Angioedema (other names: Quincke's edema, giant urticaria, acute angioedema) is trophoneurotic edema. The disease may be hereditary or acquired. It is characterized by the appearance of swelling of the subcutaneous fatty tissue and deep layers of the skin, including the mucous membranes of all organs and systems (digestive, respiratory, urinary, etc.). Angioedema may disappear within 72 hours.
The disease can have a hereditary form (about 25% of all cases). The idiopathic variant occurs in approximately 30%: in this case, it is not always possible to establish the true cause of the disease. In all remaining cases, Quincke's edema occurs with drug allergies, insect bites, food allergies, helminths and protozoa, autoimmune diseases and blood diseases.
In some cases, swelling is also called huge urticaria. According to statistics, Quincke's edema occurs in both adults and children, but in most cases the disease occurs in women at a young age. It is observed less frequently in older people and children. This problem occurs at least once in a lifetime in 10% of the population.
When a specific allergen enters the body, a strong allergic reaction occurs, in response to which Quincke's edema and other allergic diseases develop. Concomitant diseases may be bronchial asthma, food allergies, and the causes may be urticaria or hay fever, if they are not treated at the proper level.
In patients with pseudoallergic edema, the body can react quickly to the compliment system - in response to chemical or thermal irritations, which leads to the development of an allergic reaction of the body as a whole. In this case, consultation with an allergist will help make the correct diagnosis and decide on treatment.
How are angioedema classified?
Angioedema is divided into subgroups:
Based on the clinical picture:
- The course of the disease has: an acute period, which lasts up to 6 weeks, and a chronic period - more than 6 weeks;
- The disease can be combined with urticaria, or it can be isolated.
Various development mechanisms:
It can be hereditary or acquired.
Hereditary angioedema is always isolated and comes in three types:
- Type 1 – there is an absolute deficiency of the C1 inhibitor;
- Type 2 – there is a relative deficiency of the inhibitor in the body;
- Type 3 – no lack of inhibitor.
Acquired edema:
Acquired C1 inhibitor deficiency can be divided into the following types:
- absolute (isolated Quincke's edema).
- relative angioedema with the formation of autoantibodies to the inhibitor.
Idiopathic (may be combined).
Other mechanisms are involved in the development of the disease.
- May be associated with autoimmune diseases (may be combined).
- Isolated angioedema, which occurs under the influence of angiotensin-converting enzyme inhibitors.
- Quincke's edema can occur against the background of focal infection.
- Determined by hypersensitivity to various foods, medications, insect bites (often combined with urticaria).
What forms of angioedema exist?
HAE – hereditary angioedema
HAE (hereditary angioedema) is a dominant autosomal disease. It is characterized by the irregular occurrence of angioedema in any area of the body. This complement-dependent angioedema accounts for no more than 2% of all cases.
It is very important to diagnose the disease in a timely manner using a screening test. If the values are normal, the patient does not have HAE. This happens in 96% of cases: in this case, there is no need for further diagnosis.
Angioedema can be caused by ACE inhibitors: the disease develops from the first days of use and continues to worsen over several months of regular use of the drug. Foci of Quincke's edema can appear in the area of the tongue, lips, larynx, neck, and pharynx. In some cases, intestinal edema develops, without any special external manifestations on the skin and visible mucous membranes, but accompanied by abdominal pain.
Prevention of angioedema, which is caused by ACE inhibitors, consists of complete abstinence from taking all drugs of this class. Patients need consultation with an allergist; in addition, they must always have with them a bracelet or document informing them about the disease and the specifics of treatment.
PAO – acquired angioedema
Patients may also experience acquired C1 inhibitor deficiency. In this case, the clinical picture of the disease does not include a burdened hereditary history, and the disease begins to manifest itself after 40 years. Against the background of the immunodeficiency virus, acquired complement-dependent edema of lymphoproliferative diseases, multiple myeloma, chronic hepatitis B and C can occur. PAO often appears several years before the onset of the underlying disease.
What symptoms are characteristic of Quincke's edema?
The main symptom is limited and painless swelling of the mucous skin, the membrane of subcutaneous adipose tissue, which causes a feeling of distension of the skin. The disease can occur spontaneously or under the influence of triggers - provoking factors (stress, trauma, acute viral infection, surgery, alcohol, ACE inhibitors, estrogen drugs).
Quincke's edema can begin unexpectedly. Within a few minutes, swelling appears, with sharply defined borders of a pale color. The size of the swelling can vary: from a coin to a child’s palm; it can last for several hours and then disappear without a trace.
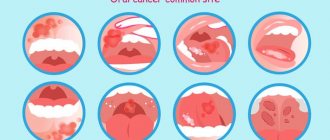
Quincke's edema often occurs in the area of the tongue, eyelids, lips, ears, soft palate, hands, feet, and genitals. Some people (no more than 25%) experience swelling of the trachea, larynx and large bronchi: it is characterized by hoarseness, a feeling of lack of air and a “barking cough”.
The patient experiences only skin tension in the area of edema: there are no other sensations, not even itching. But when pressed, a hole does not appear. Quincke's edema can occur with typical urticaria rashes. The appearance of edema in the bladder mucosa can lead to difficulty urinating, and in the intestinal mucosa - to abdominal pain.
Swelling of the trachea, pharynx, and larynx is the most dangerous and is observed in every fourth case. Characteristic features are: sudden anxiety, aphonia, difficulty breathing, hoarseness, and in some cases even loss of consciousness. During examination of the mucous membrane of the throat, swelling of the palatine arches and soft palate can be observed, the lumen of the pharynx narrows, and there may be a threat of acute lack of air - asphyxia. In this case, emergency medical intervention is required.
How can angioedema be diagnosed?
To clarify the diagnosis, it is important to consult an allergist, and an experienced immunologist will tell you what needs to be taken so that allergy treatment is systemic. It is imperative to identify the factors that provoke the onset of the disease. For example, you need to find a connection with taking some medications, foods, etc. This connection can be further confirmed using allergic skin tests.
It is necessary to evaluate a general blood test, urine test, determine functional activity and the level of C1 inhibitor, conduct allergy tests, clarify biochemical blood parameters, levels of C4, C1q and C2 components of the complement system. In this case, it is necessary to exclude intestinal diseases, autoimmune diseases, blood diseases, and conduct stool tests for helminths.
What is needed to treat angioedema?
Treatment of the hereditary form of angioedema is impossible without medications that are prescribed to enhance the body’s production of the missing inhibitor (currently not yet registered in Russia). The main task is to identify the root cause of the disease and eliminate it.
For treatment you can use:
- attenuated androgens;
- tranexamic acid;
- fibrinolysis inhibitors;
- fresh or fresh frozen aminocaproic plasma;
- various diuretics.
If the patient is diagnosed with idiopathic angioedema (with an unknown cause), it is necessary to use modern antihistamines for a long time. The choice of one of the antihistamine non-sedative drugs will be influenced by a consultation with an allergist, at which the patient’s individual characteristics and reaction to the new generation drugs will be determined.
The use of antileukotriene drugs may be necessary. If a severe course of the disease is initially diagnosed, it is necessary to use GCS, gradually reducing the dose to the minimum effective. If after using all of the above treatment methods there are no positive results, you can perform blood plasmapheresis, treatment with cyclosporine, use hydroxychloroquine, sulfasalazine, thyroxine, warfarin, methotrexate.
How to properly prevent the disease?
If the cause of angioedema is a drug or food allergy, you will need to consult an allergist, at which the specialist will recommend avoiding foods or medications that cause swelling.
All patients with HAE need to be treated for emerging foci of chronic infections, because with their exacerbation, the development of angioedema may occur. It is also advisable to exclude the use of oral contraceptives that contain estrogens, ACE inhibitors, including plasminogen activators.
Specialists at the Gorbakov Clinic advise following a strict diet (excluding all allergens), eliminating allergens from the patient’s environment, and taking preventative antihistamines during contact with various allergens or when plants are blooming.
Experienced allergists and immunologists at the Clinic will conduct professional diagnostics and prescribe adequate treatment, after which you can quickly and safely get rid of the symptoms of the disease and return to your usual way of life.
Quincke's edema is an allergic disease that is characterized by lightning-fast development and an increase in symptoms. Angioedema can affect any part of the body, which naturally causes significant inconvenience to patients. If you have ever experienced similar symptoms, or anyone in your family has suffered from angioedema, we recommend that you immediately seek advice from an allergist-immunologist, who will select the optimal course of treatment or recommend preventive measures.
First aid
If signs of Quincke's edema appear, you should immediately call a doctor. Before the ambulance arrives, the patient is given first aid, which includes the following actions:
- eliminating the allergen (for example, if it is an insect bite, then you need to remove the sting);
- ensuring the supply of oxygen to the room where the victim is located;
- calming the patient;
- release from tight clothing, belt, tie;
- removing the allergen using copious amounts of water and taking sorbents (activated carbon);
- instillation of vasoconstrictor drops into the nose;
- applying a cold compress to the affected area. If the cause of swelling is an insect bite or injection of a medication, a tourniquet is recommended;
- taking an antihistamine.
Emergency care for Quincke's edema is accompanied by the following measures:
- detoxification;
- hormone therapy (administer prednisolone intravenously or intramuscularly);
- desensitizing therapy (intramuscular injection of suprastin);
- use of diuretics;
- protease inhibitors.
Of course, the patient needs urgent hospitalization in the allergology department. Quincke's edema, especially its severe forms, is a condition that requires urgent professional help. In some cases, minutes count.
Make an appointment online
Sign up
Symptoms of angioedema / Quincke's edema
Angioedema (other names: Quincke's edema, giant urticaria, acute angioedema) is trophoneurotic edema. The disease may be hereditary or acquired. It is characterized by the appearance of swelling of the subcutaneous fatty tissue and deep layers of the skin, including the mucous membranes of all organs and systems (digestive, respiratory, urinary and others). Angioedema may persist for 72 hours.
The disease can have a hereditary form (about 25% of all cases). The idiopathic variant occurs in approximately 30% of patients. In this case, it is not always possible to establish the true cause of the disease. In all remaining cases, Quincke's edema occurs when:
- drug allergies;
- insect bites;
- food allergies;
- helminths and protozoa;
- autoimmune diseases;
- blood diseases.
In some cases, swelling is also called huge urticaria. According to statistics, angioedema occurs in both adults and children, but in most cases the disease occurs in women at a young age. It occurs less frequently in older people and infants. This problem occurs at least once in a lifetime in 10% of the population.
When a specific allergen enters the body, a strong allergic reaction occurs, in response to which Quincke's edema develops. Concomitant diseases may include bronchial asthma and food allergies.
In patients with pseudoallergic edema, the body can react quickly to the compliment system - in response to chemical or thermal irritations, which leads to the development of an allergic reaction of the body as a whole. In this case, consultation with an allergist will help make the correct diagnosis and decide on treatment.
How are angioedema classified?
Angioedema is divided into the following subgroups.
Based on the clinical picture:
- The course of the disease has: an acute period, which lasts up to 6 weeks, and a chronic period - more than 6 weeks;
- The disease can be combined with urticaria, or it can be isolated.
Depending on the mechanisms of development of angioedema, it can be hereditary or acquired :
- Hereditary angioedema is always isolated and comes in three types:
- Type 1 – there is an absolute deficiency of the C1 inhibitor;
- Type 2 – there is a relative deficiency of the inhibitor in the body;
- Type 3 – no lack of inhibitor.
- absolute (isolated Quincke's edema).
- relative angioedema with the formation of autoantibodies to the inhibitor.
With the participation of other mechanisms:
- May be associated with autoimmune diseases.
- Isolated angioedema occurring under the influence of angiotensin-converting enzyme inhibitors.
- Quincke's edema due to focal infection.
- Determined by hypersensitivity to various foods, medications, insect bites (often combined with urticaria).
What forms of angioedema exist?
HAE (hereditary angioedema) is a dominant autosomal disease. It is characterized by the irregular occurrence of angioedema in any area of the body. This complement-dependent angioedema accounts for no more than 2% of all cases.
Angiotensin-converting enzyme inhibitors can cause angioedema: the disease develops from the first days of use and continues to worsen over several months of regular use of the drug. Foci of Quincke's edema can appear in the area of the tongue, lips, larynx, neck, and pharynx. In some cases, intestinal edema develops, without any special external manifestations on the skin and visible mucous membranes, but accompanied by abdominal pain.
Prevention of angioedema, which is caused by ACE inhibitors, consists of complete abstinence from taking all drugs of this class. Patients need consultation with an allergist; in addition, they must always have with them a bracelet or document informing them about the disease and the specifics of treatment.
Patients may also experience acquired C1 inhibitor deficiency – acquired angioedema (PAO). In this case, the clinical picture of the disease does not include a burdened hereditary history. Against the background of the immunodeficiency virus, acquired complement-dependent edema of lymphoproliferative diseases, multiple myeloma, chronic hepatitis B and C can occur. PAO often appears several years before the onset of the underlying disease.
What symptoms are characteristic of Quincke's edema?
The main symptom is limited and painless swelling of the mucous skin, the membrane of subcutaneous adipose tissue, which causes a feeling of distension of the skin. The disease can occur spontaneously or under the influence of triggers – provoking factors:
- stress;
- injuries;
- acute viral infection;
- surgical interventions;
- alcohol;
- ACE inhibitors;
- estrogen drugs.
Quincke's edema can begin unexpectedly. Within a few minutes, swelling appears, with sharply defined borders of a pale color. The size of the swelling can vary: from a coin to a child’s palm; it can last for several hours and then disappear without a trace.
Often with Quincke's edema, swelling occurs in the area of the tongue, eyelids, lips, ears, soft palate, hands, feet, and genitals. Some people (no more than 25%) experience swelling of the trachea, larynx and large bronchi: it is characterized by hoarseness, a feeling of lack of air and a “barking cough”.
The development of edema is most often not accompanied by itching, but sometimes, especially if the edema is associated with urticaria, itching may be the first sign and accompany the development of the allergic process. Quincke's edema can occur with typical urticaria rashes. The appearance of edema in the bladder mucosa can lead to difficulty urinating, and in the intestinal mucosa - to abdominal pain.
Swelling of the trachea, pharynx, and larynx is the most dangerous and is observed in every fourth case. Characteristic features are: sudden anxiety, aphonia, difficulty breathing, hoarseness, and in some cases even loss of consciousness. During examination of the mucous membrane of the throat, swelling of the palatine arches and soft palate can be observed, the lumen of the pharynx narrows, and there may be a threat of acute lack of air - asphyxia. In this case, emergency medical intervention is required.
Classification
Based on the root cause of the disease, in medicine there are 2 types of edema:
- allergic type, which occurs due to the influence of a food, chemical or medicinal allergen on the human body);
- pseudo-allergic. This type is associated with a hereditary predisposition.
A group of scientists identifies a separate third type – idiopathic. This form of pathology has not yet been fully studied.
Quincke's edema in children is most often associated with genetics. The disease is accompanied by urticaria, nausea, vomiting, fever, and sometimes even loss of consciousness.
The main thing that needs to be done is to eliminate the causes of angioedema in order to avoid the development of complications, including death. The main danger is that a child at an early age cannot correctly explain his own condition. That is why the task of parents is to constantly monitor the baby. At the first signs of illness, the appearance of cyanosis or difficulty breathing, you should immediately contact a specialist.
Diagnosis of Quincke's edema / angioedema
To clarify the diagnosis, it is important to consult an allergist, and an experienced immunologist will tell you what needs to be taken so that allergy treatment is systemic. It is imperative to identify the factors that provoke the onset of the disease. For example, you need to find a connection with taking some medications, food, and so on. This connection can be further confirmed using allergic skin tests.
It is necessary to evaluate using special tests:
- general blood and urine analysis;
- determine the functional activity and level of C1 inhibitor;
- carry out allergy tests;
- to clarify biochemical blood parameters, levels of C4, C1q and C2 components of the complement system.
In this case, it is necessary to exclude intestinal diseases, autoimmune diseases, blood diseases, and conduct stool tests for helminths.
Complications
If measures are not taken in time, the consequences of Quincke's edema can become life-threatening. This applies, first of all, to damage that affects the mucous membrane of the larynx, as well as the meninges with symptoms of meningitis. These complications in most cases lead to the death of the patient.
With angioedema, anaphylactic shock often develops. This reaction is extremely life-threatening and affects the functioning of the entire body. Its main symptoms:
- swelling of the oropharynx, larynx and tongue;
- generalized itching;
- hives;
- bronchospasm, lacrimation;
- nausea, vomiting, diarrhea;
- tachycardia, hypotension, arrhythmia, acute heart failure;
- convulsions, suffocation, coma.
Treatment of Quincke's edema / angioedema
Treatment of the hereditary form of angioedema is impossible without medications that are prescribed to enhance the body’s production of the missing inhibitor (currently not yet registered in Russia). The main task is to identify the root cause of the disease and eliminate it.
To treat angioedema you can use:
- antihistamines;
- hormonal drugs;
- bronchodilators;
- attenuated androgens;
- tranexamic acid;
- fibrinolysis inhibitors;
- fresh or fresh frozen aminocaproic plasma;
- various diuretics.
If the patient is diagnosed with idiopathic angioedema (with an unknown cause), it is necessary to use modern antihistamines for a long time.
The use of antileukotriene drugs may be necessary. If a severe course of the disease is initially diagnosed, it is necessary to use glucocorticosteroids, gradually reducing the dose to the minimum effective. If after using all of the above treatment methods there are no positive results, you can perform blood plasmapheresis, treatment with cyclosporine, use hydroxychloroquine, sulfasalazine, thyroxine, warfarin, methotrexate.
How to properly prevent the disease?
If the cause of angioedema is a drug or food allergy, you will need to consult an allergist, at which the specialist will recommend avoiding foods or medications that cause swelling.
All patients with HAE need to be treated for emerging foci of chronic infections, because with their exacerbation, the development of angioedema may occur. It is also advisable to exclude the use of oral contraceptives that contain estrogens, angiotensin-converting enzyme (ACE) inhibitors, including plasminogen activators.
Specialists at the Gorbakov Clinic advise:
- follow a strict diet (exclude all allergens);
- eliminate allergens from the patient’s environment;
- carry out prophylactic intake of prescribed antihistamines during contact with various allergens or flowering plants.
Experienced allergists-immunologists of the Clinic will conduct professional diagnostics and prescribe adequate treatment, after which you can quickly and safely get rid of the symptoms of Quincke's edema and return to your usual way of life.
Causes
Quincke's edema is the body's response to an allergen. The following substances and agents may be the cause:
- toxins and poisons, incl. insects;
- dust;
- animal hair and dander;
- microorganisms - fungi, bacteria and even viruses;
- chemicals such as turpentine and phenol;
- latex products;
- plant pollen;
- medications: anesthetics, bromides, iodine, immunoglobulins, B vitamins, antihypertensives, antibiotics;
- substances contained in eggs, nuts, milk, fish, honey, citrus fruits, strawberries or chocolate;
- food colors, flavors, flavor enhancers, preservatives;
- artificial formula for babies.
Indirect factors that provoke angioedema include endocrine diseases and infection with worms. In people with hereditary allergies, swelling can be triggered by hypothermia or stress. A severe allergic reaction is insidious in that it can develop not during the first contact with the agent, but during the next one.
Prognosis and prevention
To prevent the development of soft tissue swelling, it is important to follow certain rules:
- avoid contact with products and drugs that cause allergies;
- If you have such reactions to certain types of medications, be sure to inform your doctor;
- When taking a new type of antibacterial drug, keep antihistamines on hand;
- eat right;
- follow a gentle diet;
- take vitamin complexes to strengthen the human immune system.
If the cause of swelling is a food allergy, then the diet should be adjusted and selected very carefully. There are a number of foods that are more likely to cause illness:
- strawberries;
- fish;
- eggs;
- seafood;
- citrus;
- strawberry;
- nuts.
If food has become the cause of the pathology, then doctors sharply limit the diet, but such a diet cannot be maintained for a long time. The body must receive the full range of necessary components, so fasting cannot be prolonged.