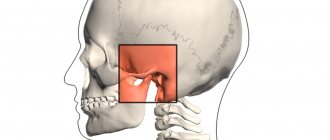
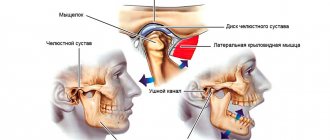
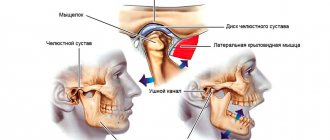
The temporomandibular joint (hereinafter referred to as the TMJ) connects the upper and lower jaw. There are two TMJs in our body - left and right. The temporal bones of the skull on each side and the head of the human mandibular bone (mandible) in normal condition have a kind of lining - an articular disc.
This disc is oval in shape, its task is to absorb the movements of the movable lower jaw in relation to the stationary parts of the skull. The disc is fixed by ligaments coming from the articular head of the mandible. The right and left articular discs should work synchronously, but in reality the situation often differs from the anatomical axioms.
Location and functions of the temporomandibular joint
The temporomandibular joint (TMJ) is considered one of the most complex joints in the body. It is formed by the head of the lower jaw, as well as the articular surface of the temporal bone. The joint is held in place by the joint capsule, ligaments and muscles. There are two temporomandibular joints, right and left. They move simultaneously and synchronously. It is this paired joint that provides all the variety of movements of the lower jaw in three planes (back and forth, up and down, from side to side). This ensures the performance of complex functions such as speech, chewing food , and breathing.
If the condition of the tissues in the system of muscles, ligaments, cartilages and bones deteriorates, the balance is disturbed - this leads to various dysfunctions of the TMJ: impaired or limited mobility, abrasion of the articular surfaces and other pathologies.
What is a temporomandibular joint dislocation?
The extraordinary mobility of the TMJ, which provides all the variety of movements of the lower jaw, also has a downside - these joints are subject to frequent subluxations and dislocations.
During normal functioning of the joint, the head of the mandibular bone leaves the glenoid fossa and then returns back. But under certain conditions, this reverse movement may not occur: the head extends too far and gets stuck in that position. Most often this occurs due to weakening of the articular ligaments, the function of which is to hold the joint together. As a rule, the situation is complicated by the fact that during a dislocation or subluxation, the facial muscles are seized by a spasm, which fixes the displaced position of the joint.
There are dislocations and subluxations of the TMJ. With subluxation, the articular head only deviates slightly from its natural position, while with dislocation, complete displacement and exit from the articular fossa occurs.
Both pathologies are unilateral and bilateral. This means that displacement of the articular head can occur on one side (right or left) or simultaneously in both joints. In addition, depending on the direction of displacement, anterior, posterior and lateral violations are distinguished. If this happens for the first time, they speak of an acute form of the disease. There is also a chronic dislocation of the TMJ, which is characterized by numerous relapses. The pathology acquires a chronic form when the ligaments of the joint are significantly weakened, as well as in the absence of teeth, impaired occlusion (closing) and other defects.
The most common are anterior acute bilateral dislocations. Lateral forms, as a rule, accompany injuries of the lower jaw, including fractures.
Surgery
Surgical intervention is more often prescribed for old injuries, when the joints have had time to change and become thinner under the influence of negative internal or external factors. Surgeons use several treatment methods.
Lindemann method. The purpose of the operation is to increase the size of the tubercle. Teflon materials are embedded into it and secured in place with metal seams. In addition, the articular notch is deepened. After Dindeman's operation, recurrence of dislocation is rarely observed.
Rauer's method. During the intervention, the articular tubercle is enlarged using grafts. Rib cartilage is used as the implanted material. Additionally, the joint capsule is reduced for better fixation in the jaw apparatus.
Self-reduction of a dislocated jaw is only possible if the victim or his relatives are trained in the technique of inserting the joint. Inept actions lead to fractures of bone structures, damage to soft tissues and nerve endings. The consequences of this require surgical intervention.
Prevention of the problem includes avoiding opening objects with your mouth and minimizing the consumption of hard foods. If you are prone to jaw loss, you should undergo regular dental examinations and diagnostic measures.
Causes of TMJ dislocation
TMJ dislocation is a fairly common occurrence. As a rule, it is caused by weakening of the articular ligaments in combination with too wide movement of the lower jaw or mechanical impact on it, for example, during a blow to the chin area.
The most common causes of acute forms of joint dysfunction are wide opening of the mouth during dental treatment, during yawning or screaming, and medical manipulations on the trachea, in particular during intubation.
There are a number of factors that can provoke an acute condition or the development of a chronic form of pathology. First of all, these are various violations of occlusion (closing), bite, and lack of teeth. Over time, such defects lead to various dysfunctions of the TMJ, while the ligaments that hold the joint, as well as the facial muscles, are weakened. Patients often notice that the dislocation was preceded by the symptom of “jamming” (that is, it is difficult to open the mouth), as well as pain and clicking when chewing [1].
Causes of TMD
There are about 70% of people suffering from this pathology, and in all age groups. The cause of this disorder is very difficult to establish.
In fact there are many of them:
- improper dental treatment (dentist mistakes when filling a tooth, prosthetics);
- malocclusion;
- sharp tension in the masticatory muscles when chewing hard and rough food;
- grinding and increased wear of teeth;
- physical activity leading to overstrain of individual muscle groups;
- problems with posture due to insufficient physical activity;
- stress;
- long-term absence of chewing teeth.
Symptoms of TMJ dislocation
The most characteristic sign of TMJ dislocation is limited mobility of the lower jaw, up to the inability to close the mouth. In addition, the pathology is usually accompanied by tension in the facial muscles.
In the bilateral anterior form, the lower jaw is displaced downward, the patient cannot close it independently, and movements are impossible. This condition is accompanied by constant pain, excessive salivation, and slurred speech. The doctor can palpate the temporal area under the tragus of the patient's ears and detect depression on both sides.
For unilateral anterior dislocation, a characteristic symptom is pronounced facial asymmetry. The lower jaw is displaced downward and to the side, in the direction of the healthy joint. The mouth is half-open, speech is slurred, and excessive salivation is also observed. Such dislocations, as a rule, occur due to a lateral impact in the lower jaw area.
To clarify the diagnosis, the dental surgeon may refer the patient for an X-ray or computed tomography scan of the joints. This allows you to clarify the shape of the dislocation, as well as exclude possible fractures or bone cracks that could have occurred as a result of the injury.
Methods and procedure of treatment
Dislocations of the TMJ can lead to damage to the articular heads, pain, restrictions in the movement of the lower jaw, difficulty chewing food and other disorders. Thus, according to statistics, in 30% of patients, TMJ pain dysfunction syndrome is caused by dislocation of the articular disc [2].
If you experience any symptoms that indicate dislocation or subluxation of these joints after a potentially traumatic situation, you should immediately seek help from an oral surgeon. After clarifying the diagnosis, he will determine the treatment.
Reduction of the TMJ occurs, as a rule, according to the so-called Hippocratic method. It is performed under local anesthesia. The patient is seated with support on the back of the head, and the doctor manually (using his hands) presses on the lower jaw, as if inserting it into its usual position. When the articular heads enter the articular fossa, a characteristic click is heard. At the same time, the facial muscles relax.
There are other common methods of reduction. Among them are the methods of Popescu, Gershuni and others. In rare cases when manual reduction is not possible, a specialist may resort to surgery. The operation is performed only under general anesthesia.
After the dislocation is reduced, a special relaxation splint is applied to the lower jaw, which limits the mobility of the joints. The duration of such treatment is 2-3 weeks [3]. To eliminate pain, painkillers and physiotherapy are used.
What methods does a gnathologist use to identify the disease?
The patient's complaints and the presence of one or more symptoms of the disease are not enough to establish an accurate diagnosis. A comprehensive examination and cooperation between doctors of various profiles is necessary, in particular consultation with an otolaryngologist, neurologist, rheumatologist and other specialists. The interaction between a dentist and an osteopath is also productive.
To clarify the diagnosis, a gnathologist will conduct a comprehensive examination, apply manual examination methods, including palpation and auscultation, and evaluate jaw mobility. Treatment of TMJ cannot begin without first checking the condition of the muscles and tissues in the head and neck area to determine signs of inflammation.
Modern methods of diagnosing and treating TMJ dysfunction necessarily involve the use of special equipment. To assess the condition of the jaw joints, three-dimensional images of this area obtained using X-rays, CT scans, and magnetic resonance imaging (MRI) help, first of all.
Prevention of TMJ dislocation
For patients prone to this pathology, it is important to adhere to preventive measures. They are aimed at eliminating joint hypermobility and unloading them. For this it is recommended:
- restriction of wide mouth opening (for example, the patient is advised to hold the lower jaw with a fist from below when yawning);
- a gentle diet that excludes excessively solid foods;
- wearing special devices and devices that provide restoration of the TMJ ligaments: trainers, collars, splints.
When the ligaments are weakened, in order to prevent dislocations and dysfunctions of the TMJ, it is important to strengthen them with the help of special exercises (myogymnastics), which are available to everyone.
|
An important role in the prevention of dislocations and subluxations of the TMJ is played by restoring the integrity of the dentition and bringing occlusion to normal. Therefore, if a patient has malocclusion or missing teeth, a dental specialist recommends prosthetics and orthodontic treatment to correct defects in the closure of the dentition.
List of sources
- Sablina G.I., Kovtonyuk P.A., Soboleva N.N. Clinical and radiological aspects in the diagnosis and treatment of pathology of the temporomandibular joints // Acta Biomedica Scientifica. 2013. No. 5 (93). URL: https://cyberleninka.ru/article/n/klinicheskie-i-rentgenologicheskie-aspekty-v-diagnostike-i-lechenii-patologii-visochno-nizhnechelyustnyh-sustavov (date of access: 08/03/2020).
- Tlustenko V.P., Potapov V.P., Kameneva L.A., Pyatanova E.A., Simonov A.S. Diagnosis and complex treatment of temporomandibular joint pain dysfunction syndrome // Saratov Journal of Medical Scientific Research. 2013. No. 3. — URL: https://cyberleninka.ru/article/n/diagnostika-i-kompleksnoe-lechenie-sindroma-bolevoy-disfunktsii-visochno-nizhnechelyustnogo-sustava (date of access: 08/03/2020).
- Khvatova V. A. Clinical gnathology. - M., 2005 // URL: https://www.stomatkniga.ru/stomatall/241-hvatova/ (date of access: 08/03/2020).
What is the clinical picture?
Symptoms of TMJ dysfunction are severe and require immediate treatment. However, differential diagnosis with subluxation of this joint is still required. Their symptoms are similar, but the therapeutic tactics are fundamentally different.
The main signs of temporomandibular syndrome that determine treatment:
- increased tone of the muscles that move the jaw;
- pain at rest and when opening the mouth in the TMJ area;
- decreased hearing acuity, tinnitus;
- at the moment of opening and closing the mouth there is a sharp crunch, click, crack;
- slight swelling of the face;
- uneven movement of the joint when opening the mouth;
- insomnia, depression;
- headache;
- neck problems.
Signs of the disease can appear all at once, or 1-2. Only a doctor can make an accurate diagnosis.