The problem occurs several weeks before the eruption of a baby or permanent tooth. The appearance of a cyst is indicated by a bluish-purple spot (hematoma). This is due to difficulty in tooth eruption.
An eruption cyst is a type of soft tissue benign tumor that appears when a tooth has already begun to erupt through the gum. Scientists and doctors have not agreed on why it occurs. The most likely causes: infection, trauma, improper development of teeth, which causes a lack of space for the “newbie”. In addition, it may be a consequence of caries and improper care.
Eruption cysts occur during the growth of baby teeth or, more often, at 6–9 years of age, when permanent teeth emerge. The fact is that, due to its anatomical structure and location, the chewing group of teeth is the most difficult to erupt.
If you notice a large formation in your baby’s mouth, in the place where a tooth should appear, consult a doctor. Do not resort to self-medication under any circumstances. Infusions, rinses and even strong antibiotics most likely will not help, but ruining a child’s health in this way will cause serious harm.
If you contact a specialist, treatment can follow one of two scenarios. In the most favorable option, the doctor will advise giving the child toys, special teethers, crackers - everything that the baby can chew. This will help break through the mucous membrane.
In difficult situations, surgery may be necessary. Then the surgeon will cut the gum under local anesthesia. This will make teething easier.
It is forbidden to try to cut or tear the mucous membrane on your own; you can cause a serious infection or injure your baby.
How does a tooth root cyst appear?
The causes of cysts are varied, and among them it is impossible to single out the prevailing ones. So, this may be the result of physical trauma to the maxillofacial bones, or a rare but common medical error, in which the tightness of the root canal was broken, which became the basis for the emergence of a source of infection. A similar situation occurs when a dental crown is installed incorrectly. But the reasons for cyst formation are not limited to this. Untreated infectious diseases (in particular, sinusitis or periodontitis) are no less a provoking factor.
What will happen if left untreated?
Ignoring the symptoms of the disease leads to dangerous consequences for health. Thus, the patient may encounter:
- destruction of roots, their strong loosening;
- jaw fracture;
- tumor formation;
- purulent abscess;
- periostat;
- osteomyelitis.
The disease can cause the development of sepsis. This is a very serious condition in which the infection enters the blood and quickly spreads throughout the body.
Classification of dental cysts
There are not many types of cysts, so understanding them is not difficult. Four main types are distinguished by location:
- wisdom tooth cyst;
— a cyst due to an illiterate (unprofessional) installed dental crown;
- a cyst that arose as a result of the influence of a third-party infectious disease (sinusitis);
- a cyst localized in the area of the front teeth.
At the same time, a classification is used based on previous circumstances preceding the occurrence of the cyst:
- a disease caused by poor-quality removal of one or more teeth;
— periodontal type cyst, provoked by an inflammatory process in the gums;
- a cyst caused by the growth of a wisdom tooth (retromolar or paradental);
- a cyst that occurs in children, first during the period of the appearance of milk (follicular) teeth, and then molars (eruption cyst);
— a cyst that arose as a complication of periodontitis (radicular);
— a situation is also possible in which the tissue forming the tooth degenerates (keratocyst).
What to prepare for after removal: what is considered normal, and when to urgently see a doctor
In order to prevent the development of dangerous situations after tooth extraction, you need to notice alarming signs, and even if they are mild, consult a doctor in time - this way you will avoid serious complications. This may be alveolitis, fistula, nerve damage and other pathologies. They cannot be stopped or cured at home.
In the table, we have listed the symptoms and explained in which cases they should alert you, and when the situation remains within the normal range.
What to prepare for after removal
| Symptom | Norm | Threat: You need to see a doctor |
| The gums are painful and swollen, the cheek is swollen and blue | Swelling and hematomas (bruises) are a natural reaction to injury, especially if the removal was difficult. They can intensify for up to 3 days, and then begin to subside | Does not go away for more than 4 days, gets worse or appears after sleeping - a feeling that the cheek is “blowing” |
| The wound is bleeding | Bleeding stops within the first hour after surgery. Further minor and rare discharge is possible | If the blood flows heavily for several hours or bleeding starts again at home - it is the abundance of discharge that should alert you |
| Presence of a blood globule in the socket | A dark red clot begins to form immediately after removal, fills the entire hole, and persists for up to 5-7 days | The hole is empty, “dry”, deep, a yellowish-grayish coating has appeared, there is an unpleasant putrefactive smell - this situation is called a “dry hole” |
| A white coating appeared on the wound | A whitish film appears on days 2-3 - this is the release of fibrin (a protein involved in tissue healing) | Yellow, greenish or dark gray color, as well as bad odor, redness and pain indicate the development of an infection |
| Discharge from the socket | Ichor is a clear liquid that can ooze from the wound in the first day | Cloudy pus with a putrid odor indicates an infectious process |
| The temperature has risen | Within two days (usually in the late afternoon) body temperature can rise to 38-39⁰С | The fever is severe, the temperature stays above 38⁰C for more than 2 days in a row or rises again after the condition has returned to normal |
| It is impossible to open your mouth wide, there is jaw clicking | It mainly happens after the removal of large teeth – molars, wisdom teeth. Symptoms may persist for up to 3 days (for complex operations - up to 7 days), then gradually subside | Difficulty opening the mouth persists for longer than 4 days, there are no positive changes, the pain intensifies |
| Pain at the site of the extracted tooth | Aching or pulsating - may be on days 1-3, but fades away every day | Lasts longer than 3 days or intensifies every day, spreads across the face, extends to the ear, neck |
| Part of the gum and cheek are numb | Normal for several hours after surgery - anesthesia continues to work | If the tissues have lost sensitivity for more than a day, the nerves may have been affected. Need to see a doctor |
| Running nose | Not the norm! Pain when blowing your nose and breathing, liquid discharge and runny nose are a symptom of complications during surgery | |
Diagnosis of symptoms of tooth root cyst
The appearance of a cyst implies the formation of a cavity, which gradually grows while simultaneously filling with pus. This condition can last for a long time, and the patient does not experience pain. A sign suggesting the presence of a cyst is slight pain that occurs when pressing on the gum. Such a symptom only in rare cases becomes a reason to visit a dentist. Basically, it occurs in later stages, when the pain intensifies and becomes nagging, continuous, cannot be relieved with analgesics, and inflammation begins to additionally manifest itself in the form of swelling and swelling of the gums in combination with a persistent unpleasant odor in the oral cavity. Finally, a situation cannot be ruled out in which a fistula occurs - that is, a channel through which the contents of the cavity independently come out.
An effective way to detect a cyst in a timely manner is to conduct an X-ray examination followed by its opening and removal.
It should be noted that at the very beginning the disease poses minimal danger to surrounding tissues, since the cavity itself is reliably isolated by thick walls. However, as pus accumulates, the pressure on the walls increases, creating the possibility of a breakthrough, which can lead to blood poisoning and, in the long term, damage to the structure of the jaw bones. At the same time, the dynamics of cyst development are unpredictable and strictly individual. However, in the presence of other inflammatory processes or infections, in a weakened body the transition to the acute stage can occur quickly.
Particular attention should be paid to early diagnosis of the disease in pregnant women. This is due to the complexity of treatment: during pregnancy, only stabilization of the cyst is possible. If the inflammatory process worsens, the choice of treatment methods is strictly limited. That is why, at the planning stage of pregnancy, it is necessary to undergo a full examination by a dentist.
Why does it occur
Among the main causes of pathology:
- advanced caries;
- jaw injuries;
- illiterate root canal treatment;
- overload of individual units as a result of poorly performed prosthetics;
- congenital anomalies of the upper/lower jaw;
- infections of the nasopharynx and oral cavity.
Regardless of the characteristics of the provoking factor, a gum cyst should be treated under the supervision of a dentist. Self-medication for this diagnosis is unacceptable.
Tooth root cyst in children
The disease has features and varieties that are characteristic strictly for children. First of all, we are talking about formations that arise and go away on their own, without complications: in the form of a rash that appears on the gums, as well as the so-called “Epstein’s pearl”. Both varieties do not pose a danger due to the absence of purulent masses, which means that the cavity is infected. In addition, they may not occur at all, being only some of the phenomena accompanying the development of the child.
The situation is different with the appearance of a cyst during the growth of teeth (both milk and molars). In this case, the resulting cavities are infected, and given the previously described asymptomatic nature of the disease in the early stages, the most reliable method of determining its presence is regular visits to the doctor. This allows for successful treatment at the very beginning of the development of the cyst, saving the tooth in almost 100 percent of cases.
General recommendations after surgery
On the first or second day after tooth extraction, you want to lie down and sleep - this is the body’s natural reaction to the stress experienced. After the release of stress hormones - adrenaline and cortisol - stabilization and rest are needed. Don't deny yourself this.
However, there are recommendations regarding sleep: you should raise the pillow higher and sleep reclining so that your head is elevated. This will prevent unnecessary pressure on the jaw and cause bleeding. To increase the inclination of the bed, place a pillow under the mattress or use two pillows.
Otherwise, maintain a calm regime without physical overload, pressure surges and overheating. That is, for the first time it is better to refuse air travel, hard work, playing sports and lifting weights, visiting the pool, bathhouse or sauna. You should not take a hot bath (a short warm shower would be preferable) and stay in the sun for a long time or sunbathe in a solarium. All this increases blood pressure, which is fraught with new bleeding. It is ideal if you have a couple of days off to recover after your teeth are removed.
Methods for treating dental cysts
As mentioned earlier, the only reliable and error-free method for diagnosing a cyst on the root of a tooth is an x-ray. In most cases, one x-ray is sufficient; however, due to individual tooth growth patterns, an additional x-ray of the root portion may be required.
Based on the analysis of X-ray data, the dentist determines and prescribes the type of treatment. Due to the difficulty of accessing the cavity, the process of getting rid of the cyst can take several sessions - however, only this method allows you to eliminate the pathology while keeping the tooth itself healthy.
There are two main directions of treatment: therapeutic and surgical.
— the sequence of actions during therapeutic treatment is as follows: the dentist gains access to the intradental canals (to do this, the tooth tissue is opened), expands them, cleans the cavity from pus, then disinfects it and installs a temporary filling. In the absence of relapse and a favorable outcome, the temporary filling is replaced with a permanent one. An alternative option may be the depophoresis method. Its difference is that the cleaning of the canals occurs due to the sequential introduction of a special substance into them, which, under the influence of an electric current, disinfects them. The common property of both methods is their applicability in the early stages of the disease;
— surgical intervention is used in most cases due to its reliability and high efficiency. There are three types of surgical treatment: cystectomy, hemisection and cystotomy. The first option involves opening the gum from the side and removing the cyst, followed by suturing. Rehabilitation takes place while taking antibiotics. Hemisection requires additional removal of the affected tooth root and crown fragment. If a cystotomy is prescribed, penetration into the cavity is carried out through the near wall. This method has a significant rehabilitation period.
In addition to the above methods, laser therapy is used. Its principle of operation is to insert a thin tube into the cyst, allowing complete disinfection using a laser, followed by vacuum cleaning. This progressive method is painless and effective, since it is guaranteed to preserve the tooth and protect against recurrence of pathology.
Reasons for the appearance of a purulent sac on the gum -
Let's now take a closer look at what exactly causes purulent inflammation at the root of the tooth, which becomes the cause of the appearance of a purulent abscess on the gum.
- Untreated caries and pulpitis – untreated caries leads to the development of inflammation of the dental pulp (neurovascular bundle located inside the tooth crown and root canals). Dentists call inflammation of the pulp the term pulpitis. In the absence of its timely treatment, apical periodontitis, in turn, occurs, in which a purulent focus of inflammation forms at the apex of the tooth root - let's call it a “purulent periodontal abscess” (Fig. 4).
Pus from such an abscess seeks a way out - as a result, a fistula tract is formed in the bone tissue, through which the pus penetrates first under the periosteum, and then under the mucous membrane (24stoma.ru). As a result, a pus-filled “cyst” appears on the gum, looking like a purulent sac or a purulent lump on the gum (Fig. 5a, b). In this case, treatment of a cyst on the gum will require opening the causative tooth, removing the nerve, treating the source of inflammation at the apex of the tooth root - followed by filling the root canals.
Read more about the treatment of apical periodontitis in the article: → Treatment of inflammation at the apex of the tooth root
- Poorly filled root canals – treatment of diseases such as pulpitis and periodontitis involves filling the root canals in the tooth. But when filling root canals, dentists often make mistakes. For example, according to official statistics alone, root canal filling is performed poorly in at least 60-70% of cases. The main mistake dentists make when filling root canals is that the canals are not filled to the top of the tooth root.
As a result, an infection develops in the unfilled part of the root canals, which causes inflammation to develop at the apex of the tooth root (i.e., apical periodontitis develops again). If a significant amount of pus forms in this focus of inflammation, which can happen during an exacerbation of the inflammatory process against the background of hypothermia, the pus seeks a way out, which can lead to its release under the mucous membrane. Which again will look like a cyst or purulent sac on the gum.→ In Fig. 6-7 you can see poorly filled root canals. Unfilled parts of the canals are marked with white arrows. Black arrows mark the boundaries of the focus of inflammation at the apex of the tooth root (on x-ray, the focus of inflammation looks like intense darkening). → In Fig. 8 you can see the well-filled root canals of the three lower incisors. Black arrows mark the tops of the roots of the teeth, up to which the canals should be filled. We have attached this photo specifically so that you can see how root canals should be filled normally.
How the treatment is carried out - the treatment in this case will consist of unsealing poorly filled root canals, after which the standard treatment of the inflammation at the apex of the tooth root is then carried out (i.e. standard treatment of apical periodontitis). You can read more about this treatment using the link above.
- The appearance of a cyst due to tooth perforation – when filling root canals or when installing pins, dentists often make another mistake - they perforate the wall of the root canal, making a “hole” in the root of the tooth. In Fig. 9-10 you can see how the dentist in both cases brought the pin directly into the bone tissue. As a result, inflammation (periodontal abscess) developed at the site of the perforation, which on an x-ray looks like intense darkening, limited for convenience by black arrows.
Treatment of perforations is a big problem in dentistry, and besides, it cannot be carried out in all cases (for example, teeth such as those in the radiographs above will have to be removed). If small perforations occur, they can be filled with special materials, for example Pro-Ruth material. Such materials are very expensive, but, of course, if you go to the same clinic where this happened to you, you should receive treatment for free, or pay for the cost of dental implantation.
- Gum cyst due to periodontitis – such a cyst in professional language is called “periodontal abscess”. In this case, a purulent abscess under the mucous membrane of the gums is formed in the projection of a deep periodontal pocket, which can form along the tooth root with local or generalized form of periodontitis. Usually, pus from the periodontal pocket is released into the oral cavity along the surface of the root, but if the pocket becomes very deep, the outflow of pus may be disrupted.
If the outflow of pus is disrupted in the projection of the periodontal pocket, a purulent abscess occurs, i.e. the same purulent sac. In the photo below you can see such a periodontal abscess in the projection of the distal root of the 6th lower tooth. On an x-ray of this tooth we see a deep periodontal pocket (to the entire depth of the tooth root). To treat this pathology, it will be necessary to open the purulent abscess and further treatment of periodontitis by a periodontist.Purulent abscess on the gum with local periodontitis -
Rehabilitation period and prevention of dental cysts
Due to the fact that the cyst is an inflammatory infectious process, drug therapy necessarily includes taking antibiotics, which are selected by the attending physician. Vitamin complexes and immunomodulators act as compensating medications. Treatment of dental cysts with medications is carried out simultaneously with removal of the cyst.
The main ways to avoid the disease are to regularly visit the dentist and carefully monitor oral hygiene. For preventive purposes, you can periodically rinse with infusions and decoctions - for example, aloe, calendula, sage. Combined with strict adherence to the dentist’s recommendations and timely relief from chronic nasopharyngeal diseases, this will ensure dental health for years to come.
You also need to clearly understand that a cyst on the root of a tooth is one of the serious and complex diseases, the treatment of which requires time and highly qualified surgeons. Only this guarantees the absence of complications: re-infection, the occurrence of an abscess, pulpitis or fistula, damage to adjacent tissues and teeth.
What is a cyst on the gum?
We have already said above that there is such a disease as apical periodontitis, in which a focus of inflammation forms at the apex of the tooth root. Most often, periodontitis has a sluggish chronic course (often almost asymptomatic), and only against the background of decreased immunity or hypothermia does inflammation worsen. With such an exacerbation, pus begins to actively form at the apex of the tooth root, i.e. A purulent abscess forms in the bone around the apex of the tooth root.
The pressure in the focus of purulent inflammation is increased, so the pus seeks a way out, spreading through the bone tissue. It first penetrates under the periosteum located on the surface of the jaw, and during this period there is only limited, extremely painful swelling on the gum. The next stage is when the pus penetrates through the periosteum under the mucous membrane of the gums. Those. gum cyst – is essentially a purulent abscess formed between the periosteum of the jaw and the mucous membrane of the gums. Because The mucous membrane is elastic, it really looks like a bag filled with pus, soft to the touch.
It should be noted that such a purulent sac can form on the gum not only on the front side of the alveolar process of the jaw (i.e. in front of the teeth), but also, for example, on the side of the palate. Moreover, if this is an ordinary leak of pus under the mucous membrane against the background of apical periodontitis, such a purulent abscess will still look like a small limited swelling, soft to the touch. But occasionally you can encounter other situations when a soft-to-touch swelling deforms a significant area of the gum.
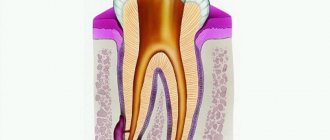
What else can a cyst on the gum look like?
Such deformation of the palate as in the photo above is associated in this case with the formation of a very large root cyst in one of the upper incisors. Such cysts form at the apex of the tooth root in the absence of timely treatment of apical periodontitis. A cyst is a cavity in the bone tissue of the jaw, lined from the inside with a dense fibrous membrane and filled with pus. Cysts grow slowly, and when the growing cyst reaches the oral mucosa, it displaces the gum mucosa.
Variants of the outcome of inflammation - in most cases, purulent melting of the mucous membrane occurs, and pus exits through the formed fistula opening. In this case, after some time, the fistula may close, which will indicate a temporary subsidence of the inflammatory process at the apex of the tooth root, or purulent discharge may leak from the fistula into the oral cavity for a long time. As for the outcome with a root cyst, in this case there cannot be a breakthrough of pus through the mucous membrane, because root cysts have their own fibrous membrane.
X-ray diagnostics –
As we said above, the final diagnosis can only be made using an x-ray, on which a cavity formation in bone tissue will always look like a rounded darkening.
In the x-ray images below we have presented you with 3 options for localizing root cysts. The most common location is root cysts at the apex of the tooth root, but cysts on the lateral surface of the root or located between the roots of multi-rooted teeth are much less common. Radiographs of root cysts of different locations –