Like any part of our body, our gums can also become injured. The tactics of the planned treatment depend on the volume and nature of the damage received. Only with properly organized treatment will trauma to the gums not leave serious consequences. When any oral disease appears without the necessary treatment, manifestations of a weakened body and complications are possible.
Despite the fact that the gums are protected from the outside by the muscle tissue of the lips, they are easily exposed when talking, eating, or laughing. This is facilitated by the fact that facial muscles in humans are quite well developed. Therefore, gums can easily suffer injuries of varying severity.
Content:
- Causes
- How does pathology manifest itself?
- How is the treatment carried out?
- Surgical techniques
- Additional treatments
- Preventive measures
If the gums have become detached from a wisdom tooth or any other unit, you need to visit a doctor as soon as possible.
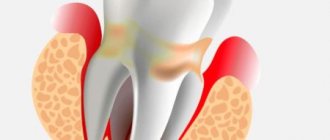
When the soft tissues subside, the neck remains unprotected and exposed. It is not covered with a thick layer of enamel, so it immediately begins to react sharply to temperature changes. The situation is aggravated by the fact that food debris gets into the formed periodontal pocket. They accumulate there and serve as an ideal breeding ground for pathogens. If such a pocket is not cleaned in a timely manner, it will increase in size. Then it will come to edentia.
Causes
Exposed necks indicate periodontal damage. Most often the problem occurs for the following reasons:
- Genetic predisposition. When exposed to this factor, a person can very diligently monitor the health of his smile, but will still periodically encounter unpleasant dental symptoms.
- Mechanical and thermal damage. The habit of gnawing on foreign objects, eating too hot food, using a hard brush are all provocateurs that contribute to irritation.
- Poor oral hygiene. If the patient neglects basic hygiene rules, a lot of plaque is deposited on the crowns. Pathogenic microorganisms spread in it. The gums become irritated, turn red, and bleed. Gradually they begin to move away from the teeth. It is important to use a brush and paste twice a day, and undergo professional hygiene at the dentist’s office annually.
- Poorly performed prosthetics or mistakes made during filling. It is necessary that the dentures fit as tightly as possible to the bases and do not fall under pressure, otherwise the gums will be constantly injured and inflamed.
- Curvature of the bite, problems with teething “eights”, uneven edges of the crowns. All this causes the gums to move away from the tooth.
- Unbalanced diet. If a person eats only soft foods and sweets, he does not actively chew food. As a result, blood circulation in the oral tissues slows down, less saliva is released, and periodontal deposits are actively formed. These are the prerequisites for a recession.
- A large amount of tartar. Despite the fact that dentists recommend removing stones annually or even more often, many patients do this very rarely. You shouldn't wait until a serious problem arises. It is easier and cheaper to prevent it than to treat it later.
- Hormonal imbalance. Most often, this reason concerns women, for example, during pregnancy, menopause, and breastfeeding. With hormonal fluctuations, the mucous membranes become especially vulnerable. Even minor mechanical impacts cause recession.
Don't forget about the negative effects of tobacco smoke. According to statistics, smokers are much more likely to suffer from gum disease and exposed necks. They accumulate plaque faster. Therefore, if you want to have a healthy smile and visit the dentist less often, stop smoking.
Mucosal injury
For any person, the cause of pain in the mouth can be ordinary injuries.
Trauma is often the cause of mouth pain.
For example:
- eating something too hot/cold. This injures the mucous membrane, and pain quickly appears in it. Inflammation indicates the presence of injury to the mucosa, caused by temperature exposure, and at the same time incompatible with its integrity. Eating something very hot can cause injury to both the palate and the tongue, as well as the throat;
- rough food, which can leave scratches on the roof of your mouth and on the inside of your cheeks. This causes pain and burning to appear after a day or two;
- A child has more ways to damage his or her mucous membrane than an adult. The baby can scratch it with his thin nail or put something in his mouth, for example, a toy. And if the child is somewhat older, his mucous membrane can be damaged by lollipops and chips.
When choosing a remedy for pain, it is very important to pay attention to the nature of the injury:
- in case of a burn, it is useful to rinse your mouth with warm water and then use Metrogil Denta dental ointment;
"Metrogil Denta"
- In case of mechanical damage, it is recommended to immediately use antiseptics by rinsing your mouth with them. For an adult, it is useful to rinse your mouth with a mixture: 10-15 drops of 3% hydrogen peroxide per glass of water. Decoctions of calendula and chamomile are also good. Also good are the drugs “Rotokan” and “Miramistin”, which fight infection as well as inflammation.
"Miramistin"
The main rule: no self-medication! Therapy must be prescribed by a specialist. Otherwise, you can make the situation even worse. So if symptoms appear, it is recommended to visit a doctor. He will prescribe the best treatment for a particular situation.
How does pathology manifest itself?
Symptoms depend on how far the gum has receded from the tooth. Most often patients complain of:
- increased bleeding and soreness of the gums;
- bad breath that cannot be eliminated with standard hygiene products;
- taste of pus;
- separation of purulent masses from the inflammatory focus;
- the appearance of deep periodontal pockets;
- loosening of individual units.
In the first days of the disease, patients may not experience any significant discomfort. They are just beginning to notice that in certain areas of the jaw the tissue seems to have sagged and become less voluminous. Because of this, the crown part of the tooth, on the contrary, looks elongated.
If the gums have peeled off, there is no need to try to do anything on your own. Without qualified help, it will still not be possible to cope with the recession. Postponing competent therapy until later is fraught with even more serious violations.
Treatment options
The mucous membrane is very sensitive, so smearing wounds on the gums with iodine and brilliant green is strictly prohibited to avoid getting burned.
Medicines
To treat wounds in the oral cavity, special ointments are used that have an antiseptic effect: Solcoseryl, Metrogyl Denta, Apident. These drugs contain components that eliminate pathogenic microflora.
If a scratch causes pain, special ointments are used to relieve pain and strengthen the gums.
In addition to gels, it is recommended to rinse with the following solutions:
- Chlorhexidine - to clean the wound and protect against germs.
- Miramistin - to prevent infection with fungi leading to stomatitis.
- Hexoral, which contains levomenthol and hexetidine, which have an antiseptic effect.
- Hydrogen peroxide, which cleanses the scratch from dirt and stops the spread of inflammation.
If a white scratch is discovered, indicating suppuration, you cannot do without the help of a dentist, since you will have to open the wound. The doctor will remove any accumulated fluid and treat the cut with antibiotics. If a child has damaged the gums, one of the following antiseptics intended for children will help:
- Cholisal - for children after one year, promotes rapid restoration of damaged tissues, relieves pain.
- Kamistad is an ointment consisting of natural chamomile oil, intended for healing scratches.
- Dentinox-N is used not only for teething, but also for suppuration, redness and burning of the gums.
- Kalgel is an antibiotic that cleanses the wound and stops suppuration.
- Glycerol - used to moisturize and soften the damaged area, as well as to prevent the appearance of scars.
It is recommended that every mother have these medications in her medicine cabinet in order to promptly lubricate the scratch and protect the child from infection. Any of these drugs are lubricated on the gums 2-3 times a day. In this case, it is necessary to observe how the baby tolerates the effect of the medicine, whether there is an allergic reaction.
ethnoscience
Having scratched the gum, you need to immediately begin treatment to prevent inflammation. To do this, you can use folk remedies based on medicinal herbs.
You can quickly and easily get rid of redness and burning using the following formulations:
- 1 tsp tincture of calendula diluted in 200 ml of water - used to rinse wounds, and also used as a compress;
- propolis lozenges for application to the inflamed area of the gum;
- decoction of chamomile and sage, for the preparation of which 1 tsp. dry herbs pour a glass of warm water. This natural antiseptic helps get rid of purulent contents.
In order for the treatment to give the fastest possible effect, you should limit the intake of solid foods, exclude hot seasonings and sour pickled foods from the diet.
By choosing the right oral hygiene products, you can reduce the risk of scratches on your gums. Quitting smoking and strengthening the immune system will help the body fight off any infection. In summer, it is advisable to include more vegetables and fruits in your diet, and take more walks in the fresh air. In winter, it is recommended to drink a vitamin complex to increase immunity.
How is the treatment carried out?
Some people think that they can be cured with regular rinses. Unfortunately, it is not. The first step is to make an appointment with a dental hygienist. The doctor removes soft and hard deposits from the surface of the crowns and subgingival area in one session.
The following methods are used to remove stone:
- Instrumental. Involves the use of special scrapers that remove deposits. It is considered outdated and is extremely rarely used by doctors, as it is traumatic.
- Ultrasonic. Using an ultrasonic scaler, the doctor crushes the stones into tiny particles. This equipment produces waves of the required frequency, which easily destroy dental plaque.
- Sandblasting. It is the most modern and safe. The doctor delivers the cleaning solution under high pressure. Abrasive particles wash away deposits from crowns and effectively flush out existing pockets. The advantage of the technique is to achieve the effect of teeth whitening by one or two shades.
If the hygiene procedure does not help and the problem is serious, the patient is prescribed surgical treatment.
Surgical techniques
In advanced situations, plaque removal alone is not enough. Then there may be a need for open or closed curettage. It is indicated if the gums are very severely detached from the dental neck and the bone structure is changed.
The dentist-surgeon treats the lesion with an antiseptic, makes a small incision and removes purulent deposits and affected tissue . Then the gum is sutured. All manipulations are performed under local anesthesia. This means that the patient is conscious and can communicate with the doctor, but does not feel pain.
For a speedy recovery after curettage, antibiotics and mouth rinsing with an anti-inflammatory solution are prescribed. If the pain after surgery is very severe, the patient can use painkillers.
First aid for stomatitis
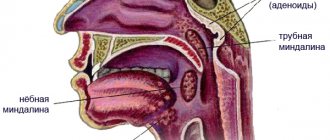
The most common cause of pain in the oral cavity is stomatitis.
Note! All of the medications listed are suitable only for relieving pain, but not for treating stomatitis itself. So you should still contact the dentist as soon as the opportunity arises.
The doctor will prescribe a comprehensive treatment for pathologies
The hospital uses complex treatment. This includes physiotherapy, as well as the following types of medications:
- anti-inflammatory;
- antibacterial;
- antiviral;
- proteolytic enzymes.
To alleviate the symptoms of this disease at home, painkillers are useful, as well as mouth rinses to get rid of inflammation.
It is also useful to use painkillers at home:
- How to rinse your mouth for stomatitis in adults
- "Analgin";
- "Tempalgin";
- "Panadol";
- paracetamol;
- aspirin.
Important ! The latter is also good as a means to combat inflammation.
To relieve discomfort, it is recommended to use painkillers
Additional treatments
Considering that gums become inflamed for various reasons, it is important to try to find out the provoking factor. Then the risk of relapse of dental pathology can be reduced to a minimum.
If the doctor determines that the disorder is related to hormonal levels, it is necessary to select hormonal therapy . In case of malocclusion, consultation with an orthodontist is indicated. If the diet is unbalanced, the patient is told what the diet should be like after recovery.
Often, when fighting gum that has receded from a tooth, anti-inflammatory drugs, immunomodulators, glucocorticosteroids, and antiseptics are used. It is very important that the patient strictly follows all medical prescriptions and does not engage in amateur activities. An integrated and responsible approach to treating recession is a guarantee of a speedy recovery.
If the tissues become so inflamed that the teeth begin to loosen, splinting may be required. If there is a deficiency of bone tissue, their deficiency is compensated with special compounds.
Gum abscess - symptoms and treatment
Gum abscess is caused by pathogens of the oral microflora, which is mainly represented by the following bacteria:
- Bacteroides forsythus (in 55.6% of cases);
- Porphyromonas gingivalis (50.0%);
- Fusobacterium nucleatum (44.4%),
- A. actinomycetemcomitans (38.9%);
- Prevotella intermedia (38.9%) and others.
In addition, in most cases, periodontal pathogens enter into symbiosis with fungi of the genus Candida (44.4%), bacteria Enterobacter (38.9%), Streptococcus intermedius (13.2%), Peptostreptococcus micros (13.2%) and Staphylococcus aureus (28.5%) [4].
The pathogenesis of the disease varies depending on the location of the inflammation.
1. An abscess that arises as a result of pathological processes in periodontal tissues. Inadequate treatment of tooth root canals leads to acute inflammation or exacerbation of its chronic form in the periodontal area. As a result, the number of microorganisms in the tooth root canal and in the periodontal area increases significantly. In response to this, granulation tissue (connective tissue formed during healing) grows in the area of the root apex, replacing bone tissue with it. At the moment of exacerbation of the process, foci of purulent melting of granulation tissue appear in this area. As a result of periodic exacerbation of the inflammatory process, the periodontal lesion gradually spreads to more and more new areas of the bone, mainly towards the vestibule of the oral cavity. This leads to the appearance of vertical slit-like defects of the cortical plate and the further development of first infiltration in the gum area, and then the appearance of an abscess [5].
2. An abscess that has arisen in the area of the periodontal pocket. Periodontal gum abscess occurs as a result of several interrelated pathological processes. A large amount of supra- and subgingival dental plaque promotes the development of periodontal pathogenic bacteria, which causes a strong immune reaction. The body responds by forming an infiltrate with a large number of immune system cells. These cells produce inflammatory mediators that stimulate the destruction of bone tissue by osteoclasts (cells that remove bone tissue by dissolving mineral content and breaking down collagen). The bone tissue begins to dissolve and a periodontal pocket is formed, which, depending on the severity of periodontitis, has different depths. At the time of exacerbation of periodontitis, suppuration from the periodontal pocket becomes continuous. If the outflow is disrupted, abscess formation occurs [6].
3. An abscess that has arisen in the area of peri-implant tissue. The cause of the development of peri-implantitis is microorganisms located in the biofilm on the surface of the structure. Colonies of microorganisms affect the soft tissue surrounding the implant, causing inflammation. Further, the process develops in the same way as with periodontitis, but does not remain localized, but spreads towards the apex of the implant. In peri-implantitis, the inflammatory infiltrate passes directly to the alveolar bone, while in periodontitis it is separated from the bone by a one-millimeter layer of connective tissue. At the early stage of peri-implantitis, an abscess occurs at the level of the upper third of the implant - in the area of the peri-implant pocket. At later stages, as the bone in the area of the implant body is destroyed, it can move closer to the transitional fold of the gums[7].
Preventive measures
To prevent gums from moving away from the tooth, you need to follow simple recommendations:
- brush your teeth twice a day;
- use a properly selected brush and paste;
- visit the dentist in a timely manner;
- prevent tartar from forming;
- no smoking;
- eat more solid foods;
- Healthy food.
At the first sign of a recession, you should see a doctor. Then the disease can be stopped very quickly.
How to treat?
Before choosing a course of treatment for stomatitis, the specialist finds out where this pathology came from in this case. To save a patient, for example, from catarrhal stomatitis, tartar is removed, teeth are treated and filled. To relieve him of ulcerative stomatitis, the doctor conducts a thorough examination of the body for problems with the blood, gastrointestinal tract, heart and blood vessels. And with aphthous stomatitis, the sick person is examined for allergies and rheumatism.
The course of therapy depends on the nature of the pathology
Along with treating the disease, the specialist prescribes local therapy, which means rinsing the mouth with chlorhexidine - 0.05% or 1% solution. The following drugs are also used when rinsing:
- aminocaproic acid;
- herbal decoctions;
- methylene blue.
A gentle diet will help speed up treatment.
Here are the foods to avoid:
- spicy;
- roast;
- rough food.
Here are some things you should increase your consumption of:
- porridge;
- pureed soups;
- vitamins (special emphasis on A and C).
Important ! After eating, you should rinse your mouth thoroughly. First with clean warm water, then with medicine.
After eating you need to rinse your mouth
Treatment for stomatitis usually takes from five days to one and a half weeks. But if the disease is started, it will last longer, becoming more and more severe.