You need to see a doctor immediately.
Symptoms of arthrosis of the jaw joint and diagnosis of the disease
The first signs of the disease usually appear between the ages of 32 and 50 years. If the patient is well informed about the symptoms and treatment of arthrosis of the jaw joint, the disease can be recognized in its infancy.
Symptoms of arthrosis of the jaw - a reminder for self-diagnosis!
You should be alert to the following changes:
- regular clicking in the joint when moving the lower jaw - the crunching seems to “send to the head”;
- limited mobility - for example, when yawning, the mouth does not open as wide as before;
- deterioration of hearing - sounds become muffled, the ears are often blocked, a characteristic noise is heard (as if a seashell was applied to the ear), deafness develops over time;
- blurred vision, which is usually accompanied by pain in the eye from the affected joint;
- pressing and bursting headaches, especially in the temporal, parotid-masticatory region;
- frequent cramps, usually painful;
- nasal congestion;
- dizziness and other problems with the vestibular system;
- abnormalities in the functioning of the salivary glands (usually dry mouth);
- facial asymmetry that has not been observed before - caused by misalignment of the jaw, the formation of bone spurs or swelling of the joint;
- fatigue when chewing food, discomfort when chewing hard and tough foods;
- morning stiffness in the jaw joint;
- decreased facial expression and difficulty swallowing food;
- increasing pain in the joint;
- toothache and tooth wear;
- numbness of the skin or mucous membranes near the affected joint;
- a feeling of “jumps” in the joint - sometimes even noticeable from the outside.
Acute piercing pain with arthrosis of the jaw joint can radiate to the ear, temple or back teeth on the affected side. However, more often patients suffer from a dull, aching pain in the jaw. In old age, pain due to arthrosis of the lower jaw may be absent, giving way to aches (including when the weather changes), heaviness and discomfort in the joint.
If, shortly before the onset of symptoms of jaw arthrosis, you have suffered from arthritis of the jaw joint, an acute infection, an exacerbation of chronic otitis, facial trauma or tooth loss, consult a doctor immediately.
Medical diagnosis of arthrosis of the jaw
When diagnosing arthrosis of the lower jaw, the doctor uses X-rays to determine the type of changes in the joint - sclerotic (replacement of normal bone tissue with abnormal one) or deformational (associated with bone abrasion or the growth of bone growths - osteophytes).
Also, x-ray examination allows us to determine the stage of arthrosis of the facial jaw:
1st - onset of the disease without significant changes in the bone;
2nd - destruction of the articular head with noticeable signs of the recovery process;
3rd - pronounced growth of bone tissue, which prevents movement in the joint;
4th - complete immobility of the jaw due to the fact that the elements of the joint are not consistent with each other.
In addition to x-rays of the jaws, the doctor may prescribe a general blood and urine test, a biochemical blood test, zonography of the affected joint, or diagnostic arthroscopy.
Between the onset of the disease and its final stage, 20-30 years may pass, or maybe 6-12 months. Do not ignore the first symptoms of arthrosis of the jaw joint. Arthrosis of the jaw is completely reversible only at the 1st stage!
How dangerous is the disease?
TMJ arthrosis is silent and unnoticeable; people live with the disease for years without even knowing about the problem. But in vain.
Degrees of TMJ arthrosis
In the Russian Federation, the Kosinskaya classification of arthrosis has been adopted, which takes into account both symptoms and radiographic data. However, the TMJ is an exception to the rule: the joint “hangs”, held by muscles and ligaments, and does not experience weight loads comparable to other joints.
When at stage 1 according to Kosinskaya the joint space narrows, the pressure on the jaw simultaneously increases, which leads to problems with the teeth, but maintains the distance. The process is gradual, so this moment can be recorded on an MRI, but since there are no symptoms characteristic of the disease in the initial stage, it cannot be said unequivocally that this is stage 1 arthrosis. Only at stage 2, when symptoms appear (pain, facial asymmetry, etc.), and the patient finally consults a doctor, is a diagnosis made.
Stage 3 according to Kosinskaya: absence of joint space, sclerosis, necrosis, inability to open the mouth, chew and speak.
Damage to the TMJ by arthrosis
Possible complications
Arthrosis is not only a problem of the joint. Compensatory, in an effort to maintain chewing function, the body redistributes the load, which leads to tooth loss and rapid wear.
The previous diseases will be reflected in TMJ synovitis, and then the inflammatory process will affect the ear and nose (with decreased hearing, nasal congestion on one side), a headache will appear, which can radiate to the neck, back of the head and not stop.
The face will lose symmetry and become pasty (the skin appears loose, finely swollen, and grayish in color). Feeding is possible only through a tube; already at the second stage the ability to fully open the mouth is lost
Any localization and form of arthrosis has serious complications, so you should not delay treatment.
See how easily the disease can be cured in 10-12 sessions.
Exacerbations
Osteoarthritis is not arthritis; a chronic disease does not have periods of exacerbation. But this does not mean that the pain will be equally aching. The inflammatory process (cold, infection, virus) spreads to the joint with the development of synovitis. Swelling and pain appear, which can appear at any radial point (from the teeth to the back of the head). The source of inflammation expands, the oral cavity, ears, and breathing through the nose are at risk.
You need to understand that the brain is located nearby. And you shouldn’t wait for necrotic tissue to give rise to oncology.
There are two main types of TMJ dysfunction:
- Myogenic (source: muscle pain);
- Arthrogenic (associated with TMJ condition).
Myogenic TMJ dysfunction usually occurs due to fatigue or tension in the masseter or accessory muscles. Leads to facial pain, headaches, and sometimes neck pain.
Arthrogenic dysfunction of the TMJ, as a rule, is the result of inflammation, degenerative changes in hard and soft tissues in the joint. It most often occurs due to capsulitis or synoviitis (inflammation), slipped discs, and degenerative arthritis.
Types of arthrosis of the temporomandibular joint
For treatment to be effective, it is important to understand that there are several types of arthrosis of the lower jaw.
Deforming arthrosis
Osteoarthritis of the TMJ usually develops after injury. The clinical course depends on the nature of growth and the location of osteophyte proliferation (towards soft tissues or the articular cavity). If bone growth is directed to soft tissues, the disease is asymptomatic for a long time. If the osteophyte grows into the cavity of the glenoid cavity, local acute pain appears, which occurs with limited jaw movement. Clicking and crunching are dull, and sometimes popping sounds appear.
The joint becomes deformed with the growth of the condyle, changes occur in the synovial membrane and are accompanied by hemorrhagic synovitis. The reason for this is irritation of the TMJ, caused by the multiple presence of dead and rejected cartilage cells (intra-articular detritus). The synovial villi on the inner lining of the joint enlarge and fat is deposited in them. Occasionally, they degenerate, forming islands of bone and cartilage tissue (metaplasia), which are separated from the articular surface and form intra-articular free bodies.
Please note: this is not salt, it is osteochondral tissue. Therefore, folk remedies for arthrosis, which can still help with gout, do not work.
Viral and infectious diseases during this period inflame the joint membrane, accelerating the destruction of cartilage and bone.
Facial asymmetry does not appear in all patients diagnosed with arthrosis deformans. This depends on the compensatory capabilities of the neuromuscular complex and on the functional grinding of the articular surfaces.
Sclerosing arthrosis
Not only vessels can be sclerotic. With arthrosis, the 2 upper layers of bone become sclerotic (bone tissue is replaced by dense connective tissue). In this case, some compaction of the head occurs, followed by expansion. Since replacement is a slow process, the body manages to compensate for the changes. Therefore, the disease goes unnoticed in the initial stages.
Neoarthrosis (post-infectious arthrosis of the TMJ)
The disease is a consequence of an acute inflammatory process in the TMJ, with repeated acute respiratory viral infections and with the presence of dysfunctional jaw syndrome (luxation, neuromuscular, occlusal-articulatory). It is asymptomatic. With exacerbation of chronic inflammation, the following is noted:
- dull, aching pain that intensifies when moving the jaw;
- crunch;
- clicking in the HFNS.
X-rays show usuria (disappearance of osteochondral tissue), defects in the articulating surfaces of bones, and sometimes the complete absence of condyles.
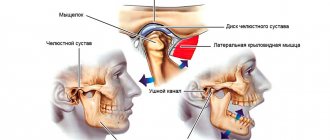
Myogenic arthrosis of the TMJ
In orthopedics, there is a separate type of deforming arthrosis of the TMJ, myogenic. Its difference: a beak-shaped bone growth on the anterior surface of the condyle.
X-ray shows myogenic arthrosis, the contours of the articular surface due to osteophyte resemble a bird
Myogenic arthrosis occurs due to prolonged spastic tension of the lateral (lateral) pterygoid muscle. Its middle bundles are attached to the anterior-inner surface of the condyle and its process. Prolonged muscle spasm leads to a lack of coordination of muscle contractions, the bone beams change direction, stretch, positioned along the direction of the tendon traction. If the spastic contraction of the muscle continues, the bones that form the joint will begin to break down.
Differences from other forms:
- the condyle always has a beak-like shape;
- bone growth (osteophyte) is always localized in a specific place;
- no restrictions on jaw movement;
- the disease occurs without facial asymmetry.
The initial stages of the disease are asymptomatic. The osteophyte grows gradually on the anterior surface of the condyle, does not rub against hard tissues, and forms a bed in soft tissues. In the joint area, nutrition is disrupted, there may be a slight swelling on the face, spider veins - but very often this is explained by fatigue, overload, without paying attention to the TMJ. Painful symptoms occur at the moment of dislocation, subluxation of the lower jaw. Since the movement of the jaw in such cases is atypical, the osteophyte injures the soft tissues, irritating the nerve endings - severe pain appears (it hurts to chew hard food), severe swelling, clicking, mild swelling and paleness of the skin flap (pastyness). At the moment the mouth opens, the jaw begins to shift to the side.
Metabolic arthrosis
This is a rare type of disease that occurs when salt metabolism in the body is disrupted. The reason is needle-shaped crystals of uric acid settling in the TMJ. In patients, large joints are first affected; they suffer for a long time from metabolic polyarthritis, the visual manifestation of which is “gouty bumps” on the joints.
Symptoms:
- significant deformation of the head of the lower jaw, detected by palpation;
- asynchronous movement of the condyles when opening and closing the mouth;
- hinge movements on the side of the diseased temporomandibular joint;
- crunch;
- local dull pain;
- when opening the mouth, the jaw moves to the side;
- Lateral position of the head leads to facial asymmetry.
On radiographs with metabolic arthrosis, the condyle is covered with whitish needle-shaped curls of various shapes that are not permeable to x-rays.
Crunching in joints - when to worry
Intra-articular injections of hyaluronic acid
Senile arthrosis of the TMJ
Senile, or invaliable, arthrosis occurs with age. “Aging” of cartilage tissue occurs in 3 stages:
- cartilage tissue becomes soft and loose;
- loses some of the water, dries out, becomes denser;
- The smooth surface disappears, the cartilage becomes fragile and becomes covered with cracks.
After 60 years, bone exposure begins. Patients feel uncomfortable chewing and clicks are noted in the TMJ. The x-ray shows subtle changes.
Features of diagnostic measures for TMJ dysfunction
For the most accurate diagnosis of damage to the articular surface of the lower jaw at the junction with the temporal bone of the skull, specialists use the following methods and the following examination plan:
- clarification of the patient’s vital functions (work specifics, presence of chronic diseases, psycho-emotional background);
- questioning the patient about the probable cause of pathological changes in the jaw (trauma, inflammatory processes in the oral cavity, past dental history, the presence of neurological pathologies);
- visual inspection of the outer surface of the projection of the joint and the oral cavity, if possible;
- palpation examination of the joints of the mandible, which helps to identify muscle tension, swelling and displacement;
- listening to sounds when opening the mouth, which can be in the form of clicks or crackling sounds;
- determination of the amplitude of jaw mobility;
- identifying the scope of possible movements;
- assessment of the functionality of the masticatory muscles;
- determining the correct bite;
- X-ray examination of the dentofacial apparatus, which will be the most informative for excluding other pathologies of teeth and gums;
- the magnetic resonance imaging method allows you to examine the soft structures of the jaw, for example, intra-articular cartilage and its physiological position, the correctness of which determines the condition of the TMJ;
- CT scan results will provide a layer-by-layer image of the bone structure of the jaws.
The results of these examinations may require consultation and treatment with a dental surgeon, traumatologist or orthodontist.
Diagnostics
In the initial stages, arthrosis of the jaw is asymptomatic (more precisely, if there is pain, discomfort - they are attributed to a cold, problems with teeth, inflammation of the facial nerve, etc.). When constant pain appears, the face loses symmetry, it is impossible to chew - the patient begins to visit doctors.
Remember: at the slightest suspicion of TMJ arthrosis, you should consult a doctor; it is impossible to make a diagnosis yourself (if you are not an orthopedist or a healer).
In the clinic to confirm the diagnosis you will need:
- take blood tests (clinical - to identify an infectious-inflammatory process, biochemistry - for arthrosis, biochemical parameters should be normal);
- take an x-ray in 2 projections (the image clearly shows the deformation of the osteophyte, the narrowing of the joint space, but the articular cartilage is not displayed in the image, and it is impossible to assess the degree of destruction of the TMJ in the early stages);
- undergo an MRI or computed tomography (MRI uses magnetic waves, and computer tomography uses X-rays, so in the early stages, MRI is an advantage).
Occasionally, an ultrasound of the joint is prescribed. In addition, a personal examination is required, because often it is necessary to treat not only arthrosis, but also to remove defects in the dentition, and to treat the accompanying inflammation of nearby tissues.
Which doctor should I contact?
The first signs of the disease are often discovered by a dentist when visiting a patient for dental treatment or complaining of pain in the jaw. When palpating the jaw muscle, its compaction is noted, and the mobility of the joint is limited. To clarify the clinical picture, the doctor may prescribe conventional or contrast radiography, as well as a computed tomography examination. Depending on the results, treatment may require the participation of several specialists.
Treatment of arthrosis that has developed against the background of anatomical pathologies of the joint (bad bite, abrasion of teeth, absence of several adjacent lateral teeth) is carried out by dental doctors. A dental therapist, an orthodontist and a prosthetist can take part in the treatment.
If there is a history of diseases that provoke the development of arthrosis of the TMJ, the dentist may refer the patient to specialists of a different profile:
- If the cause is a disease associated with metabolic disorders, an endocrinologist is involved in the treatment.
- If nerve conduction disorders are detected, the help of a neurologist will be required.
- An infectious lesion of the maxillofacial joint or the presence of an inflammatory process localized in other joints (arthritis, rheumatism) is a reason to consult a rheumatologist.
- In some cases, with arthrosis of the TMJ, partial hearing loss is observed, then an otolaryngologist joins the complex treatment.
Treatment of TMJ arthrosis
Treatment of TMJ arthrosis is complex, regardless of the stage of development of the disease. The disease cannot be overcome with one method or remedy.
Medicines for the treatment of TMJ arthrosis
In the early stages, arthrosis of the TMJ is asymptomatic, but dysfunctional syndromes may appear. Therefore, treatment should be aimed at normalizing the functioning of the lower jaw. To do this, use myogymnastic exercises (only after consultation with a doctor) and physiotherapy.
Then the position of the articular heads is normalized, the integrity of the dentition and bite are restored. For pain, clicking, crunching, and asynchronous contraction of the masticatory muscles, permanent splints, braces, and bandages are used.
At the same time, the doctor prescribes medications to restore cartilage tissue, relieve inflammation and improve metabolism around the joint.
For arthrosis of the jaw joint, consultation with a psychotherapist is indicated, because Chronic muscle spasms are always associated with problems in relationship with the world.
Medication
To restore cartilage tissue, chondroprotectors are prescribed:
- glucosamine, stimulates the production of key elements in cartilage tissue, restores the articular surface, protects from destruction;
- chondroitin sulfate, increases the ability of cartilage molecules to retain water (especially important for senile arthrosis of the temporomandibular joint), neutralizes the influence of enzymes that destroy cartilage, and stimulates the formation of collagen.
But if the cartilage is completely destroyed, chondroprotectors are not effective.
To relieve muscle spasms, the doctor prescribes mydocalm and sirdalud.
Remember: you cannot use medications on your own without a doctor. Muscle spasm is a protective reaction; without it, the TMJ will begin to deteriorate at an accelerated pace.
Drugs of this group, muscle relaxants, are used only with the simultaneous use of chondroprotectors and orthopedic treatment (splints).
Corticosteroids quickly relieve pain during synovitis, intra-articular injection only relieves inflammation, BUT the next dose is less effective (3-4 injections is the maximum), and the hormone destroys and does not heal articular cartilage. Therefore, for arthrosis of the temporomandibular joint without inflammation, drugs are not used with proper treatment.
The hyaluronic acid preparation “Ostenil mini”, a 1% solution of sodium hyaluronate (10 mg of active substance in 1 ml syringe), is also called “liquid prosthesis”. It restores the joint more effectively than chondroprotectors. 1-2 injections per year (3-4 years) are enough. There are only 2 drawbacks:
- there should be no inflammation in the joint, drugs with HA are instantly destroyed in such an environment, and the treatment will not be effective;
- this is an expensive drug (however, it is better to use it than to go under a scalpel).
For post-infectious arthrosis of the TMJ, Movalis (selective anti-inflammatory) is prescribed to suppress inflammation, as well as:
- Brufen;
- indomethacin;
- methindol;
- butadione;
- rheopirin;
- sodium salicylic acid;
- antibiotics (in the presence of low-grade fever).
Please note: long-term use of non-steroidal anti-inflammatory drugs has a negative effect on articular cartilage.
Electrophoresis with medical bile, bischofite, dimexide (compresses are also made from them), as well as with salicylic sodium (10%), lidase is indicated. Mud therapy helps a lot.
For post-infectious arthrosis, treatment is physiotherapeutic (electrotherapy with potassium iodide solution (5%) and novocaine solution (2%)). Recommended ointments are apisatron, vipratox, and an analgesic mixture.
For myogenic arthrosis, they practice novocaine blockade with vitamins B1, B12, massage using anesthetic ointments, UHF.
Metabolic arthrosis of the jaw joint is myogymnastics and the use of a splint. At the same time, salt-removing therapy (delogil, collection of salt-removing herbs) is prescribed.
Chondroprotectors: what are they, how to choose, how effective are they?
Joint pain at rest
If the condyle in the temporomandibular joint is excessively enlarged, surgical and orthopedic treatment is performed.
In addition, at any stage and for almost any type of arthrosis, vasodilators xanthinol nicotinate and pentoxifylline are prescribed, which relieve spasm of small vessels and improve blood circulation in the joint. At the same time, slight redness of the face and a feeling of heat are the norm.
Therapeutic ointments and creams do not cure advanced arthrosis of the jaw joint, but their use relieves pain, relieves swelling, and improves tissue nutrition. Finalgon and Nicoflex increase blood circulation, relieve pain and partially relax the spasmed muscle. Creams based on bee venom additionally improve the elasticity of ligaments, but due to the large number of allergic reactions, they must be used with caution. Ointments containing non-steroidal anti-inflammatory drugs (Voltaren-gel, Fastum, ibuprofen, indomethacin, etc.) are less effective than medications, but do not have as many contraindications.
Orthopedic treatment
Orthopedic devices help redistribute the load in the joint and straighten the jaw. Using splints and a sling bandage:
- functional rest is created in the joint;
- traumatic factors are eliminated;
- the activity of the chewing muscles and joints is restored.
When treating arthrosis, the dentition must be restored. Wearing mouth guards, braces, and teeth grinding are practiced.
How to treat TMJ arthrosis with exercise therapy
Physical therapy for arthrosis of the jaw joint is useful only after permission and under the supervision of a doctor.
The joint is destroyed from the inside, and the destruction of it and nearby tissues, as well as compensatory muscle spasm, intensifies with movement. Stupid exercises can cause harm, because... unknown until images are received:
- how arthrosis develops;
- what type is it;
- where are the osteophytes directed?
The joint is already receiving load - we talk, eat, opening and closing our mouths. And moving the jaw from side to side will add subluxation and swelling.
At home you can do:
- soft massage with a sponge using rotational movements around the joint to stimulate lymph outflow and blood circulation;
- gently tap a bag of raw peas or beans around the joint;
- stroke the cheek from the nose to the bridge of the nose, applying slight pressure with the palm of your hand.
Nutrition, diet
The development of arthrosis of the temporomandibular joint is not associated with dietary habits (you just don’t need to crack hard nuts so as not to break your teeth). However, it is important to pay attention to the amount of water entering the body. The individual need for clean water is calculated using the formula: 1500 ml + 20 ml per kg (over 20 kg). For example, with a weight of 60 kg, the amount of liquid is 1500 ml + 40 * 20 ml = 2300 ml
When edema occurs, diuretic herbs and herbs (birch, linden, clover inflorescences, mistletoe branches, etc.) are used.
Traditionally, for problems with joints, it is recommended to eat more vegetables and fruits (vitamins and minerals), as well as jellied meats, jelly (some patients have a special craving for soft cartilage, pig ears, etc.).
Eat a varied dietC
When pain occurs (stage 2), it is painful to eat. Food should be soft and pureed. These are juices, pureed soups, ready-made baby food in jars. Sometimes you have to feed through a tube - do not bring yourself to this state, at the first unpleasant sensations, consult a doctor.
If an operation has been performed on the joint, the food for the first time should be dietary. Food should be pureed, spicy, spicy and salty foods should be excluded.
Folk remedies
Among the folk remedies for arthrosis of the jaw, a compress with bischofite or medical bile helps a lot. But due to the fact that it is necessary to align the joint, this is a temporary measure to alleviate the condition. You still have to go to the doctor.
A compress is made only when there is no inflammation, swelling on the face or viral infectious diseases. First, place a warm (not hot!) heating pad on the sore side of the face for 3-5 minutes to warm the joint and slightly relax the spasming muscles. Then put gauze on it (attention: no colorful synthetic rags), soaked in a bischofite solution, cover first with parchment paper (cling film), then with a flannel cloth (terry towel). The compress should be kept for 1-1.5 hours, for people with sensitive skin no more than 20 minutes. If there are no negative reactions, the procedure time is increased. Course of home treatment: 10-15 compresses every other day.
A compress with medical bile cannot be used if you have pustular rashes, acne, rosacea, or rosacea. 6 layers of gauze are soaked in bile and a “sandwich” is made in the same way as with bischofite. However, they keep it for 30 minutes maximum. Course of treatment: daily for 2-3 weeks.
In case of cardiovascular insufficiency or hypertension, such procedures without medical supervision are prohibited.
When diagnosed with “metabolic arthrosis of the jaw joint,” herbal preparations that remove salts are taken. For example, collection (all herbs 100 g, grind in a meat grinder into powder):
- mint;
- buckthorn;
- dandelion;
- immortelle;
- juniper fruits;
- celandine;
- buckthorn;
- chicory (herb);
- yarrow;
- sage (leaves);
- burdock.
1.5 tbsp. collection, brew 1.5 tbsp of boiling water and infuse. Drink 0.5 tbsp. 3 times a day before meals.
This is the only type of arthritis where herbal treatment is effective. However, you can drink herbs to strengthen the immune system and for prevention during epidemics of viral infections.
Surgical operations
Surgical intervention is indicated:
- during ossification;
- with further destruction if conservative treatment does not produce results.
The joint or part of it is removed, replaced with an artificial implant or your own graft (usually part of the fibula).
Approach to treating the disease in our clinic
Our clinic is an example of integrative medicine: a synthesis of Eastern and Western approaches to treatment. In addition to neutralizing the causes of the disease and restoring the functionality of the HFNS, we restore the disturbed energy balance of the body and the integrity of its structure. Therefore, patients have the strength to cope with the disease and recover much faster than using only the usual medical protocol. All patients are different, so the appointment after the examination is individual.
We combine proven techniques of the East and innovative methods of Western medicine.
Read more about our unique method of treating arthrosis
General clinical recommendations and prevention
With arthrosis of the temporomandibular joint, it is necessary to reduce the load on the joint. To do this, you need to restore the integrity of the dentition and periodically wear braces. If you are involved in (and cannot quit) contact sports (boxing, martial arts), be sure to wear sports mouthguards.
To restore blood circulation in the joint, it is recommended to slowly (!) open and close your mouth (without sudden or lateral movements).
You will also have to get rid of habits that create additional stress on the joint:
- chew gum vigorously;
- support your cheek with your palm;
- chew seeds, nuts, hard cartilage.
Osteoarthritis of the jaw joint is called a disease of suppressed emotions. The illness can be a consequence of divorce, dismissal, or critical life situations. The most severe forms develop in nice and non-conflict people who keep their own emotions to themselves. You need to learn to enjoy life and stop seeing the world in gray colors.
Frequently asked questions about the disease
Who treats arthrosis of the temporomandibular joint?
The treatment is complex. If there is no gnathologist in the medical institution, treatment is carried out by a surgeon or orthopedic traumatologist. In this case, a dentist, a neurologist, an otolaryngologist and, if necessary, a rheumatologist and an infectious disease specialist must be involved.
Is it possible to cure TMJ arthrosis?
If bone growths have begun, the process can be stopped, but it will not be possible to defeat the disease when the joint is young and healthy. But if you start treatment at least at stage 2 of the disease, you will be able to get rid of the symptoms, stop the destruction and even restore cartilage tissue.
Why is arthrosis of the TMJ dangerous?
Deformation in the joint leads to facial asymmetry, secondary inflammation spreads to the nasopharynx and ear. Due to spasmed muscles, teeth wear out and fall out. The skin on the face becomes pasty and ages quickly.
What is the difference between arthrosis and TMJ arthritis?
Arthritis is an inflammatory process in the temporomandibular joint of infectious-allergic, traumatic, autoimmune, etc. origin, which in advanced cases can lead to arthrosis. For example, a purulent infection (purulent otitis, boil in the ear canal, flu, sore throat, mumps, etc.) infects the joint fluid. The inflammatory process spreads to the joint capsule (the local temperature rises, the blood vessels of the heads of the bones grow and dilate). The purulent process then dissolves the cartilaginous surface and meniscus, and then destroys the bone tissue, leading to arthrosis. Arthrosis destroys the joint asymptomatically at the first stage and without an acute inflammatory process. The cartilage loses moisture, dries out, and cracks. The bone then grows, changing the structure of the joint.
Literature
- Evdokimenko P.V. Arthrosis
- Petrosov Yu. A., Kalpakyants O. Yu., Seferyan N. Yu. Diseases of the temporomandibular joint
Themes
Arthrosis, Joints, Pain, Treatment without surgery Date of publication: 10/08/2021 Date of update: 11/01/2021
Reader rating
Rating: 4.67 / 5 (3)