During endodontic treatment, a popular practice is to temporarily fill the root canal. As part of this procedure, a special paste is placed inside the canal, which has many healing properties. Such a filling can be applied for either a couple of days or several months, depending on the chosen treatment method. At the end of treatment, the temporary filling is replaced with a permanent one.
The specific period for which a temporary filling is installed is determined by the dentist. Most often, a material with a long duration of action is selected so that the treatment effect is maximum.
In some cases, medicinal pastes can be used in combination with disinfectants and antiseptics. This combination significantly increases the effectiveness of treatment. In addition, these drugs help reduce the risk of infection of soft and hard tissues.
Features of temporary filling with pastes
In the case of a specific degree of development of the disease, the techniques for temporary filling of root canals may differ. This is justified by the peculiarity of the technique used during treatment. In acute forms of the disease, potassium hydroxide is injected into the canal, often without compaction and for a period of 1 to 7 days based on the clinical picture.
The main goal of the procedure is to prevent the appearance of inflammatory processes and harmful microorganisms inside the canal. In case of chronic diseases, the drug is most often administered with compactions for a period of up to 2 months. If necessary, the material used can be periodically replaced until the desired result is achieved. Based on general practice, treatment can last from six months to 1 year, depending on the extent of the disease, as well as the characteristics of the individual patient’s body.
The application of a temporary filling is also aimed at stimulating the processes of regeneration of damaged cells. To do this, the following filling techniques are used:
- the canal is cleaned and prepared, after which paste is placed in it for a period of 7 to 10 days;
- at the end of the period, the old layer of paste is removed and replaced with a new one;
- After a certain time, the manipulations are repeated (the exact timing is announced by the dentist).
To provide a clear picture of the treatment, an x-ray is taken. It must be performed no earlier than 3 months from the date of the patient’s first visit. The fact is that in the first stages of treatment the result can be variable.
X-ray of teeth
At the end of all procedures, restoration of damaged tissue takes about 3-5 years. During this period, it is recommended to follow all the doctor’s recommendations so as not to repeat the next development of the disease.
Modern Moscow dentistry uses potassium hydroxide-based preparations with various antiseptic additives.
Long-term exposure to calcium hydroxide in maxillary anterior teeth (clinical case)
In our dental practice, calcium hydroxide has taken a leading place as medicinal pastes for intracanal therapy only in recent decades, although the use of calcium hydroxide in dentistry has been known since 1838 (Nygren), but this paste has been most widely used in the dental world since 30 years of the last century, with the aim of antimicrobial effects on the microflora of root canals (LRG Fava. WP Saunders. Calcium Hydroxyde pastes: classification and clinical indications. IEJ, 1999). To date, calcium-containing pastes are one of the main drugs in the treatment of infected canals (Ingle's Endodontics 6, Chpt 28, 1009-1010, 2008).
However, in the scientific community there is still no consensus on how long it is possible or necessary to put calcium hydroxide into the root canals. Typically the exposure period is recommended from 1 to 4 weeks. But, works are often published where the exposure period reaches up to 6 months. It seemed like something like that here? Who among us does not have patients who suddenly disappear for six months to a year with calcium hydroxide in the canal, and when we appear we do not find any noticeable exacerbation of the process in them. The inflammatory process either heals during this time, or the temporary restoration we created falls apart and the inflammation persists. In such cases, we blame the failure on failed coronal sealing.
However, among the studies examining prognostic factors affecting the periapical status of the tooth, calcium hydroxide exposure was not even included in the list of prognostic factors. Among such factors, greater importance is still given to the initial periapical status of the tooth and instrumentation with obturation along the entire length of the root canal (NChugal “Endodontics Prognosis”). The additional use of calcium hydroxide adds percentage to the success of treatment (“Reduction of Intracanal Bacteria Using Nickel-Titanium Rotary Instrumentation and Various Medications” G Shuping, D Orstavik 2000 JOE) but is still not able to completely remove the bacterial flora from the root canals (“One-versus Two-visit Endodontic Treatment of Teeth with Apical Periodontitis: A Histobacteriologic Study", Jorge Vera, DDS, Jose F. Siqueira, Jr, DDS, MSc, PhD, Domenico Ricucci, JOE 2014).
In the presented clinical case, a long time investment (more than 6 months) of calcium hydroxide was used in order to obtain sterility of the root canal of tooth No. 11. However, over time, after about six months, the inflammatory process not only did not decrease in size, but repeated exacerbations began to appear. Changes in the root canal treatment protocol, the use of additional irrigants, and an increase in the size of root canal treatment also did not bring any changes to the dynamics of the process. They began to “prepare the patient for resection of the root apex,” additionally “killing” tooth No. 12, since, according to the doctors, curettage of the periapical area could damage its neurovascular bundle.
This patient came to me with approximately the same input data. I decided that perhaps the reason for the failure of the treatment lay in insufficient instrumentation of the root canal of tooth No. 11, so I carried out my chemo-mechanical treatment, increasing the size of the finishing file to ISO 70. Additionally, instrumentation of tooth No. 12 was carried out to size No. 55 according to ISO. However, 10 days after the administration of calcium hydroxide, the tooth worsened the inflammatory process. This became an additional intraoperative factor that reduces the prognosis of treatment (Ng YL, K Gulabivala, T Mann “A prospective study of the factors affecting outcomes of NSRT”, IJE, 2011). Among other factors that negatively affected the prognosis, there was also the factor of the size of the lesion, in particular, according to the study by S Hoskinson (“A retrospective comparison of outcomes of root canal treatment” Oral Patogy Oral Medicine 2002), an increase in the size of the periapical process by 1 mm results in a decrease in success rate by 18%. Therefore, on my part, it was decided to perform apical microsurgery with resection of the apexes of the roots of teeth 11 and 12 after their obturation.
According to the preoperative CBCT analysis, the outer cortical plate of the upper jaw and the lower wall of the nasal cavity were missing, therefore, despite the routineness of the procedure, the curettage process was complicated by perforation into the nasal cavity. This defect was isolated by a biological membrane. The postoperative course was unremarkable. Observations were carried out at 6 and 12 months, after which it was possible to conclude the success of the treatment carried out according to the criteria of the European Society of Society.
Photo report of the work
Video report of the work
Indications for the procedure
Temporary filling of 1 root canal is a standard procedure during endodontic treatment. Among the general indications are the following:
- significant damage to the root canal is observed (most often due to the chronic form of pulpitis);
- the purulent stage of pulpitis was diagnosed (location does not matter);
- there are serious damage to intraradicular soft tissues.
First of all, the patient will have an x-ray to analyze the working length of the root canals, as well as the possibility of carrying out the procedure.
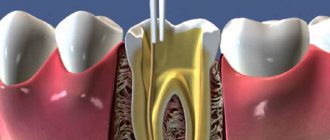
To begin treatment, it is necessary to carry out instrumental treatment, during which the canal acquires the desired shape. At the end of the mechanical manipulations, the funnel-shaped canal is directly treated.
During treatment, various types of pastes can be used. It all depends on the characteristics of the disease, the extent of infection, and the patient’s preferences.
What is calcium filling?
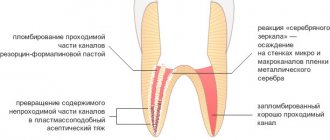
For filling, a special composition is used - copper-calcium hydroxide. It has the consistency of a paste, which is injected into the recess with a special tool - a channel filler.
Calcium hydroxide paste completely closes the canal, preventing pathogens from getting inside
To ensure that there are no voids left in the cavity, the tooth is lightly exposed to electric current.
This method performs a therapeutic function: it disinfects tooth tissue, killing bacteria.
The patient walks with this calcium filling for some time. Then the dentist takes it out, rinses it, thoroughly dries the root canal and performs the final filling with a permanent filling.
Types of pastes
One of the most popular drugs is a paste based on antibiotics and corticosteroids. Most often, such a paste contains about 3 antibacterial agents with a wide spectrum of action. Such drugs have a complex effect and significantly accelerate the regeneration of damaged tissues. The paste also contains a radiopaque filler. It is necessary for a visual assessment of the quality of channel filling. This paste has an extremely strong effect with a minimal duration of action. The filling is applied for a period of 3 to 7 days.
An equally popular paste is a material based on metronidazole. The peculiarity of this paste is the effective suppression of pathogenic microflora in the root canals. In addition, the unique properties of the drugs used make it possible to stop the destruction of hard and soft tissues, as well as prevent the occurrence of inflammatory processes. Most often, metronidazole paste is used in case of excessive infection of the canals.
Another type of paste is a preparation based on an antiseptic mixture with a long-lasting effect. This material has an extremely strong effect due to a number of antiseptic components. The paste does not harden, but slowly dissolves, enriching the tissue with healing elements. Most often, this material is used to diagnose pulpitis or periodontitis, as well as in case of problems with baby teeth.
The fourth variety is potassium hydroxide paste. This drug ensures the beginning of a highly alkaline reaction, during which all existing bacteria and other harmful microorganisms are destroyed inside the root canal. For severe forms of periodontitis, non-hardening forms of the material are used, which are placed in a specific canal using a special filler. This paste must be changed every 6-8 weeks. The exact frequency is determined individually by the attending physician.
Note that, regardless of the specific category of pastes, it is extremely rare to completely cure damaged tissue in one session. The patient is assigned several sessions, during which the effectiveness of the current treatment process is diagnosed, as well as the need to apply another filling.
Does calcium help maintain teeth in old age?
Yes, in old age, taking calcium supplements helps preserve your teeth. A study was conducted that confirmed this fact. So, two groups of people after 65 years of age took three years in a row: the first took calcium supplements and vitamin D, the second took a placebo (“dummies”). After this, the subjects were observed for another two years. It turned out that in the first group people lost teeth less often than in the second. But this is not due to the fact that calcium makes teeth stronger. Here, the main role was played by strengthening the jaws, and consequently, better fixation of the tooth in the jaw.
Preparation for the procedure
Proper preparation is the most important aspect of endodontic treatment. If you do not provide for all possible nuances, the effectiveness of the procedures may be reduced to zero. Before filling directly, it is necessary, first of all, to thoroughly clean the root canal of any plaque that has formed, and also remove all damaged tissue.
In general, all preparatory actions are quite standard. They are carried out in stages and have the following action plan:
- carious lesions are eliminated, as well as dead tissue (specialized drills are used for this);
- pulp is removed from open canals;
- An x-ray is taken to determine the specific shape and length of the canal;
- The root canal is expanded to the required size using various attachments and other tools.
Please note that strict adherence to all of the above points is the key to effective treatment. If you neglect at least one of these stages, with a high degree of probability the current situation will only worsen.
How is canal filling done with paste?
Proper filling of root canals promotes a speedy recovery without any complications. To do this, it is necessary to use proven and high-quality drugs, as well as sterilized dental instruments. Only a highly qualified doctor can perform the procedure correctly, so we recommend contacting only reputable dental clinics.
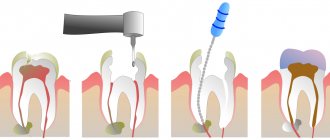
Filling is performed in stages with a clear sequence of actions:
- All affected tissue is removed. In some cases, the practice is used to remove healthy tissue in order to gain unhindered access to each section of the canal.
- Pulp extraction.
- Channel length analysis. Note that the length of the canals varies; the root and its bends play a special role in this matter.
- Mechanical processing of channels. The channels are carefully processed along their entire length to create the maximum possible space. If this is neglected, the material will not be able to spread throughout the entire volume of the channel.
- Canal filling with gutta-percha. The last stage of work. Its effectiveness will directly depend on the correct measurement of the channel length, as well as on the quality of the machining.
Tooth hurts after root canal filling
Dental clinic patients are often concerned about the question of why their tooth hurts after inserting filling material into the tooth canal after removal of the nerve. Since any intervention in the body has its consequences, toothache is an “echo” of the filling procedure.
The most common reasons for a tooth to ache after root canal filling are:
- burns and overdrying of dentin;
- allergic reaction to filling material;
- depressurization of the seal;
- change in bite;
- exposure to polymerization lamps;
- shrinkage of the filling.
After the procedure, the dentist usually advises you on how long the tooth under the filling hurts. However, if you feel increasing pain in a filled tooth for more than 2 weeks, you should urgently consult a doctor. Such pain can occur when an instrument breaks off in the canal, root perforation, or improper treatment of pulpitis.
What can pain after filling indicate?
In this case, the degree of pain plays a key role. Minor discomfort for several days after the procedure is a completely natural consequence. This happens due to irritation of the tissues and pulp, so there is nothing wrong with it. In addition, the patient may experience a feeling of some swelling inside the tooth, which is also normal.
Another thing is severe pain, which can be accompanied by hemorrhages in the oral cavity. This indicates the presence of a serious error during the filling. In this case, it is necessary to contact a dental clinic as soon as possible for an examination.
In general, to avoid unpleasant consequences, we recommend following the standard rules:
- do not expose your teeth to excessively cold temperatures, especially after drinking hot drinks;
- maintain oral hygiene;
- regularly brush your teeth both at home and in the clinic (professional ultrasonic cleaning, etc.);
- undergo routine dental checkups;
- do not neglect your doctor's advice.
Following these simple recommendations will help maintain healthy teeth for a long time.
Beneficial properties of calcium
Preparations containing calcium have an antibacterial effect. Most dental diseases are caused by bacteria that actively multiply in an acidic environment. But an alkaline environment, on the contrary, kills them.
Calcium helps create an alkaline environment in the tooth cavity that is unsuitable for bacterial activity.
To obtain a filling paste, calcium hydroxide powder is diluted with saline solution. Interaction with liquid leads to the release of hydroxyl ions, which kill pathogenic bacteria.