Is it possible to swallow phlegm in the throat?
The accumulation of mucus in the throat forces the patient to pay attention to it.
There are only two options: expectoration or swallowing. Both processes are physiological. Swallowing is harmless: sputum passes into the stomach and is broken down into components. Enzymes in the gastric juice transform mucus into water, which returns to the body and brings only benefits. Harmful components are digested and excreted naturally.
The feeling of mucus in the throat due to hypersecretion of the glands of the respiratory system is normal. These nerve endings signal stagnation of phlegm. The main thing is the absence of suffocation, which is a dangerous sign of the development of events: swelling of the larynx with a threat to life.
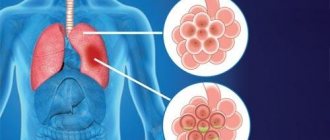
Sputum in the lungs by composition
Why is the formation of fungus in the maxillary sinus dangerous?
How can the growth of a fungal colony be dangerous? In any case, it’s not very pleasant when some kind of parasite, mold, or fungus lives in you. This is really a parasite that lives in the cavity of the maxillary sinus and feels great there. In addition, mycetoma is dangerous because the blood supply and oxygen supply to the brain deteriorates, since the function of nasal breathing is disrupted. A person simply begins to experience partial oxygen starvation due to mycetoma.
Plus, the waste products of the fungus in the maxillary sinus flow into the nasopharynx, which can additionally lead to additional complications, including the development of allergies and provoking respiratory diseases. And, of course, chronic sinusitis.
The role of CT in the study of mycetoma
Of course, a good computed tomogram gives a complete picture of the maxillary sinuses and is the main tool in diagnosing “mycetoma” when examining a patient. A CT scan of the maxillary sinus shows the location, size, and volume of mycetoma damage (local volume or total fungal infection of the cavity).
In fact, computed tomography is the gold standard for diagnosing mycetoma today.
Coughing up white mucus without coughing
Enveloping the larynx with white mucus without a reflexive attempt to remove it is a common reason for patients to see a doctor. Most often, this is pure physiology, not dangerous to health: unfavorable ecology, food irritating the mucous membranes, alcoholic drinks.
If, in addition to sputum, cold symptoms appear: runny nose, headache and fever, this is a reason to consult a doctor.
Most likely, acute respiratory infections provoked an exacerbation of a latent process, which is localized in the upper respiratory tract and does not manifest itself in anything other than hypersecretion of mucus. The pathology does not descend into the bronchi, so there is no cough. But such “innocence” may hide tumors of the nasopharynx, so consultation with a specialist is necessary.
For prevention purposes, any expectoration of white mucus without coughing for a couple of days is a reason to visit a therapist.
An examination with special equipment and a series of tests will allow you to determine the true cause of hypersecretion and prescribe therapy or send you to a specialized specialist.
Symptoms during the formation of mycetoma
In the early stages, a patient with mycetoma feels absolutely nothing, because there are no symptoms of the disease yet.
And as the fungal growth increases in size, it will become more difficult for the patient to breathe due to nasal congestion on one side, while the nose will be clean, without discharge. But sometimes the discharge can be in the form of crumbly masses of a gray-dirty color. In addition to the symptoms listed earlier, the patient may experience dizziness, headaches, when the mycetoma grows strongly, it occupies the entire volume of the maxillary sinus, creating excess pressure, including in the orbital area. And, of course, with a large growth of mycetoma of the maxillary sinus, sinusitis is possible. The patient may have pain in the upper teeth in the lateral part from the side of the mycetoma. And, as I said earlier - difficulty breathing, the patient switches to mouth breathing as a result of acquired chronic sinusitis.
How extensive can a mycetoma be?
Molds can grow until the maxillary sinus is completely filled. And when the mold ball occupies the entire maxillary sinus (it usually takes 5-7 years to grow), the diameter of the ball reaches an average of 3-5 centimeters.
For example, here is a photo of a mycetoma of the maxillary sinus, when the growth of fungi has almost completely “captured” it. The cause of the formation of mycetoma in this case was a part of the root filling of the tooth that was removed into the maxillary sinus:
We describe in detail how the root filling got into the maxillary sinus in this clinical case.
Other reasons
If sputum accumulates in the throat due to allergies, then you should take antihistamines (Suprastin, Cetirizine, Loratadine, Tavegil). Relief should occur within the first day of using them. If the symptom is caused by reflux and reflux of stomach contents, then treatment is prescribed by a gastroenterologist.
It will be individual for each patient (with the use of enzymes, anti-inflammatory drugs and dopamine receptor blockers).
You will also be interested in:
- How to treat a dry cough in an adult that lasts for a long time without fever
How is endoscopic septoplasty performed?
The essence of the operation is to excise those areas of bones and cartilage that have been deformed. The mucous membrane is not subjected to excision, since it is pre-exfoliated, which allows its integrity to be preserved and the rehabilitation period to be significantly reduced.
Modern medicine allows surgical intervention to be performed in an extremely gentle way, so in most cases only that part of the septum that is deformed and causes discomfort is excised.
The operation is performed using an endoscope. During the intervention, a thorough examination of the deformed area is performed. The necessary areas are removed using low-traumatic microtools. The operation is monitored using an endoscope.
Causes caused by pathological processes
Green sputum without cough is always the cause of an infectious disease. It can form or accumulate in the throat with the following pathologies:
- pharyngitis (inflammation of the larynx);
- rhinitis (inflammation of the nasal mucosa);
- nasopharyngitis (inflammation of the nasopharynx);
- bronchial or pulmonary diseases (usually chronic);
- tonsillitis (inflammation of the tonsils);
- allergy.
Most often, the feeling of phlegm in the throat occurs in people who suffer from laryngopharyngeal reflux or esophagitis.
Mucus drains from the nose down the back of the throat. Or it is thrown from the lower respiratory tract, esophagus. Irritation that occurs inside the pharynx increases the formation of sputum.
Viral and bacterial diseases that cause excess mucus in the throat are often accompanied by elevated body temperature. When fluid comes back from the esophagus, there is an unpleasant taste in the mouth.
Why choose Elena Malysheva Medical Center?
When choosing a doctor and a clinic for septoplasty, it is necessary to establish a trusting contact between the specialist and the patient. World-class doctors work at Elena Malysheva’s clinic. Dmitry Semenovich Gorin is a certified ENT doctor who has practiced in famous institutions in the USA (Ear, Nose and Throat Institute in New York) and Germany (University of ENT Diseases).
Dmitry Semenovich works with both adult patients and children. Having extensive practical experience behind him, Dr. Gorin performs ENT operations at the highest level. Thanks to the coordinated work of the entire medical center, preliminary diagnosis and basic treatment are carried out with a high degree of efficiency. The modern equipment used allows endoscopic septoplasty to be performed in a gentle manner, reducing the duration and intensity of rehabilitation.
Swelling after surgery persists for a week, and you can start working in 10-14 days.
Endoscopic septoplasty is a gentle surgical method that will solve your breathing problem. Elena Malysheva's clinic will free you from problems and allow you to freely take a deep breath through your nose!
More detailed information and registration by phone: 8.
Possible causes of sputum without cough and additional symptoms
Sputum is mucus that is secreted by glandular cells of the trachea, nasal cavity, paranasal sinuses and bronchi. Normally, no more than 100 ml of mucus accumulates in the tracheobronchial tree per day. It has bactericidal properties and is involved in the removal from the respiratory tract:
- dust;
- allergens;
- pathogenic agents.
When the mucous membrane is irritated, the activity of glandular cells increases 10 times or more.
Therefore, in case of illness, up to 4 liters of pathological sputum are produced per day. Expectoration of mucus without coughing is a nonspecific symptom that accompanies pathologies of various systems:
- respiratory;
- digestive;
- endocrine;
- nervous.
To find out the cause of the condition, you need to determine:
- the nature of sputum - elasticity, transparency, color, smell;
- associated symptoms – chest pain, sore throat, burning sensation in the nose;
- factors that provoke exacerbation are strong odors, physical activity, drinking hot drinks, etc.
Expectoration of mucus without coughing in half of the cases indicates damage to the nasopharynx or bronchopulmonary system.
Sinusitis and rhinitis
Thick mucus is released without coughing in case of inflammation of the nasopharynx and paranasal sinuses. Copious sputum is expectorated in the following diseases:
- The best cough syrup for children from all types
- Rhinitis (runny nose). Inflammation of the nasal mucosa is accompanied by the secretion of viscous mucus. Its transparency and elasticity depend on the form of the disease. An infectious runny nose produces yellow or green mucus. In people with insufficient tone of blood vessels, vasomotor rhinitis occurs, in which a transparent secretion is formed. With atrophic rhinitis, foul-smelling green sputum occurs.
- Sinusitis. When the maxillary sinuses become inflamed, sinusitis occurs, the ethmoid sinuses - ethmoiditis, the sphenoid sinuses - sphenoiditis, and the frontal sinuses - frontal sinusitis. If you cough up white, thick mucus without coughing, the cause of the illness is a viral infection or allergy. With bacterial and fungal inflammation, it acquires a yellow or green tint and an unpleasant odor.
Expectoration of mucus without coughing occurs mainly in the morning, as during the night it flows down the back wall of the throat into the hypopharynx.
Pharyngitis, laryngitis, tonsillitis
Phlegm in the throat without cough in children and adults occurs due to inflammation:
- palatine tonsils – tonsillitis;
- pharynx – pharyngitis;
- larynx - laryngitis.
If the secretion is transparent, this indicates the onset of the disease or the attenuation of inflammation. In the absence of complications, the cough does not bother you, and small amounts of sputum are expectorated. If it becomes thick and green, purulent inflammation is possible.
The release of viscous mucus without coughing after laryngitis is a sign that the inflammation has become chronic.
Reflux esophagitis
If there is no cough, but there is sputum in an adult, the cause may be the reflux of gastric contents into the esophagus - gastroesophageal reflux disease (GERD). Gastric juice contains hydrochloric acid, which irritates the mucous membrane and provokes the production of mucus.
GERD manifests itself:
- heartburn;
- sour taste in the mouth;
- swallowing disorder;
- hoarseness of voice;
- heaviness in the stomach after eating.
GERD is characterized by insufficiency of the esophageal sphincter.
The contents of the stomach enter the esophagus when the body is tilted or in a supine position. Therefore, clear mucus is coughed up after waking up. If you accidentally inhale gastric juice, a spasmodic cough occurs, accompanied by a burning sensation in the laryngopharynx.
Tuberculosis and other lung infections
Viscous mucus accumulates in the respiratory tract during infectious inflammation of the bronchi and lungs. Green sputum occurs when the ENT organs are damaged:
- Koch's bacillus;
- adenovirus;
- Staphylococcus aureus;
- pneumococcus;
- coronavirus;
- measles virus;
- peptostreptococcus;
- pyogenic streptococcus;
- corynebacterium.
Pathogenic microorganisms produce toxins, so signs of intoxication (poisoning) come to the fore:
- weakness;
- lack of appetite;
- headache;
- drowsiness;
- sweating
With viral inflammation, the sputum is clear, with bacterial inflammation it is yellow, and with purulent inflammation it is green.
If there is no cough and mucus accumulates in the bronchi, breathing becomes harsh. When listening with a stethoscope, moist rales are heard in the lungs.
Allergy
Sputum production without coughing is one of the signs of a respiratory allergy. Irritants (allergens) are:
- medicines;
- plant pollen;
- Food;
- fumes from household chemicals;
- dust mites.
Manifestations of respiratory allergies:
- Night cough in children and adults - causes of dry and wet cough, diagnosis and treatment methods
- labored breathing;
- redness of the throat mucosa;
- nasal congestion;
- lacrimation (with hay fever);
- pain when swallowing;
- hoarseness of voice.
Depending on the location of the inflammation, the allergy occurs with or without a cough.
Patients complain of expectoration of clear, viscous sputum, which sometimes becomes glassy. In the absence of treatment, the clinical picture is supplemented by new symptoms - spasmodic cough, shortness of breath, swelling of the mucous membranes.
Bronchitis
With inflammation of the bronchi, the production of bronchial secretions increases 5-7 times. At the initial stage, the cough appears and then disappears. When accumulated mucus irritates the receptors, coughing attacks occur. Without taking mucolytics, she does not expectorate, so wheezing appears in the lungs.
Symptoms of bronchitis:
- malaise;
- hard breathing;
- chest discomfort;
- nasal congestion;
- moderate increase in temperature.
After 2-3 days, the mucus begins to come out abundantly, so a productive cough occurs. It intensifies at night or in the morning, with a sharp change in temperature.
Sjögren's syndrome
Sputum without fever and cough is one of the signs of Sjögren's disease. It is characterized by damage to connective tissue and exocrine glands. Accompanied by sinusitis and tracheobronchitis, separation of rusty sputum.
Symptoms of Sjögren's disease:
- muscle and joint pain;
- dry eyes;
- seizures in the corners of the mouth;
- violation of the act of swallowing;
- prostration;
- dry tongue;
- formation of crusts in the nose;
- enlargement of the parotid glands.
The mucous membrane of the throat dries out and acquires a bright red tint.
If the glands are insufficient, the saliva becomes viscous. Due to dysphagia (impaired swallowing), the patient cannot swallow it. Therefore, there is a feeling of mucus accumulation in the throat.
Inflammation of the adenoids
Sputum without cough in a child appears against the background of adenoiditis. This is the name for inflammation of an enlarged nasopharyngeal tonsil. The adenoids block the nasal passages, so viscous secretions accumulate in the nasal cavity. During sleep, it flows into the throat through the back wall of the pharynx.
Manifestations of adenoiditis:
- night snoring;
- violation of nasal breathing;
- coughing up yellow mucus;
- restless sleep;
- headache;
- elevated temperature.
There is no cough while awake. It occurs in the morning or immediately after waking up due to irritation of the throat by nasal secretions. If left untreated, the Eustachian tube becomes inflamed (eustachitis), so the child complains of decreased hearing acuity and ear pain.
Esophageal diverticulum
An esophageal diverticulum is a saccular bulge in the wall of the esophagus. It manifests itself as dysphagia, bad breath, and a feeling of a lump in the throat. Many people experience hypersalivation - excessive production of saliva, so they complain of copious sputum discharge without coughing attacks.
Associated symptoms depend on the location of the diverticulum. The most striking clinical picture when a protrusion forms in the clavicle area:
- change in voice timbre;
- nausea;
- scratching in the throat;
- expectoration of thin sputum;
- regurgitation of food;
- backflow of mucus from the esophagus into the throat.
Large diverticula put pressure on the respiratory system, causing coughing. It is combined with chest pain and dizziness.
Consequences of smoking
Non-infectious bronchitis is a problem faced by smokers with more than 7 years of experience. Systematic damage to the bronchi by tobacco smoke leads to irritation and inflammation of the mucous membrane, which increases the activity of glandular cells.
Symptoms of smoker's bronchitis:
- rawness in the throat;
- occasional cough;
- mucus department;
- dyspnea;
- hard breathing;
- tachycardia (against the background of coughing attacks).
During the day, sputum passes without coughing. But during sleep, it accumulates in the throat, so in the morning coughing attacks occur, during which clots of transparent mucus are released.
Worm infestation
If a child or adult does not cough up clear or white sputum, the cause may be helminthiasis. In the acute phase, parasite larvae circulate in the blood and enter the bronchi. They irritate the mucous membrane, causing a productive cough. A person complains about:
- chest pain;
- swelling of the mucous membranes;
- shortness of breath;
- nausea.
When the mucus is swallowed, the worms enter the intestines, where they develop into adults. In the later stages, helminthiasis manifests itself:
- abdominal pain;
- unstable stool;
- weakness;
- sleep disturbance;
- elevated temperature;
- convulsions.
With a chronic disease, immunity decreases, so rhinitis, tracheitis, and influenza often recur.
Other reasons
Foul-smelling mucus without coughing is a dangerous symptom that occurs against the background of purulent inflammation of the ENT organs. Without treatment, complications are possible - abscess and gangrene of the lung, sepsis (blood poisoning).
Possible causes of expectoration:
- lungs' cancer;
- pulmonary syphilis, disintegration of syphilitic gum;
- bronchopulmonary carcinoma;
- cystic fibrosis;
- pulmonary mycosis;
- actinomycosis;
- bullous disease;
- pleural empyema;
- COPD
Yellow sputum without cough is a sign of bacterial diseases of the nasopharynx. If clots of dried blood are found in it, this indicates mucopurulent inflammation. Brown sputum in the morning without cough occurs with bronchiectasis and cardiac pathologies.
Breathing with turbulence and friction
Chief, I can hear you
Bronchial breathing is a sound phenomenon that occurs when air turbulence passes through the larynx, and is also the site of the division of the trachea into two main bronchi (tracheal bifurcation). Since zones of turbulence occur both during inhalation and exhalation, bronchial breathing is clearly audible both in the first phase of breathing and in the second.
You've probably noticed that the doctor doesn't listen to the lungs at one point, but strives to poke the stethoscope all over the back, and in young beautiful girls he listens especially intently to the lungs in front. In general, he is not doing this out of a good life, believe me. Our lungs are rather large, and the doctor needs to determine whether the noise is heard over their entire surface or whether it is localized. Is one type of breathing heard everywhere, or is there an alternative somewhere?
A striking example of such an alternative is bronchial breathing. As we have already said, normally vesicular breathing should be heard over the entire surface of the lungs. Let me clarify: almost all of it. Above the larynx, in the projection of the trachea and especially in the projection of its bifurcation - the level of the IV-V thoracic vertebrae (in young beautiful girls - this is right at the very top of the cleavage;)) bronchial breathing is normally heard. Sometimes, to distinguish it from pathological bronchial breathing, it is called laryngo-tracheal breathing. That is, the laryngo-tracheal is somehow the norm, but the bronchial is no longer the norm.
Let me emphasize once again that normally bronchial breathing should not be heard over other parts of the lungs. If it appears somewhere else, it means there is a problem in the lungs. Most often, associated with compaction of the lung tissue (under such conditions, sounds are conducted much better than through air lungs).
Depending on the severity of the process, bronchial breathing may overlap with vesicular breathing, or may completely displace it. What can cause hardening of lung tissue? Pneumonia, first of all. Especially massive, lobar, for example.
In addition to pneumonia, compaction of lung tissue can cause tuberculosis, pulmonary infarction, compression atelectasis of the lung (collapse of lung tissue and compression of the lung to its root), pneumosclerosis (when lung tissue is replaced by connective tissue).
To be fair, it should be noted that bronchial breathing can rarely be heard over the entire surface of the lungs. Most often, it is perfectly audible above the source of compaction, and if you move to the side, its volume drops exponentially. This fact helps the doctor to say with a certain degree of probability where exactly the problem is located.
Amphoric breathing is also a variant of pathological bronchial breathing. It can be heard if a cavity in the lung (5-6 cm in diameter, usually smooth-walled) connects to a bronchus. A cavity can appear, for example, with a lung abscess.
Essentially, we get the Pan Flute element. The air passes over the opening of the cavity - and we hear a fairly loud and somewhat musical sound.
The old professors mentioned more than once suggested taking an empty champagne bottle and blowing over its neck. The sound is almost the same as with amphoric breathing.
It's cold!
Fortunately, quite rarely, there are disturbances in the innervation of the respiratory muscles. With such a pathology, they do not all work at the same time, but one by one, step by step. As a result, we get a stepped inhalation. Our exhalation is passive, muscles are not particularly needed there, so the second phase of breathing is usually not changed.
This type of breathing is called saccoded.
But in the overwhelming majority of cases, saccoded breathing is explained by completely normal and not at all pathological reasons. First of all, the cold. It’s good for the doctor, under his coat he may have not only a fiery heart, but also, for example, a woolen vest. But the patient has no choice, he has to be naked to the waist (from above), even if it is not hot in the office or ward, to put it mildly. The muscles begin to engage in tremulous thermogenesis, resulting in saccoded breathing upon auscultation.
Therefore, it is recommended to examine patients in a more or less warm room. And warm the head of the phonendoscope in your hands before applying it to the patient’s skin. For experienced therapists, this is already at the level of automation: you interview a person, and the stethoscope warms up in your hand.
Another option is people who, when they see a doctor, begin to get terribly worried. And again we hear saccoded breathing. Again, if the patient sobs before the doctor arrives, then for some time he will again experience saccoded breathing. And again, the reason is not illness at all, it’s just the consequences of crying.
Well, to figure out whether it is a violation of the innervation of the respiratory muscles or recent crying - this is precisely the art of the diagnostician.
Noise maker mouse
And now we move on to the most notable noisemaker in the lung area. As you know, our lungs are covered with a kind of elastic film - pleura. And the chest cavity is lined from the inside with the same pleura. Between these two layers there is a small cavity, which is called the pleural cavity. Both leaves are coated with a small amount of lubricant to facilitate breathing movements.
If the pathological process is localized not in the depths of the lungs, but on the surface, the pleura covering the lungs can also become inflamed. In this case, the lubrication can either disappear (as with the rapid loss of a noticeable amount of fluid by the body - cholera, blood loss, indomitable
vomiting and other delights), or fibrin may be deposited on the surface of the pleura, adhesions and scars may occur (tuberculosis, cancer, etc.).
As a result, the sliding of the pleura becomes no longer so easy and carefree. And not so silent.
Pleural friction noise is one of the loudest sound phenomena. Already annoying, the old professors compared it to the crunch of snow on a frosty day. Amazingly accurate definition.
Distinctive features - does not disappear when coughing, is clearly audible both on inhalation and exhalation, if you press with the head of the phonendoscope, the pleural friction noise will intensify. Thus, it can be distinguished from fine moist rales and crepitus. There is another sadistic technique: cover the patient’s mouth and nose and ask him to imitate breathing movements with his stomach, perhaps accompanied by music. The pleural friction noise will remain, but there will be no wheezing or crepitus. The main thing with this technique is to quickly run away after it is completed.
Most often, pleural friction noise is heard in places of greatest amplitude of respiratory movements, that is, from below on the sides. Much less often (with tuberculosis) it can be detected in the area of the apexes of the lungs