The clinic of orthodontics, gnathology, and aesthetic dentistry MY ORT offers treatment for arthritis of the temporomandibular joint. This disease is rare, but requires timely attention from a specialist to avoid serious complications.
Arthritis of the TMJ, depending on the causes, is divided into three types:
- The infectious form is a consequence of a previous disease or inflammatory process. The main causes are previous tuberculosis, syphilis, gonorrhea, diseases of a rheumatological nature.
- The dystrophic form appears with constant heavy loads on the joint area. Such regular exposure causes tissue changes and causes illness.
- Traumatic arthritis develops against the background of a severe bruise or injury. The danger of this form is that the Patient does not immediately understand the development of the problem. After a bruise, pain and swelling are observed. But it is precisely these symptoms that indicate the development of damage to the joint area, which many patients mistakenly do not pay attention to.
According to the method of infection penetration into the blood, arthritis is divided into hematogenous, contact, and direct. In hematogenous infection, pathogenic bacteria enter the body through the blood. In the second method, the source of infection becomes inflammatory processes in the lower jaw, middle ear or salivary gland. With timely treatment, complications rarely develop. But with a chronic form or lack of therapy, there is a high risk of developing arthritis. The direct method involves injuries or complications that develop after surgical operations.
Characteristics of the disease
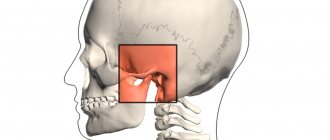
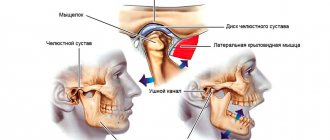
In medicine, the disease is called arthritis of the temporomandibular joint (TMJ). With the help of this joint all movements of the lower jaw occur.
The inflammatory process can occur in acute or chronic form. The main sign of the development of pathology is restriction in the movement of the lower jaw.
Such a pathology requires complex treatment and intervention by specialists of various profiles.
Depending on the area of localization, there are several forms of arthritis:
- disease of the lower or upper joint;
- arthrosis of the upper jaw joint.
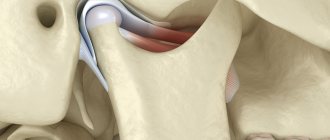
Osteoarthritis occurs when a joint is severely deformed. The lesion affects both areas of the jaw node, the cartilage tissue is destroyed. In the first stages, the joint capsule becomes inflamed, then the cartilage tissue is affected.
Traumatic inflammation
The first thing that is required is to ensure the immobility of the affected joint. This should be done by a professional traumatologist. The patient's jaw is fixed with a sling-shaped bandage equipped with a special plate that prevents the jaws from closing. This allows the victim to eat food, even if only in liquid form. Cold compresses are recommended to prevent swelling; At the same time, the doctor will prescribe medications that prevent the development and spread of inflammatory processes. In most cases, systemic administration of painkillers is also required, since injuries are associated with a gross violation of tissue integrity, which can lead to painful shock.
After the swelling subsides, physical therapy will be added to the medicinal treatment methods, designed to prevent the affected joint from fusing into a fixed conglomerate. Physiotherapy is also used: UHF, electrophoresis, diadynamic therapy, phonophoresis with hydrocortisone.
Risk factors
Main reasons:
- Injury. The cause in this case may be a bruise, a blow, or a sudden opening of the mouth.
- Infection of ENT organs. Arthritis of the maxillary joint can be caused by streptococci, chlamydia or tuberculosis.
- Osteomyelitis.
- Untreated caries.
- Periodontal diseases.
- Otitis.
In addition, the following conditions may also affect the development of jaw arthritis:
- Gout.
- Systemic lupus erythematosus.
- Diabetes.
- Thyroid diseases.
- Rheumatoid and reactive arthritis.
Sometimes inflammation can be caused by general hypothermia of the body.
Diagnostics
In principle, a diagnosis of “jaw arthritis” can be made based on severe symptoms. However, the doctor’s goal is to establish the reasons for its development, only then will treatment of the jaw joint be successful. Therefore, a whole medical consultation may be needed, which may include:
- orthopedist in tandem with a traumatologist. Their examination is a priority, since it is necessary to exclude a fracture of the jaw, damage to cartilage or ligaments;
- dentist: his task is to make sure that jaw arthritis is not a complication of a diseased tooth;
- an otolaryngologist checks the condition of the ENT organs to exclude from the list of possible causes of diseases of the nose, throat, ears and accompanying sinuses;
- An infectious disease specialist will be needed if inflammatory processes of a viral or bacterial nature are detected in the body. In case of tuberculosis, a consultation with a phthisiatrician is required, and in case of skin rashes and unfavorable test results, the patient will be referred to a dermatovenerologist;
- A rheumatologist will prescribe treatment if the jaw is affected by rheumatoid arthritis.
If during the examination there are suspicions of problems with the trigeminal nerve, a visit to a neurologist will be mandatory.
One of the first instrumental studies will be radiography. This technique has a fairly low accuracy, but it is inexpensive and allows you to determine whether a fracture has occurred. To identify the presence/absence of microcracks, tomography, computed tomography or magnetic resonance imaging is prescribed.
How does the disease manifest itself?
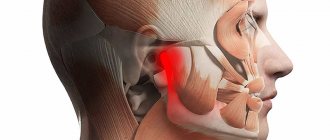
- pain in the jaw area, radiating to other parts of the face and intensifying when opening the mouth;
- restrictions in joint movement;
- dizziness, chills;
- general weakness;
- increased body temperature (may be over 38 degrees);
- sleep problems;
- jaw clicks;
- joint pain on palpation;
- deformation of the oval of the face due to the fact that the chin begins to move to the side;
- hearing problems.
The important thing is that with arthritis of the jaw joint, purulent inflammation can begin! In such a situation, the joint turns red, swells and becomes very sensitive. A compaction is felt in the area of the mandibular joint. The skin changes its color, speech is impaired, and the process of chewing food becomes difficult.
Rheumatoid inflammation
This type of jaw arthritis is mostly treated by a rheumatologist, although further guidance may be needed from other doctors. Drug treatment is mainly limited to relieving inflammation and pain; Physiotherapeutic procedures act as a supporting and accelerating effect. But therapy is not limited to these areas only , since with rheumatoid arthritis there is a very high probability of developing ankylosis of the joint, which threatens partial (and sometimes complete) loss of its mobility. This phenomenon is explained by pathological growth of tissue in the articular cavity; there is no gap left for rotation of the joint parts. Therefore, a person with such a diagnosis must constantly work on the diseased joint. The exercises are simple, but require regular performance, at least three times a day, and only after pain has been eliminated and inflammation has been relieved.
Experts in physical therapy consider four exercises to be the most effective:
- the chin is pressed with the palm from below, the mouth slowly opens, overcoming resistance. With the same speed and the same pressure, the mouth closes;
- the chin is grasped with the fingers, the jaw rises and falls. Your hand should press in the “down-back” direction;
- fingers press on the side of the jaw; the chin moves left and right. Then pressure is applied from the opposite side, and the exercises are repeated;
- the chin is pushed back by the hand; The jaw should be pushed forward as much as possible.
Each exercise is repeated three times. When performing them, pain may begin; if they are strong, you should do fewer approaches per day, reduce the intensity of pressure, or even take a break for several days. If the pain does not go away, the supervising doctor should be notified about the condition of the jaw.
It is worth making one more clarification. Like other diseases, inflammation of the jaw joint can go from acute to chronic. In this case, after the onset of a period of remission, the main emphasis in treatment is on physical therapy. In addition to the already mentioned electrophoresis and UHF, mud therapy and paraffin therapy provide good therapeutic results.
Type of pathology
The clinical picture of arthritis depends on the form in which the disease occurs:
Acute form.
It is expressed by swelling of the soft tissues and severe pain in the affected area. As a rule, the acute form is the result of some kind of injury.
Chronic form.
This form is manifested by aching pain and difficulty opening the jaw, especially in the morning.
Infectious form.
Most often it is a consequence of a previous illness (flu, ARVI). Infectious arthritis is characterized by severe pain that makes it difficult to open the mouth. The pain radiates to the ears, temples and back of the head.
Traumatic appearance.
The most common form of the disease that occurs against the background of trauma.
Specific arthritis.
Rare disease. As a rule, it occurs as a consequence of syphilis, tuberculosis or gonorrhea.
Purulent form.
It is a consequence of acute arthritis in an advanced form. A compaction forms in the area of the mandibular joint, and body temperature may increase.
Rheumatoid form.
Constant pain in the maxillary joint area. With this form, the clinical picture may be supplemented by pain in the knee, hip or elbow joint.
Depending on what caused the inflammation, the following routes of infection are distinguished:
- Hematogenous. Bacteria enter the joint along with the blood (syphilis, tuberculosis, measles, etc.).
- Contact path. The disease develops due to damage to areas located near the maxillary joint (otitis, phlegmon, abscess).
- Straight way. Develops due to direct penetration (wound, jaw fracture).
The form of pathology can be identified only after examination and diagnostic testing.
Infectious inflammation
If the cause of arthritis in the jaw joint is the action of harmful organisms, the main focus of therapy is treatment of the provoking disease. Until it is clear which aggressor started the inflammatory process, the doctor prescribes antibacterial drugs with a wide range of influence. When the pathogen is identified, the medications are replaced by those that most effectively fight the specific disease.
Non-steroidal anti-inflammatory drugs are also included in therapy, whose task is to counter the spread of inflammation. They are often combined with antihistamine complexes to make the swelling go down faster.
If conservative treatment is ineffective (usually this happens in the later stages of the disease), surgical intervention is prescribed. The operation is performed under general anesthesia, the cavity is cleaned of pus and a drainage is installed to drain the secreted fluids from the tissues. Postoperative treatment consists of painkillers, anti-inflammatory and antibacterial drugs. If recovery proceeds without pathologies, physiotherapeutic procedures are prescribed 3-4 days after the surgeon’s work. Until the drainage is removed, the patient is prescribed a strict diet consisting exclusively of liquid food.
Treatment of TMJ arthritis
When TMJ arthritis is diagnosed, treatment involves constant rest for the patient.
The acute course of the disease is treated according to the following algorithm:
- immobilization of the affected joint (for this, an unloading belt or intermaxillary ligature is used);
- then the doctor selects and prescribes a course of antibiotics, taking into account the characteristics of the infection that provoked the disease and the patient’s individual sensitivity to medications;
- To reduce and subsequently eliminate the inflammatory process, non-steroidal medications are prescribed;
- drugs are prescribed that can suppress the effect of free histamine;
- the patient’s state of mental peace is maintained by sedatives;
- to achieve maximum effect, a course of physiotherapy is prescribed: novocaine electrophoresis, laser therapy;
- Compresses with demixide are regularly applied to the affected side;
- if there is an admixture of pus in the joint, then aspiration is indicated.
Subacute stage of the disease (begins after 14-21 days) and is treated with the following method:
- restoration of damaged joint tissues and prevention of scarring;
- prescribing medications that increase microcirculation;
- a complex of vitamins to boost and maintain immunity;
- biogenic stimulation;
- enzyme therapy.
Forecast and prevention of TMJ arthritis
If, upon detection of the first symptoms of the disease and timely contact with a specialist, the correct treatment is performed, the prognosis for recovery is favorable. This applies to any form of TMJ arthritis. If you neglect the symptoms and endure pain, then there is a risk of developing TMJ ankylosis.
The main preventive measure that will allow you to avoid the disease is the sanitation of the oral cavity, the implementation of regular hygiene procedures, as well as the treatment of infectious diseases under the close supervision of a doctor.