The topic of anesthesia in dentistry is one of the most discussed, since its use allows most dental procedures to be performed painlessly for the patient. However, treatment involving serious interventions (treatment of pulpitis, tooth extraction, prosthetics) is significantly complicated if the patient is allergic to anesthesia.
According to experts, allergic reactions, hypersensitivity to the components of the drug occur in 15-20% of patients. Allergies have different causes and manifestations, and accordingly, the solution in each situation must be individual.
Allergy to anesthesia in dentistry: main types
The reaction to anesthesia has 3 different development mechanisms:
- allergic;
- toxic;
- psychogenic.
Allergies directly to an anesthetic drug are extremely rare, difficult to diagnose, and have a cumulative nature. As a rule, the reaction occurs after the 2-5th application of the anesthetic and is manifested by both local and generalized symptoms (urticaria, edema, anaphylactic shock).
Most often, an allergy occurs not to the anesthetic itself, but to the excipients that are present in it or in the packaging (latex, parabens, bisulfites that prevent the oxidation of active ingredients). As a result, the patient experiences a toxic reaction to dental anesthetics and is the most common.
The psychogenic type of allergy is not a problem of somatic origin. It is associated with the patient’s fear of dental procedures and increased anxiety. The most common psychosomatic reaction to local anesthesia is fainting after injection.
What allergy medications are there?
Medicines used to prevent and relieve allergy symptoms are called antihistamines. Their mechanism of action is to block the production of histamine, a chemical that is normally present in the human body, is involved in immune processes and regulates various physiological functions. When an allergen enters the body, a large amount of histamine is released. This leads to an inflammatory response that manifests itself as allergy symptoms. In order not to harm yourself and restore the normal state of the body as quickly as possible, it is important to know which allergy medicine can be used and what the features and differences are between the presented drugs. There are three generations of antihistamines.
How does an allergy to local anesthesia manifest: symptoms
Symptoms depend on the mechanism of allergy development. With a contact allergy, the patient experiences:
- itching;
- burning;
- development of allergic stomatitis;
- edema.
An allergy to the components of the drug can cause a reaction in the skin, respiratory system, or cardiovascular system. In severe cases of allergies, anaphylactic shock may develop.
Symptoms:
- tingling of the facial skin;
- general weakness;
- the appearance of chest pain.
In the absence of timely medical care, swelling of the respiratory tract begins, heart failure, and convulsions develop.
A toxic reaction differs from an allergy in both its symptoms and the nature of its effect on the body. Anesthetic drugs contain vasoconstrictor components.
How does an allergy to anesthesia manifest itself with increased vascular permeability, direct contact with a needle into a blood vessel when the anesthetic is administered:
- acceleration/deceleration of heartbeat;
- dizziness;
- lethargy;
- decreased visual acuity;
- noise in ears.
Symptoms
Signs of allergies are presented in the following list:
- Changes in taste sensations - when eating food, a bitter, sour or metallic taste appears, which is not characteristic of cooked dishes;
- Burning sensation in the mouth or tongue;
- Excessive salivation or, conversely, complete dry mouth;
- Inflammation of the mucous membrane, tongue and gums: swelling, redness, the appearance of small ulcers and bleeding;
- Electrical discharges in the oral cavity, due to the presence of two or more metal alloys in the filling unit;
- Redness and swelling of the eyelids, nose, lips, cheeks, accompanied by a sore throat.
These are the most common reactions of the body to low-quality filling and orthodontic preparations.
Allergy to dental anesthesia: causes
The most common causes of allergies to local anesthetics:
- hypersensitivity to anesthetic drugs;
- vegetative-vascular diseases;
- hereditary factor;
- incorrect dosage calculation;
- intravascular injection;
- psychoneurological disorders.
Hypersensitivity to local anesthetic drugs
In dentistry, multicomponent drugs are used for local anesthesia. The main active ingredient in them, as a rule, does not have side effects in the form of allergies, and complications are associated with excipients in the solution.
If the body is sensitive to individual components of anesthesia drugs, dentistry uses painkillers with the most simplified composition.
Second generation drugs
2nd generation antihistamines have a wider spectrum of action, practically do not cause drowsiness, and if the dosage is observed, the development of side effects is minimized. The effect of the drug lasts up to 24 hours. Not addictive. However, due to the nature of their action, they can disrupt the heart rhythm. There is a risk of developing individual intolerance. This group includes effective drugs: fenistil, claritin and histalong.
- Fenistil. Available in the form of a gel, emulsion and drops, which makes the drug universal for administration. Gel and emulsions can be applied to the skin to eliminate an allergic reaction, local cooling and anesthesia, which is especially effective for insect bites or skin itching that occurs after contact with an allergen.
- Claritin. It is considered the safest of the second generation drugs and is therefore widely used. Does not cause drowsiness or decreased concentration. Can be used by both adults and children (from 3 years old). Can be used for long-term use. Should be taken with caution in the presence of liver dysfunction.
- Gistalong. It has the longest therapeutic effect of the second generation drugs. Can be used to treat chronic allergic processes. Despite the positive qualities of the drug, it cannot be used for heart rhythm disturbances. Not recommended for children and elderly people.
How do you know if you are allergic to anesthesia?
For diagnostic purposes, a blood test for allergies to anesthesia is performed (allergy tests). This test is performed as prescribed by an allergist or dentist. The direction indicates the drugs for which the study should be carried out.
Indications for allergy testing:
- there have previously been cases of an allergic reaction to local anesthesia in dentistry;
- the patient is allergic to any drug;
- before dental treatment, if a person has symptoms such as cough, urticaria and itching of the skin, lacrimation for no known reason.
The analysis does not require preliminary preparation or adherence to the “fasting” rule. However, you should not take antihistamines before taking samples. The analysis is not carried out during periods of acute infectious diseases, exacerbation of chronic diseases, at elevated temperatures, during pregnancy and for several weeks after delivery or termination of pregnancy.
Symptoms of the disease
Drug allergies very rarely become chronic; acute reactions develop more often
Typical symptoms:
- Hives, skin rashes, itching. The red bumps disappear when pressed. Skin symptoms persist for up to a day.
- Quincke's edema.
- Attacks of bronchial asthma.
- Allergic rhinitis (runny nose).
If symptoms go away on their own or while taking antihistamines, this does not mean that you can neglect consulting a doctor. Especially if the child has developed an allergy.
The most dangerous symptom that requires emergency care is anaphylactic shock. This is the name of a condition in which muscle spasms occur, suffocation develops, and swelling of the lungs and brain appears. To eliminate the threat to life, anti-shock measures are required, which can only be carried out by qualified physicians.
When the first symptoms of a drug allergy appear, it is recommended to follow the following algorithm of actions:
- The first step is to stop using the drug. If the reaction is just beginning to develop, this may be enough to prevent complications. Next, you should carefully monitor your well-being.
- If at least one of the symptoms appears and persists for 10 minutes, then you need to take an antihistamine - any that is at hand.
- If symptoms increase, or the effect of an antihistamine is not enough to relieve allergies, you should immediately consult a doctor.
Allergy to anesthesia in children
Recently, there has been a tendency to increase the number of cases of diagnosing various types of allergies in children. When using local anesthesia in children with allergies in dentistry, there is a higher risk of developing an allergic reaction and various complications. Therefore, special attention is paid to the choice of local anesthetic for a child in dentistry.
Let's tell you how we solve this problem at the Amel Smart clinic:
- The clinic employs experienced anesthesiologists who advise and help choose the safest method of pain relief for the child;
- In addition to classical anesthesia, we use computer anesthesia and sedation in pediatric dentistry;
- a note about allergies is placed in the baby’s medical record;
- all clinic staff have been trained and are ready to provide professional emergency assistance at any time;
- Each room is equipped with a kit necessary to provide first aid for anaphylactic shock.
In most cases, dental treatment in pediatric dentistry is carried out without pain relief. But for large problems that require serious intervention, pain relief cannot be avoided. In this case, pediatric anesthesia is used, and during dental procedures, an anesthesiologist is constantly present in the office to monitor the main indicators of the child’s condition.
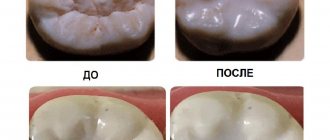
Dental treatment for allergies to anesthetics
Today, it is possible to choose the optimal method of pain relief in dentistry for each patient. In this case, many factors are taken into account: the complexity of treatment, the tendency to allergies and the presence of hypersensitivity to specific drugs, the general condition of the patient.
In the case of drug allergies, whenever possible, treatment is carried out without pain relief. For serious interventions, the doctor selects the drug for anesthesia, taking into account the patient’s existing contraindications (modern dentistry can offer a large selection of safe anesthetics). Nowadays, it is quite common practice that in dentistry, before treatment, tests are carried out for allergies to anesthesia drugs, which allow you to choose a safe solution for pain relief and eliminate the risk of complications. In rare cases, when it was not possible to select a drug for local anesthesia, dental treatment can be performed under anesthesia.
To avoid a toxic reaction, changing the anesthetic or abandoning local anesthesia is not required. The doctor uses a special needle insertion technique called a "blood test" that prevents the drug from being injected directly into the blood vessel.
In addition, Amel Smart uses hardware anesthesia, which has many advantages:
- performing different types of anesthesia;
- the most accurate dosage of the drug;
- precise determination of the injection site;
- painlessness of the procedure.
For patients with a psychosomatic reaction to anesthesia, injections of the drug are given in a lying position. If the patient is very afraid or experiences severe psychological discomfort from being in the clinic or the upcoming manipulations, he is offered treatment with sedation (medicated sleep).
Measurement of activation markers and cytokines
After antigenic stimulation, T cells express activation markers such as CD25, CD69, CD40L, CD71, HLA-Dr, which can be measured by flow cytometry or immunofluorescence using specific monoclonal antibodies. There are a few studies that mention their use for drug allergies [34, 35].
Since delayed reactions to drugs are characterized by the appearance of sensitized T lymphocytes, other methods may be used to determine the immune response:
measurement of the level of lymphocytes expressing chemokine receptors (CCR4, CCR7, CCR10) is carried out by flow cytometry and immunohistochemistry. A number of authors have shown their role in T-cell inflammation of the skin [36];
determination of cytokines IL-2, IL-5, IL-13, interferon-gamma by flow cytometry and ELISA. The authors showed the high diagnostic significance of these methods (75% and 79%, respectively) [37, 38]. Cytokines can also be determined in supernatants using the ELISpot method, which is similar to ELISA;
determination of cytotoxicity of T-lymphocytes and natural killer cells. Cytotoxic proteases (granzyme B and granulysin) are determined. Immunohistochemistry and ELISpot methods are used. Low sensitivity has been proven in patients with DRESS syndrome, but higher sensitivity in Stevens-Johnson syndrome and toxicepidermal necrolysis [39]. Some authors propose the determination of skin lymphocyte-associated antigen by cytoflowmetry [40];
determination of transcription proteins (c-maf, GATA3, T-bet, STATs, p38MARK using polymerase chain reaction and flow cytometry [41].
Currently, only genetic markers can be considered prognostic methods, as, for example, shown for some ethnic groups in relation to certain drugs (abacavir, carbamazepine, dapsone and allopurinol) [42, 43]. However, genetic correlations with allergy to LA have not yet been identified.
Thus, most of the described methods for laboratory diagnosis of drug allergy to MA, with the exception of the determination of specific IgE and IgG and BAT, are so far available only to research laboratories.
First aid for allergies to local anesthesia
If a patient experiences an allergy attack due to anesthesia, the dentist has an emergency kit in his office for such an event. It includes antihistamines, antishock drugs, antispasmodics, adrenaline, syringes, alcohol, venous catheter and tourniquet, gauze, cotton wool, saline solution. Every dental specialist has the skills to provide first aid to patients before the ambulance arrives.
Treatment of allergies to anesthetic in dentistry includes standard measures used in the treatment of allergic diseases:
- 1
Elimination of the provoking factor. - 2
Antihistamine therapy.
- 3
Preventive therapy.
Basophil Activation Test (BAT)
In recent decades, BAT has been the classic method for diagnosing allergies. Basophils and mast cells play a central role in immediate allergic reactions. DG Ebo [18] points to the increasing interest of researchers in BAT, in which the activation of these cells is measured by flow cytometry. Currently, the most commonly used basophil activation markers are CD63 and CD203c. Flow-CAST and CAST-ELISA are commercial assays based on basophil activation. CAST-ELISA determines the release of sulfodyleukotrienes activated by basophils by ELISA. The analysis is extremely slow and takes a lot of working time; its use is impractical in busy laboratory conditions.
Flow-CAST uses flow cytometry to identify basophils labeled with anti-IgE-fluorescein isothiocyanate and anti-CD63-PE, markers of activation and degranulation. Modification of Flow-CAST using anti-CD203c instead of anti-CD63 improves the performance of the study [25].
The sensitivity and specificity of BAT in allergy to muscle relaxants are reported to range from 36% to 92% and from 93% to 100%, respectively [26], and for allergy to beta-lactam antibiotics, the sensitivity ranges from 33% to 67% and the specificity from 79% to 100% [27]. The BAT method can be considered very promising for the assessment of both immediate allergic reactions and non-allergic hypersensitivity [28]. There is limited experience with the use of the BAT method for drug allergies to LA. So, N.V. Bychkova studied the reactions of 189 people (average age 37 years) to MA groups of articaine, lidocaine, mepivacaine (1:30 dilution). The least sensitization was detected in patients to drugs of the lidocaine (8%) and mepivacaine (3%) group. Among drugs in the articaine group, the frequency of positive reactions in patients varied from 41% to 18%, depending on the composition of the drug. The author concludes that the use of lidocaine, mepivacaine and articaine, which do not contain preservatives, is preferable for patients [29].
Prevention of allergic reactions: recommendations from Amel Smart specialists
To avoid unwanted reactions and complications from the use of anesthetic in dentistry, you must follow a number of rules:
- if you have an allergy to painkillers or other types of allergies, you must inform your doctor about it before starting treatment;
- information about allergies must be in the patient’s medical record;
- To diagnose intolerance to anesthetics, the dentist prescribes an anesthesia allergy test for the patient;
- Having information about the type of allergy, the doctor does not use drugs containing the allergen in the treatment of the patient;
- if premedication is necessary for patients with allergies, the anesthetic drug is combined with antihistamines, and in some cases with hormonal anti-allergy drugs.
If you suspect an allergy, it is advisable to consult an allergist before going to the dentist. Having information about intolerance to certain components, experienced doctors at the Amel Smart dental clinic will select the safest solution to the patient’s problem.
In vivo tests
To confirm allergic reactions to LA, skin tests (prick test, intradermal, application) and a dosed provocative test (careful repeated administration of the suspected drug) are used. In case of drug allergy to MA, all tests are performed in vivo
possible according to strict indications. Skin tests are recommended after 4–6 weeks. after a reaction, during remission, after discontinuation of medications. The informativeness of skin testing depends on many reasons (a reaction may develop not to the drug itself, but to its metabolite; both dermographism and skin unresponsiveness should be taken into account). These tests are simple to perform, the most cost-effective, but dangerous due to the possible development of anaphylactic reactions [9]. There are currently no certified skin test reagents available for LA allergy. Typically, in practice, standard concentrations of LA are used to conduct skin tests, which are prepared immediately before testing [10]. In our work, when examining 147 patients with anamnestic indications of LA intolerance, positive skin tests (prick tests) were detected in 8 patients (5.4%): in 5 - for articaine + epinephrine, in 2 - for lidocaine, in 1 - on mepivacaine. When performing skin tests, the development of symptoms of urticaria and bronchospasm of moderate severity was noted in 1 patient after administration of a combined drug containing articaine + epinephrine.
To diagnose an allergy to LA, the in vivo
, proposed by academician A.D.
Ado [11]. The advantage of the method lies in the study of the allergic reaction in situ
.
Subsequently, we applied this principle in the development of microprovocation tests with MA with the determination of tryptase, eosinophilic cationic protein and myeloperoxidase in saliva [12]. The indicated mediators in saliva before and after provocation were studied using standard methods using immunochemiluminescence and enzyme-linked immunosorbent assay (ELISA). This made it possible to differentiate different types of immune response to MA in a minimally invasive way. in vivo
tests are dangerous and can be used in unavoidable cases [13].
Clinical blood test.
An increase in blood eosinophils over 5% is diagnostically significant. However, in the case of LA intolerance, eosinophilia is extremely rare, and more often it is combined with a concomitant atopic constitution and allergies to non-infectious allergens (inhalation, food). Some doctors try to correlate the increase in the number of peripheral blood leukocytes with allergic reactions to the drug, but such an increase can be caused by other reasons [14].
In vitro tests
The choice of test depends on the suspected mechanism and time since the onset of the allergic reaction [15]. Laboratory diagnosis of drug allergies includes diagnostic and prognostic methods. A position paper from the European Academy of Allergy and Clinical Immunology reviews the most appropriate diagnostic tests for allergic reactions to drugs [16]. in vitro diagnostic tests
for immediate-type allergic reactions in the acute phase, preference is given to the determination of tryptase and histamine; for reactions in the long-term period, various methods for determining specific IgE and the basophil activation test (BAT), performed by flow cytometry. To confirm delayed-type RLH, the following laboratory methods are recommended: lymphocyte transformation test; determination of interleukins IL-5, IL-2, IL-4 or granzyme by ELISA, ELISpot (Enzyme-Linked ImmunoSpot), multiplex analysis, combination of determination of cytokines and cytotoxicity markers. Prognostic methods include determination of HLA markers.
Determination of tryptase
mast cells confirms their degranulation. Tryptase levels may rise within 24 hours after the onset of an acute allergic reaction (usually within 30–120 minutes). The test is highly sensitive but nonspecific [17].
Histamine release test
detects the release of histamine in response to allergen stimulation. However, histamine levels decrease quickly (within half an hour) after an allergic reaction develops, so this test is used for research purposes only.
Determination of methylhistamine
in urine. N-methylhistamine is a stable metabolite of histamine and is detected in urine. It is an indicator of mast cell degranulation during an acute allergic reaction. It is important to evaluate renal function to interpret the results. However, approval for clinical use of this test was recently withdrawn [18].
Determination of anaphylatoxins
(C3a, C4a, C5a) are carried out when acute allergic reactions are suspected; they serve as markers of activation of the complement system. Their research is of particular value in situations where the inflammatory process occurs without the participation of IgE antibodies. However, this method is rarely used in routine practice.