What is it and how to treat it?
Osteomyelitis is an inflammation of the bone marrow with a tendency to progress.
This is what distinguishes it from the widespread dentoalveolar abscess, dry socket, and osteitis seen in infected fractures. Osteomyelitis affects adjacent cortical plates and often periosteal tissues. In the era of preantibiotics, osteomyelitis of the mandible was not uncommon. With the advent of antibiotics, the disease began to be detected less frequently. But in recent years, antimicrobial drugs have become less effective, and the disease has reappeared.
Features of symptoms
The main noticeable symptom is called pain, but in fact it is far from the first, it’s just that the symptoms of the disease are not obvious at the initial stage. In addition, pain also occurs with all other diseases of the spine, so even with the onset of pain, the infection goes unnoticed for a long time, for months. Patients begin to worry when general intoxication, a feeling of chills, a rise in temperature, increased sweating and weight loss are added to the pain, and the pain begins to manifest itself especially strongly at night.
The most obvious symptom of osteomyelitis is pain against the background of general intoxication and poor health
In accordance with the infecting ability of pathogens, three types of osteomyelitis developing in vertebral structures are distinguished.
- Spicy.
- Primary chronicle.
- Chronic.
Table. Symptoms of osteomyelitis by type.
| ● multi-stage sharp pain, increasing in amplitude at night; | ● mild episodic pain syndromes; | ● mild pain of unclear localization; |
| ● excessive sweating; | ● chills; | ● rises to 37°C, usually in the evening; |
| ● strong rise in temperature to 39°C and above; | ● mild intoxication; | ● pain may intensify at night; |
| ● convulsive conditions; | ● slight temporary increase in temperature; | ● feeling of stiffness of the spine; |
| ● hypotension; | ● increased sweating; | ● sweating; |
| ● swelling of soft paravertebral tissues. | ● general state of lethargy; | ● slight swelling and numbness of the spine. |
| ● vascular tension; | ||
| ● pain in the back muscles. |
By the way. Almost always, patients mistake the primary chronic and stable chronic form for manifestations of osteochondrosis or other vertebral and joint pathologies, or diseases of internal organs such as the lungs and heart.
During its development, osteomyelitis inflames not only the bone tissue, but also spreads to the entire blood supply system in the spine. This can lead to sepsis, disability and death.
Occasionally, the infection involves nerve structures in the inflammatory process by moving into the spinal canal, causing the formation of an epidural abscess. It puts pressure on the nerves, and if the source of infection is located in the neck or chest area, it can result in paraplegia (paralysis of either lower or upper limbs in pairs) and quadriplegia (simultaneous paralysis of all limbs).
By the way. Victims of osteomyelitis most often become older men, especially those who experience frequent stress and excessive tension and have a large number of different diseases. This reduces immunity and makes it impossible to cope with bacteria that cause inflammation.
Victims of osteomyelitis are most often older men
When the disease takes a protracted chronic form, the number of purulent foci in the bone increases and their size also increases. New inflamed tissue may begin to grow, which comes into conflict with healthy tissue and infects it, expanding the area of infection. The bone marrow does not remain aloof from the inflammatory process, since the accumulating pus interferes with the normal functioning of the blood cells that provide it with nutrition.
Osteomyelitis of the jaw. Causes
In the maxillofacial region, osteomyelitis occurs mainly as a result of the continuous spread of odontogenic infections or as a result of trauma. Primary hematogenous osteomyelitis in the maxillofacial region is rare, usually in very young people. Thus, osteomyelitis of the jaw occurs after tooth extraction, root canal treatment, or with fractures of the upper or lower jaw. This initial lesion leads to an inflammatory process caused by bacteria.
The incidence of osteomyelitis is much higher in the mandible due to the dense, poorly vascularized cortical plates and blood supply. Osteomyelitis of the maxilla is much less common due to the excellent blood supply from several feeding vessels. In addition, the maxillary bone is less dense than the mandibular bone.
Reduced patient protection, both local and systemic, may significantly contribute to the development of osteomyelitis. Osteomyelitis can be associated with a variety of systemic diseases, including diabetes, autoimmune conditions, malignancies, malnutrition, and acquired immunodeficiency syndrome. Medicines associated with the risk of osteomyelitis: steroids, chemotherapy drugs, bisphosphonates. Radiation therapy (causes so-called radiation osteomyelitis of the jaw), osteoporosis and bone pathology can change the blood supply to this area and become a potential springboard for the development of osteomyelitis.
Vertebral infection
Not so long ago, this disease was considered incurable, since it was impossible to remove the infection from the skeletal system. Today, the process is successfully stopped through an operation during which infected tissue is removed, associated with intensive antibacterial drug action.
Spinal osteomyelitis is treated surgically
By the way. Osteomyelitis often occurs in children, affecting the bones in the legs and arms. Adults mainly suffer from an inflammatory process localized in the bones of the spine. In some cases, if an adult patient has diabetes, the process begins to develop from the lower extremities, if there are trophic ulcers on them.
Infection of the vertebrae cannot be considered a common cause of back pain, especially if the patient is young and, in principle, healthy. But cases of the disease are becoming more frequent, and osteomyelitis (the second name is spondylitis) is gradually becoming an urgent problem.
By the way. The most common route of infection into the vertebral segments is hematogenous, which is carried out through the bloodstream. In some episodes of infection, microbes appear in the vertebrae after various medical diagnostic procedures, such as urological cystoscopy.
Etiology of causes of osteomyelitis
To understand how bone tissue becomes infected, it is necessary to remember how the blood supply occurs in the spine.
Initially, the body of each vertebral segment is isolated from the rest by a cartilaginous intervertebral septum. But along the ridge there are arteries that branch from the neck and carry blood to all vertebral tissues, and, of course, through the vascular network, to the vertebrae. The lumbar zone receives nutrition with blood passing through the arterial canals of the lumbosacral zones. Each vertebra is entangled with venous vessels that connect to form veins.
Blood supply to the spinal cord
In this way, viruses can penetrate the vertebra through both veins and arteries. As soon as the pathogens find themselves in the bone tissue, the inflammatory stage is activated, during which it dies.
Accumulating obsolete microorganisms that are not removed in a timely manner form purulent accumulations in the spinal tissue. The outer vertebral membrane is destroyed, and the process spreads to other parts of the spinal column.
Who is at risk
Bone tissue is designed to be resistant to infection. Therefore, for osteomyelitis to begin, additional factors contributing to the development of the disease are necessary. These factors weaken bone tissue, increasing its vulnerability and reducing resistance to infection.
- Injuries accompanied by bone fractures, when infection can easily be introduced into the vertebra both by the bloodstream and by the tissue located next to the fracture.
- An operation to reposition bone fragments or a deep puncture was performed.
- Impaired blood circulation in the event that blood vessels are damaged or the blood flow is unstable. A deficiency of immune cells occurs, which reduces the ability to resist infection.
- Disease diabetes mellitus.
- Weakening and pathology of peripheral arteries, which may be associated with smoking.
- Infections.
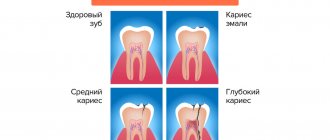
- Deep carious dental lesions.
- Hereditary hemoglobinopathy expressed by sickle cell anemia.
- Placement of a dialysis or medical catheter.
- Intravenous drug use.
Causes of osteomyelitis
By the way. Despite the fact that catheters are absolutely necessary in various situations - dialysis, emptying the bladder, administering medications into veins for a long time - they carry perhaps the highest risk of unsterility and possible infection.
Greatest risk of infection during catheterization
Based on this, there are groups of patients who are most susceptible to osteomyelitis:
- elderly people;
- patients with drug addiction;
- people whose immune systems are weakened.
Drug-dependent individuals are most at risk of contracting osteomyelitis
Long-term use of corticosteroids for rheumatoid arthritis and other diseases, diabetes accompanied by insulin dependence, AIDS, people who have received organ transplants, suffer from malnutrition, and have cancer - all these patients have reduced immunity and an increased ability to resist infection at the bone-cellular level.
Osteomyelitis of the jaw. Symptoms
Like any infection of the maxillofacial area, osteomyelitis of the lower jaw and osteomyelitis of the upper jaw are accompanied by symptoms:
- pain
- swelling and redness on the surface of the skin
- adenopathy
- heat
- paresthesia of the inferior alveolar nerve
- lockjaw
- malaise
- fistulas
Pain from osteomyelitis is often described as deep and aching, which often does not correspond to the clinical picture.
In acute osteomyelitis, swelling and erythema of the overlying tissues are very often observed, which indicate the initial phase of the inflammatory process in the underlying bone.
Fever often accompanies acute osteomyelitis, whereas it is relatively rare in chronic osteomyelitis.
Inferior alveolar nerve paresthesia is a classic sign of pressure on the inferior alveolar nerve as a result of an inflammatory process in the bone marrow of the mandible.
Trismus may be present due to an inflammatory reaction in the muscles of mastication.
The patient usually experiences malaise or a feeling of general weakness, which can accompany any systemic infection.
Finally, both intraoral and extraoral fistulas are usually present in the chronic phase of maxillofacial osteomyelitis.
Osteomyelitis - what kind of disease
Osteomyelitis of the jaw is an infectious and inflammatory process characterized by spread to the bone tissue of the jaw and bone marrow. When a purulent process occurs, the disease turns into the form of necrosis.
The exact etiology of the disease has not been determined. Pathology occurs when a pathogen is active, which can be either an internal infection present in a healthy body or an infection that has penetrated from the outside.
Osteomyelitis has symptoms:
- fever, weakness, chills;
- mobility of teeth in the area of infected bone;
- formation of fistulas on the gums and face in the jaw area;
- pain in the affected area;
- restriction of jaw movement;
- inflammation of the soft tissues on the face.
Depending on the form of the disease, signs of damage may have specific manifestations.
Treatment of osteomyelitis involves detoxification and anti-inflammatory therapy, elimination of the purulent process by drainage, removal of affected tissues and teeth.
Osteomyelitis of the jaw. Diagnostics
Patients are often given laboratory tests as part of their initial evaluation. In the acute phase of osteomyelitis, leukocytosis with a shift to the left is often observed, which is typical for any acute infection. But leukocytosis is relatively rare in the chronic phases of osteomyelitis.
The patient may also have an elevated erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP). Both ESR and CRP are very sensitive. Almost all patients will undergo maxillofacial imaging.
Computed tomography (CT) has become the standard of care in the evaluation of maxillofacial pathology such as osteomyelitis. It provides a three-dimensional image. CT can provide very detailed images of early cortical bone erosion in osteomyelitis. Often, along with pathological fractures, you can see the degree of damage and bone sequestration. CT scanning, like conventional X-ray examination, shows changes when bone demineralization reaches 30 to 50%, which significantly delays the diagnosis of osteomyelitis. Magnetic resonance imaging (MRI) is generally considered more valuable in assessing soft tissue lesions in the maxillofacial region. However, MRI can help in the early diagnosis of osteomyelitis. Thus, MRI can help in identifying the early stages of osteomyelitis.
Osteomyelitis of the jaw. Treatment
The first step in treating osteomyelitis is to correctly diagnose the condition. A preliminary diagnosis is made based on clinical assessment and radiological examination.
Treatment of osteomyelitis of the maxillofacial region requires both conservative and surgical methods. In later stages, antibiotic therapy is rarely effective, so the vast majority of cases of osteomyelitis require surgery.
For osteomyelitis of the upper or osteomyelitis of the lower jaw, as a rule, classical treatment is used - sequestrectomy. The goal is to remove necrotic or poorly vascularized bone sequestration in the infected area and improve blood flow. Sequestrectomy involves removing infected and avascular pieces of bone—usually cortical plates—in the infected area. Visual assessment is critical at these stages, but radiation diagnostics, which shows the osseous extent of the pathology, also helps. It is often necessary to remove teeth adjacent to the area of necrosis.
Supporting the weakened area with a fixation device (external fixator or reconstruction plate) is often used to prevent pathological fracture.
Treatment of spinal infection
As a rule, in the main cases osteomyelitis is treated conservatively. Therapy is carried out with intravenous antibiotics.
Since the disease is primarily caused by the Staphyloccocus bacterium, which is highly sensitive to antibiotics, the intravenous treatment process takes about a month, and then a control two-week course begins, which is administered orally. During the entire period, the patient is prescribed bed rest.
Antibiotics for osteomyelitis
Important! If the infection is of tuberculosis etiology, the patient may take antibiotics for up to a year.
In addition to therapy, the spine is fixed for six to twelve weeks using a rigid corset, until x-rays show positive dynamics of therapy.