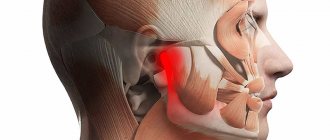
In addition to pain, TMJ arthritis can manifest itself:
- swelling and redness of the skin over the joint;
- an increase in the patient's general body temperature;
- restriction of mouth opening and inability to completely close the teeth.
Diagnosis of inflammatory processes affecting the TMJ consists of analyzing the patient’s medical history, palpation examination of the area of the joint, as well as the results of radiography and CT scans of the affected joint. Therapeutic tactics aimed at eliminating this disease involve the use of jaw immobilization, complex antibacterial therapy, chondroprotectors, physiotherapeutic procedures, intra-articular injections of corticosteroids, as well as muscle exercises.
This disease is represented by acute and chronic forms, any of the forms is accompanied by dysfunctional disorders of the TMJ. Among all diseases of the temporomandibular joint, inflammatory lesions occupy about 18%. The category of the population most often suffering from this disease is young and middle-aged people. Based on the etiological factors contributing to the development of this disease, rheumatologists, dentists and traumatologists can treat it.
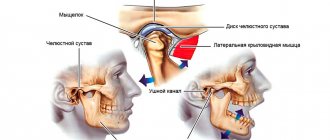
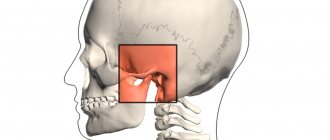
Anatomically, the TMJ is represented by a paired joint of the mandibular and temporal bones; its main function is to ensure mobility of the lower jaw. The joint itself consists of the head of the joint of the lower jaw, the articular tubercle, the mandibular fossa of the temporal bone, the articular disc, the ligamentous apparatus and the articular capsule. At the onset of the disease, periarticular tissues and the joint capsule are exposed to the pathological process. During the gradation of the disease, inflammation spreads to the surface of the joint, synovial membrane and areas of bone structures, accompanied by deformation of the cartilage and the appearance of connective tissue in the joint cavity. This disease can be complicated by deforming arthrosis, muscle contractures or bone ankylosis of the temporomandibular joint.
What is arthrosis of the TMJ
Arthrosis of the TMJ is a disease that destroys the components that form the joint (Greek arthron joint, suffix oz - destruction). First, the articular cartilage is destroyed, then the following occurs in the articular elements:
- proliferation (tissue growth);
- calcification (calcium redistribution) and ossification of cartilage;
- hyperplastic (proliferation) and destructive (destruction) processes in the epiphyseal parts of bones (these are the rounded ends of the bones - the head and fossa);
- reactive-inflammatory (from the word “response”) changes in the synovial membrane;
- fibrosis (overgrowth of connective tissue) with hardening of the joint capsule, which affects nearby muscles, tendons and ligaments.
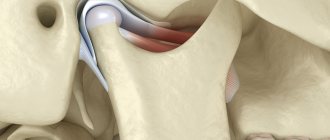
With the destruction of cartilage, its shock-absorbing functions are reduced, and impacts are transmitted directly to the bone. Patients involuntarily increase the destruction by reacting emotionally to events - they clench their teeth, not daring to say too much, with a “stony” face and tense muscles, compressed blood vessels and stress hormones, they face the blows of fate. The amount of nutrients decreases, the TMJ would be happy to recover - but there is no building material. Instead, the epiphyseal sections of the bone are flattened under pressure, and bone growths appear on them.
Then the joint enlarges, compressing the nerve endings located nearby. The pain radiates to the ear, back of the head, and teeth. When the jaw moves, a specific clicking sound appears (occlusion-articulation syndrome).
ICD codes M.19. 0 (1, 2, 8 – last digit changes)
TMJ dysfunction: what is it, how is it diagnosed?
Impaired functionality of the TMJ is an interdisciplinary pathology. Several specialists should be involved in its treatment: gnathologist, neurologist, otolaryngologist, orthopedist, psychologist, etc. Together, this problem can be solved faster and better.
TMJ dysfunction is a lack of coordinated activity of its components, muscle and occlusal disorders. The main symptoms of the pathology are pain in the joint area, temples, neck, noise effects when moving the jaw, problems with chewing food, diction, night grinding of teeth, snoring. Often, patients with TMJ dysfunction have complaints about their appearance (the beauty of their face, teeth, posture).
It is possible to discover the true cause of many complaints about the patient’s general and dental health after a face-to-face consultation with a doctor with in-depth gnathological knowledge. A thorough history, examination and physical examination allows a preliminary diagnosis to be made. Confirmation of TMJ dysfunction is provided by x-rays, CT, MRI, and ultrasound. In gnathology, the results of electromyography, phonoarthrography, and gnathodynamometry are also of greater diagnostic importance.
Functional disorders of the TMJ should be distinguished from diseases such as arthrosis, arthritis, synovitis, hemarthrosis, dislocation and subluxation of the lower jaw. Although these pathologies may be a consequence or complement each other. Therefore, the results of differential diagnosis are important here.
Causes of arthrosis of the temporomandibular joint
Arthrosis can be triggered by a one-time injury (compression, blow, bruise), as a result of which cracks and erosions appear on the articular surfaces. The disease is caused by a fracture of the condyle and condylar process if the fusion is incorrect.
Other reasons:
- prolonged stress;
- consequence of acute traumatic arthritis;
- birth trauma (arthrosis develops due to improper application of forceps);
- underdevelopment of the jaw (microgenia);
- sudden removal of molars (accident, fight);
- errors during dental prosthetics;
- impaired coordination of muscle contractions during dislocation and subsequent sharp (jerky, zigzag, circular) movements of the jaw;
- complete absence of teeth;
- deep bite;
- introduction of drugs into the joint cavity (for example, hydrocortisone, glucose solutions, novocaine).
Structure of the TMJ
Etiological factors of arthrosis (without which the disease does not develop):
- infections;
- metabolic disease;
- injuries;
- atherosclerosis of the terminal branches of blood vessels;
- prolonged spastic contraction of the lateral pterygoid muscle (responsible for moving the jaw forward and to the side).
Even children are diagnosed with TMJ arthrosis. In newborns, the disease develops as a result of birth trauma. Dysfunction in the joint due to various malocclusions is observed in 40% of children from 4 to 14 years old, but in only 1% x-rays reveal coracoid (myogenic) arthrosis.
During menopause, the likelihood of developing arthrosis due to endocrine disorders increases. With age, it is possible to develop senile, i.e. invaluable arthrosis, when cartilage tissue cannot recover, dries out and collapses.
At risk are people whose professional activities involve inadequate load on the joint (violinists), or those suffering from spasms of the masticatory muscles (bruxism).
Treatment of TMJ: what is effective?
Modern medicine gives preference to organ-preserving, atraumatic and minimally invasive methods of therapy. If there is no effect from conservative treatment, taking into account the severity of the TMJ pathology, surgery may be prescribed.
Doctors at the Sechenov University Clinic help improve the quality of life and relieve clinical manifestations of functional disorders of the jaw joint by performing the following manipulations:
- Installation of special caps or splints. This helps to level out jaw closure disorders and helps correct the bite.
- Conducting pharmacotherapy. The patient is prescribed muscle relaxants (Mydocalm, Kalmirex, Tizalud, Sirdalud) intramuscularly and/or orally, psychotropic drugs (Fluoxetine), painkillers and anti-inflammatory drugs from the NSAID group (Nimesil, Dexalgin, Ketanov, Ketonal), chondroprotectors, calcium preparations, etc.
- Intra-articular injections. Patients are injected with Botox or its analogues in this way. solution, sodium hyaluronate. This helps to relax the masticatory muscles, move the articular disc to its normal position, and replace synovial fluid.
- Physiotherapy for TMJ. This can be phonophoresis, for example, with hydrocortisone, treatment with currents of various amplitudes and strengths, myogymnastics. These methods help relieve pain, swelling, inflammation, and muscle spasms.
- Surgical intervention. It is a last resort, but effective and final. Chondroplasty of the TMJ disc and the head of the lower jaw joint is performed. Sometimes suturing of the intra-articular ligaments and capsule is required.
The level of diagnostic and therapeutic measures in the clinics of Sechenov University can be considered unprecedentedly high. Almost no one can repeat what they can do here outside the center, since they either do not have the appropriate training or equipment.
Symptoms of TMJ arthrosis
Information about arthrosis of the temporomandibular joint on the Internet is 50% far-fetched descriptions of arthrosis of large joints, 30% is outdated data and obvious nonsense. And only 20% is true. Alas, texts are written by people without medical education, copying not from special educational literature or monographs, but from each other. Therefore, trust only trusted sources, and treat your health where there are no such ignorant things on the clinic websites.
First signs
A person may assume that he has arthrosis of the jaw when, after visiting doctors and following their recommendations, pain in the back of the head, ear, when chewing, hearing loss on one side, clicking, etc. does not go away.
Due to the structural features of the joint, the body manages to turn on the compensatory mechanism, so there is no long-term aching pain; due to the medications taken, it successfully disappears for a while.
Obvious symptoms
There are only 2 obvious symptoms (but it is also impossible to say 100% that this is arthrosis):
- displacement of the jaw to the side;
- pain when chewing.
You need to see a doctor immediately.
How dangerous is the disease?
TMJ arthrosis is silent and unnoticeable; people live with the disease for years without even knowing about the problem. But in vain.
Degrees of TMJ arthrosis
In the Russian Federation, the Kosinskaya classification of arthrosis has been adopted, which takes into account both symptoms and radiographic data. However, the TMJ is an exception to the rule: the joint “hangs”, held by muscles and ligaments, and does not experience weight loads comparable to other joints.
When at stage 1 according to Kosinskaya the joint space narrows, the pressure on the jaw simultaneously increases, which leads to problems with the teeth, but maintains the distance. The process is gradual, so this moment can be recorded on an MRI, but since there are no symptoms characteristic of the disease in the initial stage, it cannot be said unequivocally that this is stage 1 arthrosis. Only at stage 2, when symptoms appear (pain, facial asymmetry, etc.), and the patient finally consults a doctor, is a diagnosis made.
Stage 3 according to Kosinskaya: absence of joint space, sclerosis, necrosis, inability to open the mouth, chew and speak.
Damage to the TMJ by arthrosis
Possible complications
Arthrosis is not only a problem of the joint. Compensatory, in an effort to maintain chewing function, the body redistributes the load, which leads to tooth loss and rapid wear.
The previous diseases will be reflected in TMJ synovitis, and then the inflammatory process will affect the ear and nose (with decreased hearing, nasal congestion on one side), a headache will appear, which can radiate to the neck, back of the head and not stop.
The face will lose symmetry and become pasty (the skin appears loose, finely swollen, and grayish in color). Feeding is possible only through a tube; already at the second stage the ability to fully open the mouth is lost
Any localization and form of arthrosis has serious complications, so you should not delay treatment.
See how easily the disease can be cured in 10-12 sessions.
Exacerbations
Osteoarthritis is not arthritis; a chronic disease does not have periods of exacerbation. But this does not mean that the pain will be equally aching. The inflammatory process (cold, infection, virus) spreads to the joint with the development of synovitis. Swelling and pain appear, which can appear at any radial point (from the teeth to the back of the head). The source of inflammation expands, the oral cavity, ears, and breathing through the nose are at risk.
You need to understand that the brain is located nearby. And you shouldn’t wait for necrotic tissue to give rise to oncology.
Arthrosis of the TMJ: how is it different from dysfunction and why is it dangerous?
The cost of inaction in case of functional disorders of the TMJ is destruction of the joint. Doctors call this degenerative process arthrosis. This is no longer just a limitation of functionality and the discomfort it causes. With arthrosis, the nutrition of joint tissues is disrupted, elasticity is lost, and dystrophy is characteristic. The TMJ changes structure and shape. And obviously not for the better.
Osteoarthritis increases gradually. At first it is morning stiffness in the joint, clicking, dull pain when talking or chewing. Lack of adequate assistance from doctors leads to the development of synovitis, jaw stiffness, facial deformation, numbness in the area of the affected organ, hearing loss, and cephalgia.
Patients with arthrosis of the TMJ require changes in lifestyle, nutrition, immediate assistance from an orthopedic dentist and gnathologist, and drug therapy. In the later stages of the disease, only a maxillofacial surgeon will help.
Types of arthrosis of the temporomandibular joint
For treatment to be effective, it is important to understand that there are several types of arthrosis of the lower jaw.
Deforming arthrosis
Osteoarthritis of the TMJ usually develops after injury. The clinical course depends on the nature of growth and the location of osteophyte proliferation (towards soft tissues or the articular cavity). If bone growth is directed to soft tissues, the disease is asymptomatic for a long time. If the osteophyte grows into the cavity of the glenoid cavity, local acute pain appears, which occurs with limited jaw movement. Clicking and crunching are dull, and sometimes popping sounds appear.
The joint becomes deformed with the growth of the condyle, changes occur in the synovial membrane and are accompanied by hemorrhagic synovitis. The reason for this is irritation of the TMJ, caused by the multiple presence of dead and rejected cartilage cells (intra-articular detritus). The synovial villi on the inner lining of the joint enlarge and fat is deposited in them. Occasionally, they degenerate, forming islands of bone and cartilage tissue (metaplasia), which are separated from the articular surface and form intra-articular free bodies.
Please note: this is not salt, it is osteochondral tissue. Therefore, folk remedies for arthrosis, which can still help with gout, do not work.
Viral and infectious diseases during this period inflame the joint membrane, accelerating the destruction of cartilage and bone.
Facial asymmetry does not appear in all patients diagnosed with arthrosis deformans. This depends on the compensatory capabilities of the neuromuscular complex and on the functional grinding of the articular surfaces.
Sclerosing arthrosis
Not only vessels can be sclerotic. With arthrosis, the 2 upper layers of bone become sclerotic (bone tissue is replaced by dense connective tissue). In this case, some compaction of the head occurs, followed by expansion. Since replacement is a slow process, the body manages to compensate for the changes. Therefore, the disease goes unnoticed in the initial stages.
Neoarthrosis (post-infectious arthrosis of the TMJ)
The disease is a consequence of an acute inflammatory process in the TMJ, with repeated acute respiratory viral infections and with the presence of dysfunctional jaw syndrome (luxation, neuromuscular, occlusal-articulatory). It is asymptomatic. With exacerbation of chronic inflammation, the following is noted:
- dull, aching pain that intensifies when moving the jaw;
- crunch;
- clicking in the HFNS.
X-rays show usuria (disappearance of osteochondral tissue), defects in the articulating surfaces of bones, and sometimes the complete absence of condyles.
Myogenic arthrosis of the TMJ
In orthopedics, there is a separate type of deforming arthrosis of the TMJ, myogenic. Its difference: a beak-shaped bone growth on the anterior surface of the condyle.
X-ray shows myogenic arthrosis, the contours of the articular surface due to osteophyte resemble a bird
Myogenic arthrosis occurs due to prolonged spastic tension of the lateral (lateral) pterygoid muscle. Its middle bundles are attached to the anterior-inner surface of the condyle and its process. Prolonged muscle spasm leads to a lack of coordination of muscle contractions, the bone beams change direction, stretch, positioned along the direction of the tendon traction. If the spastic contraction of the muscle continues, the bones that form the joint will begin to break down.
Differences from other forms:
- the condyle always has a beak-like shape;
- bone growth (osteophyte) is always localized in a specific place;
- no restrictions on jaw movement;
- the disease occurs without facial asymmetry.
The initial stages of the disease are asymptomatic. The osteophyte grows gradually on the anterior surface of the condyle, does not rub against hard tissues, and forms a bed in soft tissues. In the joint area, nutrition is disrupted, there may be a slight swelling on the face, spider veins - but very often this is explained by fatigue, overload, without paying attention to the TMJ. Painful symptoms occur at the moment of dislocation, subluxation of the lower jaw. Since the movement of the jaw in such cases is atypical, the osteophyte injures the soft tissues, irritating the nerve endings - severe pain appears (it hurts to chew hard food), severe swelling, clicking, mild swelling and paleness of the skin flap (pastyness). At the moment the mouth opens, the jaw begins to shift to the side.
Metabolic arthrosis
This is a rare type of disease that occurs when salt metabolism in the body is disrupted. The reason is needle-shaped crystals of uric acid settling in the TMJ. In patients, large joints are first affected; they suffer for a long time from metabolic polyarthritis, the visual manifestation of which is “gouty bumps” on the joints.
Symptoms:
- significant deformation of the head of the lower jaw, detected by palpation;
- asynchronous movement of the condyles when opening and closing the mouth;
- hinge movements on the side of the diseased temporomandibular joint;
- crunch;
- local dull pain;
- when opening the mouth, the jaw moves to the side;
- Lateral position of the head leads to facial asymmetry.
On radiographs with metabolic arthrosis, the condyle is covered with whitish needle-shaped curls of various shapes that are not permeable to x-rays.
Crunching in joints - when to worry
Intra-articular injections of hyaluronic acid
Senile arthrosis of the TMJ
Senile, or invaliable, arthrosis occurs with age. “Aging” of cartilage tissue occurs in 3 stages:
- cartilage tissue becomes soft and loose;
- loses some of the water, dries out, becomes denser;
- The smooth surface disappears, the cartilage becomes fragile and becomes covered with cracks.
After 60 years, bone exposure begins. Patients feel uncomfortable chewing and clicks are noted in the TMJ. The x-ray shows subtle changes.
How does the disease manifest itself?
TMJ dysfunction is directly indicated by double clicking of the jaw when opening and closing the mouth. The symptom indicates that the head of the mandible and the intraarticular disc are moving incorrectly. During a collision, the latter jumps off and moves, which is accompanied by sound. The clicking or crunching noise may be heard by both the patient and others. A stronger sound is heard when the person closes their mouth.
Pain sensations are localized in the lower jaw, neck, temples, sternoclavicular joint, and teeth. With severe migraines, the pain radiates to the eyes and ears, so the symptom is easily confused with attacks of hypertension, osteochondrosis and other pathologies. Clicking sounds when you open your mouth may or may not be painful.
Patients often complain of “seizing” of the joint. This results in difficulty opening or closing the mouth. A person has to move his jaws so that the articulation elements fall into place.
The pathology can impair hearing, cause ringing or noise in the ears, accompanied by dizziness, burning of the mucous membranes in the larynx, nose, and snoring. Painful, unpleasant symptoms cause loss of strength, depression, insomnia, and increased excitability.
Diagnostics
In the initial stages, arthrosis of the jaw is asymptomatic (more precisely, if there is pain, discomfort - they are attributed to a cold, problems with teeth, inflammation of the facial nerve, etc.). When constant pain appears, the face loses symmetry, it is impossible to chew - the patient begins to visit doctors.
Remember: at the slightest suspicion of TMJ arthrosis, you should consult a doctor; it is impossible to make a diagnosis yourself (if you are not an orthopedist or a healer).
In the clinic to confirm the diagnosis you will need:
- take blood tests (clinical - to identify an infectious-inflammatory process, biochemistry - for arthrosis, biochemical parameters should be normal);
- take an x-ray in 2 projections (the image clearly shows the deformation of the osteophyte, the narrowing of the joint space, but the articular cartilage is not displayed in the image, and it is impossible to assess the degree of destruction of the TMJ in the early stages);
- undergo an MRI or computed tomography (MRI uses magnetic waves, and computer tomography uses X-rays, so in the early stages, MRI is an advantage).
Occasionally, an ultrasound of the joint is prescribed. In addition, a personal examination is required, because often it is necessary to treat not only arthrosis, but also to remove defects in the dentition, and to treat the accompanying inflammation of nearby tissues.
How are diagnostic measures carried out?
Since the symptoms are similar to other diseases, differential diagnosis is carried out, which consists of a comprehensive instrumental and laboratory examination:
- orthopantogram (OPTG);
- teleroentgenogram (TRG);
- computed or magnetic resonance imaging (CT, MRI);
- ultrasound diagnostics (ultrasound);
- blood tests to determine the level of immunity, detection of rheumatoid factor.
An important study is an orthopantogram - a detailed panoramic image and a teleroentgenogram - a lateral X-ray of the skull. From them, the doctor can see pathological changes in the joint, the structure and structure of bone, muscle, and connective tissues.
Treatment of TMJ arthrosis
Treatment of TMJ arthrosis is complex, regardless of the stage of development of the disease. The disease cannot be overcome with one method or remedy.
Medicines for the treatment of TMJ arthrosis
In the early stages, arthrosis of the TMJ is asymptomatic, but dysfunctional syndromes may appear. Therefore, treatment should be aimed at normalizing the functioning of the lower jaw. To do this, use myogymnastic exercises (only after consultation with a doctor) and physiotherapy.
Then the position of the articular heads is normalized, the integrity of the dentition and bite are restored. For pain, clicking, crunching, and asynchronous contraction of the masticatory muscles, permanent splints, braces, and bandages are used.
At the same time, the doctor prescribes medications to restore cartilage tissue, relieve inflammation and improve metabolism around the joint.
For arthrosis of the jaw joint, consultation with a psychotherapist is indicated, because Chronic muscle spasms are always associated with problems in relationship with the world.
Medication
To restore cartilage tissue, chondroprotectors are prescribed:
- glucosamine, stimulates the production of key elements in cartilage tissue, restores the articular surface, protects from destruction;
- chondroitin sulfate, increases the ability of cartilage molecules to retain water (especially important for senile arthrosis of the temporomandibular joint), neutralizes the influence of enzymes that destroy cartilage, and stimulates the formation of collagen.
But if the cartilage is completely destroyed, chondroprotectors are not effective.
To relieve muscle spasms, the doctor prescribes mydocalm and sirdalud.
Remember: you cannot use medications on your own without a doctor. Muscle spasm is a protective reaction; without it, the TMJ will begin to deteriorate at an accelerated pace.
Drugs of this group, muscle relaxants, are used only with the simultaneous use of chondroprotectors and orthopedic treatment (splints).
Corticosteroids quickly relieve pain during synovitis, intra-articular injection only relieves inflammation, BUT the next dose is less effective (3-4 injections is the maximum), and the hormone destroys and does not heal articular cartilage. Therefore, for arthrosis of the temporomandibular joint without inflammation, drugs are not used with proper treatment.
The hyaluronic acid preparation “Ostenil mini”, a 1% solution of sodium hyaluronate (10 mg of active substance in 1 ml syringe), is also called “liquid prosthesis”. It restores the joint more effectively than chondroprotectors. 1-2 injections per year (3-4 years) are enough. There are only 2 drawbacks:
- there should be no inflammation in the joint, drugs with HA are instantly destroyed in such an environment, and the treatment will not be effective;
- this is an expensive drug (however, it is better to use it than to go under a scalpel).
For post-infectious arthrosis of the TMJ, Movalis (selective anti-inflammatory) is prescribed to suppress inflammation, as well as:
- Brufen;
- indomethacin;
- methindol;
- butadione;
- rheopirin;
- sodium salicylic acid;
- antibiotics (in the presence of low-grade fever).
Please note: long-term use of non-steroidal anti-inflammatory drugs has a negative effect on articular cartilage.
Electrophoresis with medical bile, bischofite, dimexide (compresses are also made from them), as well as with salicylic sodium (10%), lidase is indicated. Mud therapy helps a lot.
For post-infectious arthrosis, treatment is physiotherapeutic (electrotherapy with potassium iodide solution (5%) and novocaine solution (2%)). Recommended ointments are apisatron, vipratox, and an analgesic mixture.
For myogenic arthrosis, they practice novocaine blockade with vitamins B1, B12, massage using anesthetic ointments, UHF.
Metabolic arthrosis of the jaw joint is myogymnastics and the use of a splint. At the same time, salt-removing therapy (delogil, collection of salt-removing herbs) is prescribed.
Chondroprotectors: what are they, how to choose, how effective are they?
Joint pain at rest
If the condyle in the temporomandibular joint is excessively enlarged, surgical and orthopedic treatment is performed.
In addition, at any stage and for almost any type of arthrosis, vasodilators xanthinol nicotinate and pentoxifylline are prescribed, which relieve spasm of small vessels and improve blood circulation in the joint. At the same time, slight redness of the face and a feeling of heat are the norm.
Therapeutic ointments and creams do not cure advanced arthrosis of the jaw joint, but their use relieves pain, relieves swelling, and improves tissue nutrition. Finalgon and Nicoflex increase blood circulation, relieve pain and partially relax the spasmed muscle. Creams based on bee venom additionally improve the elasticity of ligaments, but due to the large number of allergic reactions, they must be used with caution. Ointments containing non-steroidal anti-inflammatory drugs (Voltaren-gel, Fastum, ibuprofen, indomethacin, etc.) are less effective than medications, but do not have as many contraindications.
Orthopedic treatment
Orthopedic devices help redistribute the load in the joint and straighten the jaw. Using splints and a sling bandage:
- functional rest is created in the joint;
- traumatic factors are eliminated;
- the activity of the chewing muscles and joints is restored.
When treating arthrosis, the dentition must be restored. Wearing mouth guards, braces, and teeth grinding are practiced.
How to treat TMJ arthrosis with exercise therapy
Physical therapy for arthrosis of the jaw joint is useful only after permission and under the supervision of a doctor.
The joint is destroyed from the inside, and the destruction of it and nearby tissues, as well as compensatory muscle spasm, intensifies with movement. Stupid exercises can cause harm, because... unknown until images are received:
- how arthrosis develops;
- what type is it;
- where are the osteophytes directed?
The joint is already receiving load - we talk, eat, opening and closing our mouths. And moving the jaw from side to side will add subluxation and swelling.
At home you can do:
- soft massage with a sponge using rotational movements around the joint to stimulate lymph outflow and blood circulation;
- gently tap a bag of raw peas or beans around the joint;
- stroke the cheek from the nose to the bridge of the nose, applying slight pressure with the palm of your hand.
Nutrition, diet
The development of arthrosis of the temporomandibular joint is not associated with dietary habits (you just don’t need to crack hard nuts so as not to break your teeth). However, it is important to pay attention to the amount of water entering the body. The individual need for clean water is calculated using the formula: 1500 ml + 20 ml per kg (over 20 kg). For example, with a weight of 60 kg, the amount of liquid is 1500 ml + 40 * 20 ml = 2300 ml
When edema occurs, diuretic herbs and herbs (birch, linden, clover inflorescences, mistletoe branches, etc.) are used.
Traditionally, for problems with joints, it is recommended to eat more vegetables and fruits (vitamins and minerals), as well as jellied meats, jelly (some patients have a special craving for soft cartilage, pig ears, etc.).
Eat a varied dietC
When pain occurs (stage 2), it is painful to eat. Food should be soft and pureed. These are juices, pureed soups, ready-made baby food in jars. Sometimes you have to feed through a tube - do not bring yourself to this state, at the first unpleasant sensations, consult a doctor.
If an operation has been performed on the joint, the food for the first time should be dietary. Food should be pureed, spicy, spicy and salty foods should be excluded.
Folk remedies
Among the folk remedies for arthrosis of the jaw, a compress with bischofite or medical bile helps a lot. But due to the fact that it is necessary to align the joint, this is a temporary measure to alleviate the condition. You still have to go to the doctor.
A compress is made only when there is no inflammation, swelling on the face or viral infectious diseases. First, place a warm (not hot!) heating pad on the sore side of the face for 3-5 minutes to warm the joint and slightly relax the spasming muscles. Then put gauze on it (attention: no colorful synthetic rags), soaked in a bischofite solution, cover first with parchment paper (cling film), then with a flannel cloth (terry towel). The compress should be kept for 1-1.5 hours, for people with sensitive skin no more than 20 minutes. If there are no negative reactions, the procedure time is increased. Course of home treatment: 10-15 compresses every other day.
A compress with medical bile cannot be used if you have pustular rashes, acne, rosacea, or rosacea. 6 layers of gauze are soaked in bile and a “sandwich” is made in the same way as with bischofite. However, they keep it for 30 minutes maximum. Course of treatment: daily for 2-3 weeks.
In case of cardiovascular insufficiency or hypertension, such procedures without medical supervision are prohibited.
When diagnosed with “metabolic arthrosis of the jaw joint,” herbal preparations that remove salts are taken. For example, collection (all herbs 100 g, grind in a meat grinder into powder):
- mint;
- buckthorn;
- dandelion;
- immortelle;
- juniper fruits;
- celandine;
- buckthorn;
- chicory (herb);
- yarrow;
- sage (leaves);
- burdock.
1.5 tbsp. collection, brew 1.5 tbsp of boiling water and infuse. Drink 0.5 tbsp. 3 times a day before meals.
This is the only type of arthritis where herbal treatment is effective. However, you can drink herbs to strengthen the immune system and for prevention during epidemics of viral infections.
Surgical operations
Surgical intervention is indicated:
- during ossification;
- with further destruction if conservative treatment does not produce results.
The joint or part of it is removed, replaced with an artificial implant or your own graft (usually part of the fibula).
Orofacial pain is widespread in the population. Patients with facial pain see doctors from many specialties, including dentists, oral surgeons, neurologists, internists, and otolaryngologists. Diagnosing facial pain can be very challenging for a doctor.
Facial pain can be caused by a number of reasons. In the International Classification of Headache and Facial Pain, 3rd revision (ICHD-3 beta), pain syndromes in the facial area are given in Chapter 11 “Head or facial pain associated with pathology of the bones of the skull, neck, eyes, ears, nose, sinuses, teeth , oral cavity or other structures of the face and neck” and in Chapter 13 “Painful cranial neuropathies and other facial pain” [1]. It should be noted that in Chapter 11, almost all sections use the term “headache”; only one section mentions facial pain per se (11.8). In Chapter 13, pain syndromes are referred to as “neuralgia” or “neuropathy.”
Most of the syndromes listed in the ICHD are not often encountered in the practice of a neurologist. One of the common mistakes in interpreting the cause of facial pain is overdiagnosis of trigeminal neuralgia (TN) followed by long-term and ineffective treatment with carbamazepine. At the same time, it has been shown that TN is a relatively rare cause of facial pain [2].
This article will focus on temporomandibular joint dysfunction (TMD). Today, TMD is considered the most common cause of chronic facial pain not associated with dental diseases [3]. Facial pain associated with pathology in the temporomandibular joint (TMJ) occurs in 19–26% of the adult population, and in women it is observed 1.5 times more often than in men [4, 5].
Clinical picture
Patients with TMD may experience pain in the face, upper and lower jaw, neck and shoulders, and in and around the ear. The pain may be constant or appear when chewing, talking, or opening the mouth. Often the pain is also accompanied by a feeling of facial fatigue and swelling.
In addition to facial pain, patients may experience headaches, neck pain, ear pain, toothache, burning and stabbing pain in the face, as well as shooting and puncture sensations. In addition to pain, there are also more rare and therefore even more difficult to diagnose symptoms: noise, ringing or congestion in the ears, non-systemic dizziness and even itching or tingling in the head and neck area. Pain may develop gradually, but many patients report an abrupt onset of pain and associated symptoms.
The occurrence of difficulties with chewing, the inability to open the mouth wide, the appearance of crunching/clicking when opening or closing the mouth, as well as blocking of the lower jaw - all this indicates damage to the TMJ itself and facilitates diagnosis.
Diagnosis and differential diagnosis
Previously, TMD was considered exclusively as a pathology of the TMJ and as a consequence of subluxation of the lower jaw, arthritis, arthrosis or trauma to the TMJ, as well as occlusal disorders [6, 7]. However, in 2014, the Diagnostic Criteria for TMD for Use in Clinical Practice and Research (DC/TMD), developed by the International RDC/TMD Consortium Network and Orofacial Pain Special, was adopted Interest Group). In accordance with these criteria, TMD is divided into two groups: pain and intra-articular pathology; their combination is also possible [8].
A large number of patients with TMD experience a painful form, that is, pain in the area of the masticatory muscles, while no pathology of the joint itself is detected. The literature describes facial pain associated with myofascial dysfunction of the facial muscles [7, 9]. The authors indicate that when palpating the muscles on the side of pain, attention was paid to the dense consistency and tension of the muscles, especially the masticatory and facial muscles, as well as severe pain and myofascial trigger points. When palpating the masticatory muscle, pain spreads to the upper and lower jaws, upper and lower molars, ear, frontal region, TMJ, and neck. When palpating the temporal muscle, pain radiates to the corresponding half of the head, forehead, upper teeth, and orbit. Since the prevalence of the painful form of TMD exceeds the prevalence of the intra-articular form [10], most patients can and should receive effective care from a neurologist. Thus, facial pain in a patient is most often caused by hypertonicity and myofascial pain syndrome in the masticatory muscles without pathological changes in the structures of the joint itself.
When a patient presents with facial pain, the neurologist needs to conduct a proper examination (palpation) in order to diagnose and optimally treat such patients. This will avoid unnecessary referral of patients to dentists and ENT doctors and unnecessary and often painful examinations.
New criteria for the correct diagnosis of TMD are presented in the table.
Diagnostic criteria for TMD DC/TMD for use in clinical practice and research (adapted from [8])
Thus, according to the diagnostic criteria for TMD for clinical use, pain disorders are not associated with the pathology of the TMJ itself and can be represented by myalgia, arthralgia and headache associated with TMD. The given criteria are based on anamnesis and clinical examination (palpation of the temporal and masticatory muscles) and do not require mandatory imaging studies. In myalgia, pain may be felt in the jaw, temple, ear, or anterior to the ear and usually changes with jaw movement, chewing, or parafunctional activities. This means that pain in the face, ear, anteriorly and near the ear, as well as noise in the ear may be symptoms of TMD and do not indicate the presence of an ENT pathology.
In the case of local myalgia, the pain felt by the patient is reproduced by palpation of the temporal and masticatory muscles within their palpable area. In myofascial pain syndrome, pain extends beyond the palpable area within or beyond the palpable muscle (myofascial pain syndrome with referred pain).
It should be noted that for a complete diagnosis, it is necessary to follow the correct muscle palpation protocol: 3 points in the temporal muscle (anterior, middle and posterior sections) and 3 points in the area of the masseter muscle (the beginning of the muscle, its body and its insertion) [11]. Palpation is carried out with one or two fingers on each side separately or on both sides at once (depending on the patient’s convenience), the duration of pressing to determine myalgia should be at least 2 s, if it is necessary to determine the subtype of myalgia - at least 5 s. In practice, it is also possible to palpate the masticatory muscle by pressing it with the examiner’s thumb in the patient’s oral cavity and with the rest of the fingers outside.
To determine the presence of arthralgia, it is necessary to confirm that the pain felt by the patient in the face is localized in the TMJ area and is reproduced with provocative tests: palpation in the area or around the condylar process of the mandible or with maximum active or passive opening of the mouth, lateral movement or protrusion of the mandible.
When pain is localized in the parotid region anterior to the pinna, identifying the specific structure involved may be challenging for the clinician. In this case, it is necessary to determine whether the pain is localized in the area of the condylar process of the mandible (arthralgia) or the masticatory muscle. In the latter case, one of the types of myalgia will be diagnosed. To determine the location of the condylar process of the jaw and confirm the source of the pain felt by the patient, it is necessary to palpate the preauricular area with the mouth closed. In case of difficulty, palpation should be performed when opening the mouth or moving the lower jaw forward (Fig. 1).
Rice. 1. Palpation to determine the location of the condylar process of the mandible. a - with comfortable closing of the mouth; b - with protrusion of the lower jaw.
To find the points of palpation of the masticatory muscle, it is necessary to ask the patient to clench and then unclench his teeth. In this case, determining the boundaries of the palpated muscle is greatly simplified (Fig. 2).
Rice. 2. Palpation of the masticatory muscle to determine the shape of the TMD. a — the origin of the muscle; b - muscle body; c — muscle attachment zone.
Palpation of the temporal muscle is much simpler. It is necessary to palpate at least 3 points in the anterior, middle and posterior portions of the muscle (Fig. 3). If there is difficulty in finding the boundaries of the temporal muscle, the patient should be asked to clench his teeth.
Rice. 3. Palpation of the temporal muscle to determine the shape of the TMD. a - anterior portion of the muscle; b - middle portion of muscle; c - posterior portion of the muscle.
Another type of painful form of TMD is TMD-related headache. In ICHD-3, beta headache associated with TMD is classified as a secondary cephalalgia and is described as “tension caused by a disorder involving structures in the region of the TMJ” [1]. The first two points are nonspecific criteria confirming the secondary nature of the pain; only point 3 contains characteristics specific to TMD: headache is provoked or aggravated by active movements of the jaw, passive movements in the usual range of jaw mobility and/or during provocative tests with temporomandibular structures, for example, by applying pressure to the TMJ and surrounding masticatory muscles. However, the comments to the diagnostic criteria contain a recommendation from the International Headache Society to use newer and more accurate criteria developed by the International Network Consortium RDC/TMD and the Orofacial Pain Study Group to fully diagnose and clarify the causes of pain associated with TMD.
Differential diagnosis of headache associated with TMD includes other forms of primary and secondary cephalgia. When carrying out differential diagnosis, it is necessary to rely on the known diagnostic criteria for these cephalgia. In the case of strictly unilateral headache, it is necessary to exclude migraine and cervicogenic headache. Patients with migraine are characterized by provocateurs of a painful attack that are not typical for TMD, migraine symptoms accompanying the attack (nausea, vomiting, phono- and photophobia), and often a hereditary history of G.B. To confirm the diagnosis of cervicogenic headache, rotation tests and diagnostic blockades of cervical structures are used [1]. In the case of bilateral localization of pain, it may be difficult to differentiate from tension headache combined with tension in the pericranial muscles. In this case, inspection and palpation shown in Fig. 1-3 are of key importance for diagnosis.
Somewhat less common in neurologist practice are intra-articular forms of TMD. It should be noted that in many cases, the identified intra-articular pathology is combined with the painful form of TMD, and is not isolated.
When there is damage to the TMJ itself, there are several forms of TMD. With various forms of displacement of the intra-articular disc with reduction, different intracapsular sounds are noted during palpation of the joint and movements of the lower jaw: crunching, crackling, clicking. Disc displacement without reduction is usually caused by spasm of the lateral pterygoid muscle [12]. When the disc is displaced without reduction, there is a pronounced limitation in mouth opening and impaired ability to eat. In the case of degenerative disc pathology, a rougher (grinding-like) and longer sound can be noted - crepitus, caused by friction of the damaged intra-articular disc. Locking of the TMJ with the mouth open and the inability to close the mouth without an auxiliary maneuver indicate subluxation of the mandible.
The examination rules for diagnosing the intra-articular form of TMD are shown in Fig. 4. To confirm the diagnosis of various intra-articular forms of TMD, an MRI examination of the joint is necessary.
Rice. 4. Palpation aimed at detecting sounds in the TMJ. a - when opening/closing the mouth; b - lateral movement of the jaw to the right; c - lateral movement of the jaw to the left; d - protrusion of the lower jaw. Palpation is carried out sequentially on each side.
Etiology and pathogenesis of TMD
The etiology of TMD is multifaceted and is a combination of psychological, postural, orthopedic, genetic, biopsychosocial and occlusal factors that disrupt the functional balance in the structures of the TMJ itself and the muscles surrounding it [6, 13, 14].
The view on the pathophysiology of TMD cannot be considered fully formed. In 1934, James Costen first gave a systematic description of this group of diseases, citing malocclusion as the main cause. For many years, it was believed that the cause of myogenic and joint disorders in TMD were malocclusion (occlusal disorders, missing teeth, suboptimal prosthetics, chewing on one side and other causes) and parafunctional activity (night and/or daytime bruxism), which leads to increased load on the TMJ and muscles that provide chewing (temporal, masticatory, medial and lateral pterygoid). Facial and jaw injuries and emotional disorders also played a significant role. In particular, the presence of symptoms of depression doubles the likelihood of developing the arthralgic form of TMD, and anxiety disorders more often accompany myalgia in TMD [15, 16]. Some authors [7] point to the role of orthopedic disorders (for example, short leg syndrome) in the genesis of TMD. During an orthopedic examination, a significant number of patients (66%) reveal asymmetries of the shoulders, shoulder blades, and shortening of one leg, which causes a compensatory change in posture and muscle imbalance throughout the entire spine. The “forward head posture” also has a serious influence on the occurrence of the myogenic form of TMD [17].
However, in recent years, a number of authors have expressed doubts about the exclusive role of dental pathology in the development of TMD. Indicate a frequent combination of TMD and various types of headache. In patients with TMD, the most common primary form of headache is migraine (55.3%), the prevalence of tension-type headache is 30.2% [18]. According to other authors [19], the prevalence of TMD in patients with chronic daily headache is 58.1%.
In recent years, the works of leading Russian and foreign researchers of chronic pain [20-22] have for the first time suggested the possible central causes of TMD, in particular the role of possible dysfunction of pain control systems. Thus, it has been shown that the prevalence of the painful form of TMD in chronic migraine is significantly higher than that in episodic migraine. The authors suggested that pain and myofascial pain syndrome in TMD may be caused by impaired processing of pain impulses in the central nervous system and are not related to peripheral/dental factors.
Treatment
Based on the current understanding of the pathophysiology of TMD, a number of treatment options have been developed. In neurological practice, treatment of TMD includes a wide range of non-drug and pharmacological approaches:
1. Patient education.
Educating patients about the causes and form of TMD and the importance of behavior modification (eg, actively focusing on not clenching teeth) is important. In case of acute pain, it is necessary to recommend a temporary refusal to eat solid foods and open the mouth wide.
2. Nonsteroidal anti-inflammatory drugs
(NSAIDs) are often the first choice drugs and are effective in relieving TMD pain. Among the large group of NSAIDs, the drug nimesulide (Nise) deserves special attention. The difference in clinical efficacy and tolerability of different NSAIDs may be due to different selectivity for COX-1 and COX-2 inhibition. Nimesulide is primarily a COX-2 inhibitor with a wide range of additional effects, which helps explain its specific anti-inflammatory and analgesic activity. More than 200 clinical studies have assessed the effectiveness of nimesulide in a wide range of pain syndromes (tooth extraction and other dental operations, hypertension, back pain, joint pain, dysmenorrhea). In these studies, nimesulide systematically demonstrated a reduction in inflammatory pain that was significantly superior to that of placebo and at least equal to or in some cases more effective than other NSAIDs [23].
The main clinical benefit of nimesulide is the time to onset and duration of pain relief. Compared to other NSAIDs, nimesulide has a faster onset of analgesic action, namely 15 minutes after oral administration [24]. It should also be noted that a rapid onset of action was noted in patients with chronic pain syndrome.
A significant advantage of this drug is the lower relative risk of complications of the upper gastrointestinal tract compared with non-selective NSAIDs due to its predominant effect on COX-2. However, a single dose of nimesulide provided higher efficacy and a faster onset of analgesic action than comparable single doses of selective COX-2 inhibitors such as celecoxib and rofecoxib [25]. When comparing nimesulide with the non-selective NSAID diclofenac, the drug showed comparable efficacy, but better overall tolerability [26].
The overall risk of severe liver reactions associated with NSAID use is low. The incidence of liver injury associated with the use of nimesulide is within the frequency range for other NSAIDs [23].
The use of all NSAIDs is associated with some cardiovascular risk and in patients with hypertension, hypercholesterolemia and cardiovascular disease, all NSAIDs should be used with caution, especially in the elderly. Risks and benefits should be assessed on an individual basis and the lowest effective dose recommended for the shortest possible period of time. Many data indicate that nimesulide demonstrates a low overall risk of cardiovascular events such as myocardial infarction or congestive heart failure [27].
An international panel of experts concluded that, when used appropriately, nimesulide remains an extremely important and safe treatment option for a variety of conditions characterized by acute inflammatory pain due to its rapid onset of analgesic action and proven positive benefit/risk profile [23].
For TMD, Nise is recommended to be used at a dose of 100 mg 2 times a day. The duration of its use, like other NSAIDs, should be limited to the minimum necessary time.
3. Gymnastics
. After applying a cold compress, exercises are performed to stretch the masticatory muscles, then a warm towel must be applied.
4. Cognitive behavioral psychotherapy and biofeedback
communications are also highly efficient.
For chronic TMD, it is recommended:
1. Prescription of the tricyclic antidepressant amitriptyline (up to 75 mg/day). The choice of amitriptyline as a first-line drug is due to the relatively high risk of developing bruxism while taking selective serotonin reuptake inhibitors [28].
2. Referring the patient to a dentist to select a special muscle relaxant splint (especially in the case of night bruxism) and assess the presence and correction of occlusal disorders.
3. In the case of myofascial pain syndrome, it is possible to inject anesthetic into trigger points in the masseter, temporal and pterygoid muscles.
4. Treatment with botulinum toxin type A for the painful form of TMD, which has demonstrated high effectiveness in a large volume of studies [9, 29]. Such therapy can allow not only to achieve long-term and sustainable relaxation of the muscles of the masticatory group and relief of pain associated with myofascial pain syndrome in these muscles, but also temporary remission of nocturnal bruxism, which will reduce the risk of developing an intra-articular form of TMD.
5. Conducting comprehensive treatment of comorbid diseases, in particular depression, anxiety disorders, chronic pain.
6. In case of proven presence of intra-articular form of TMD, impaired jaw function and lack of effect of conservative therapy, the patient should be referred to a maxillofacial surgeon [30].
TMD is considered today to be the most common cause of chronic facial pain not associated with dental disease. It has been shown that facial pain in many cases is caused by hypertonicity and myofascial syndrome in the masticatory muscles without pathological changes in the structures of the joint itself. Since the prevalence of the painful form of TMD exceeds the prevalence of the intra-articular form, most patients can and should receive effective care from a neurologist. To fully diagnose the nature of TMD, one should rely on the DC/TMD diagnostic criteria for clinical use. These criteria are based on history and clinical examination (correct palpation of the temporal and masticatory muscles) and do not necessarily require imaging studies. If typical symptoms of intra-articular pathology (primarily sound) are detected, an MRI of the joint is indicated to confirm the diagnosis.
Currently, TMD is considered a disease with a multifactorial etiology. Myofascial pain syndrome in the muscles of the masticatory group can be considered as a manifestation of a violation of antinociceptive functions, i.e., it is a reflection of central sensitization and a violation of descending pain control.
Treatment of the painful form of TMD at the first stage should be carried out by a neurologist. Recommendations for the treatment of TMD include patient education, NSAIDs, cognitive behavioral therapy, and biofeedback. For chronic pain, it is also possible to prescribe amitriptyline, administer injections of anesthetics and botulinum toxin type A, as well as referral to a dentist and maxillofacial surgeon.
The authors declare no conflict of interest.
Approach to treating the disease in our clinic
Our clinic is an example of integrative medicine: a synthesis of Eastern and Western approaches to treatment. In addition to neutralizing the causes of the disease and restoring the functionality of the HFNS, we restore the disturbed energy balance of the body and the integrity of its structure. Therefore, patients have the strength to cope with the disease and recover much faster than using only the usual medical protocol. All patients are different, so the appointment after the examination is individual.
We combine proven techniques of the East and innovative methods of Western medicine.
Read more about our unique method of treating arthrosis
Splinting the lower jaw as a method of treating TMJ dysfunction
Good results for the treatment of TMJ dysfunction are shown by applying a splint to the lower jaw. After examining the patient’s oral cavity, an individual splint is made for the jaw. Hypoallergenic flexible plastics are used that do not impede speech and hygiene procedures.
Applying a splint to the lower jaw allows you to:
- Restore occlusal height.
- Redistribute chewing loads.
- Prevent pathological tooth wear.
- A jaw splint limits the movements of the lower jaw that cause bruxism.
- Treat pain caused by improper functioning of the masticatory muscles.
- Protect the joint from repeated occlusal trauma.
- Ensure regeneration of articular tissues.
Splinting the jaw at the Novodent dental clinic relieves pain and alleviates the patient’s condition.
General clinical recommendations and prevention
With arthrosis of the temporomandibular joint, it is necessary to reduce the load on the joint. To do this, you need to restore the integrity of the dentition and periodically wear braces. If you are involved in (and cannot quit) contact sports (boxing, martial arts), be sure to wear sports mouthguards.
To restore blood circulation in the joint, it is recommended to slowly (!) open and close your mouth (without sudden or lateral movements).
You will also have to get rid of habits that create additional stress on the joint:
- chew gum vigorously;
- support your cheek with your palm;
- chew seeds, nuts, hard cartilage.
Osteoarthritis of the jaw joint is called a disease of suppressed emotions. The illness can be a consequence of divorce, dismissal, or critical life situations. The most severe forms develop in nice and non-conflict people who keep their own emotions to themselves. You need to learn to enjoy life and stop seeing the world in gray colors.
Frequently asked questions about the disease
Who treats arthrosis of the temporomandibular joint?
The treatment is complex. If there is no gnathologist in the medical institution, treatment is carried out by a surgeon or orthopedic traumatologist. In this case, a dentist, a neurologist, an otolaryngologist and, if necessary, a rheumatologist and an infectious disease specialist must be involved.
Is it possible to cure TMJ arthrosis?
If bone growths have begun, the process can be stopped, but it will not be possible to defeat the disease when the joint is young and healthy. But if you start treatment at least at stage 2 of the disease, you will be able to get rid of the symptoms, stop the destruction and even restore cartilage tissue.
Why is arthrosis of the TMJ dangerous?
Deformation in the joint leads to facial asymmetry, secondary inflammation spreads to the nasopharynx and ear. Due to spasmed muscles, teeth wear out and fall out. The skin on the face becomes pasty and ages quickly.
What is the difference between arthrosis and TMJ arthritis?
Arthritis is an inflammatory process in the temporomandibular joint of infectious-allergic, traumatic, autoimmune, etc. origin, which in advanced cases can lead to arthrosis. For example, a purulent infection (purulent otitis, boil in the ear canal, flu, sore throat, mumps, etc.) infects the joint fluid. The inflammatory process spreads to the joint capsule (the local temperature rises, the blood vessels of the heads of the bones grow and dilate). The purulent process then dissolves the cartilaginous surface and meniscus, and then destroys the bone tissue, leading to arthrosis. Arthrosis destroys the joint asymptomatically at the first stage and without an acute inflammatory process. The cartilage loses moisture, dries out, and cracks. The bone then grows, changing the structure of the joint.
Literature
- Evdokimenko P.V. Arthrosis
- Petrosov Yu. A., Kalpakyants O. Yu., Seferyan N. Yu. Diseases of the temporomandibular joint
Themes
Arthrosis, Joints, Pain, Treatment without surgery Date of publication: 10/08/2021 Date of update: 11/01/2021
Reader rating
Rating: 4.67 / 5 (3)